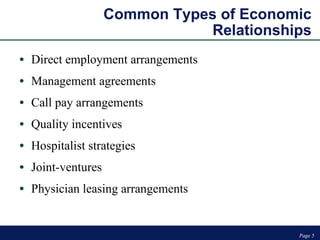
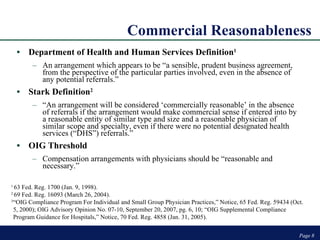
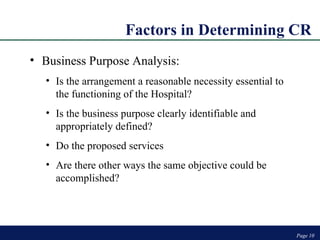
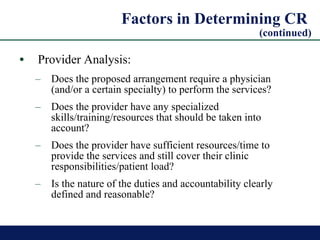
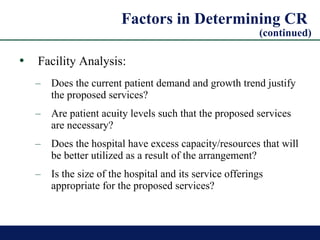
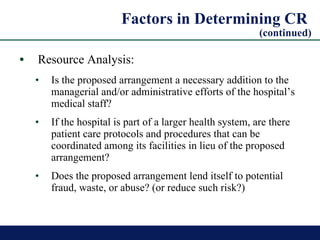
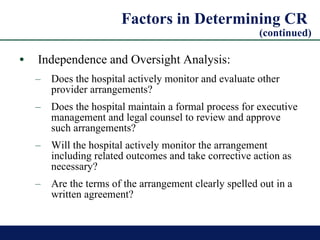
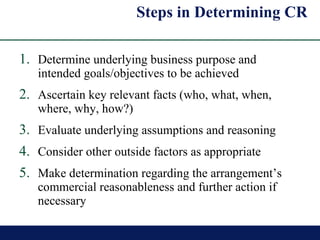
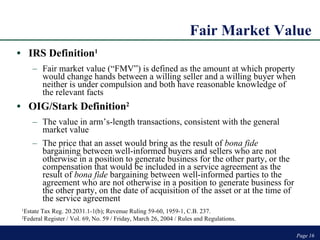
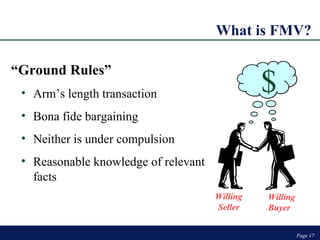
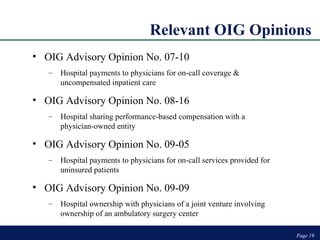
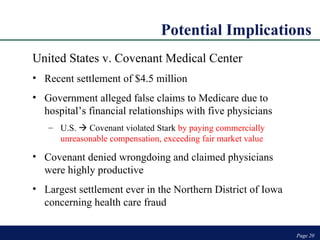
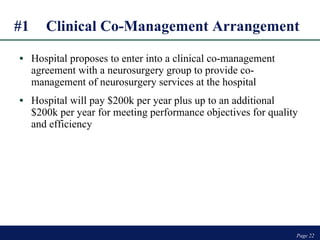
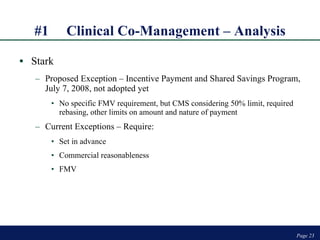
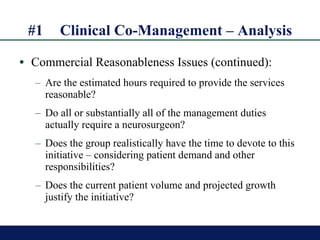
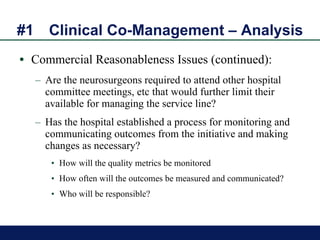
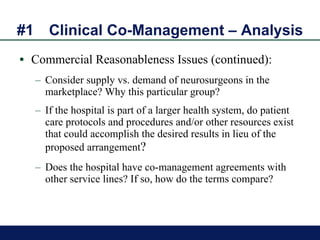
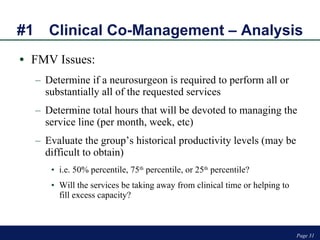
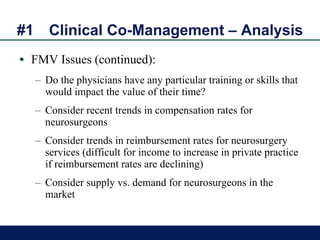
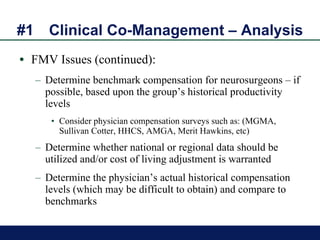
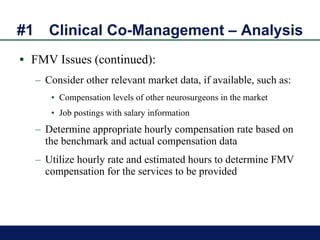
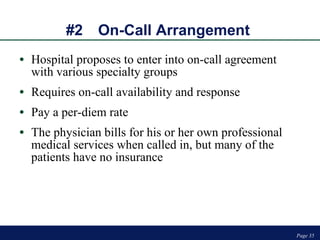
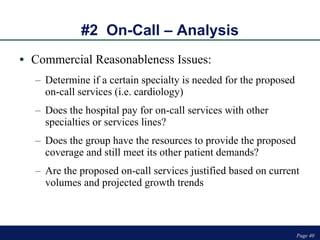
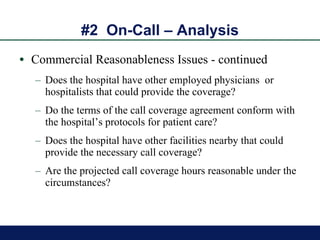
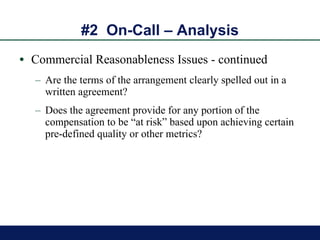
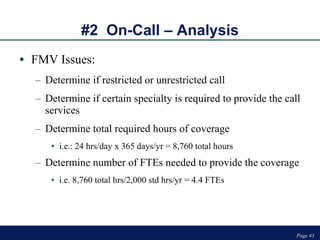
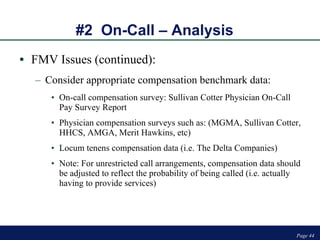
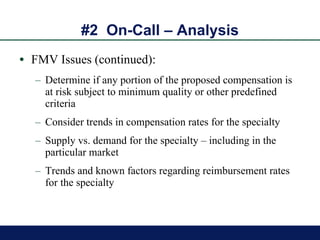
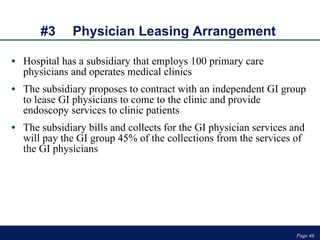
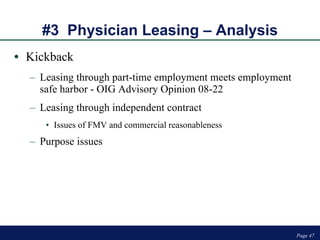
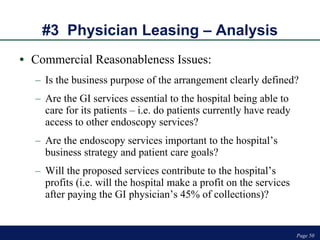
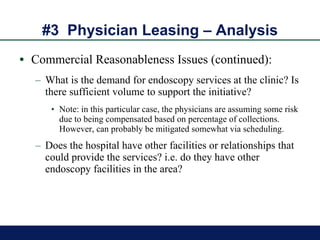
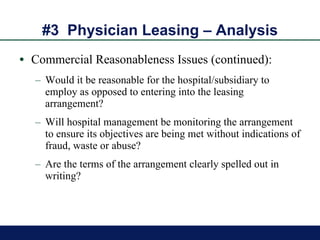
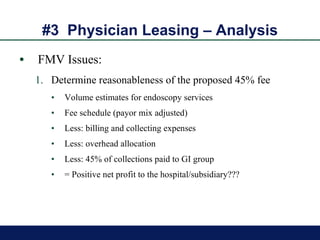
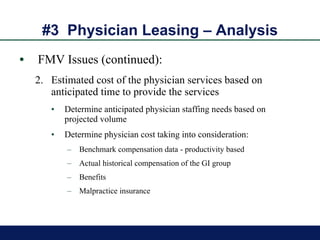
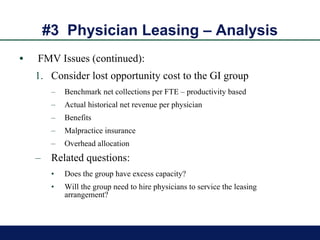
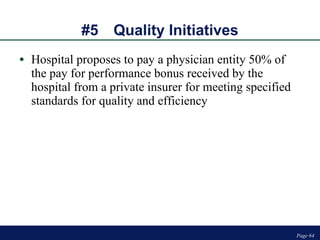
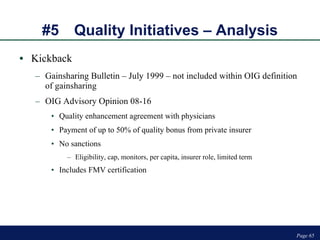
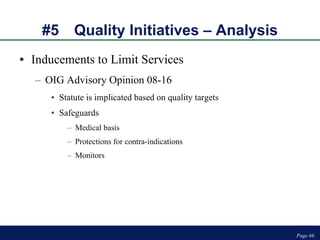
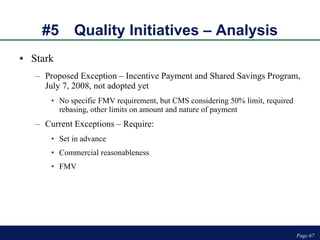
The document discusses the assessment of fair market value and commercial reasonableness in hospital-physician economic relationships, emphasizing compliance with regulations such as the Stark Law and the Anti-Kickback Statute. It highlights the importance of defining commercial reasonableness and fair market value through various factors including business purpose, provider analysis, and resource analysis while applying case studies to illustrate these concepts. The content also outlines specific arrangements such as clinical co-management, on-call agreements, and physician leasing arrangements, addressing the implications of compensation structures and monitoring processes.



![Contact Information Page Page Knoxville - Atlanta - Tampa Bay - Austin W. James Lloyd (865) 673-0844 [email_address] John R. Holdenried (402) 636-8201 [email_address] Visit our web site at www.pyapc.com Visit our web site at www.bairdholm.com](https://image.slidesharecdn.com/hospphyeconomicrelationships-12724143215686-phpapp02/85/Hosp-Phy-Economic-Relationships-71-320.jpg)