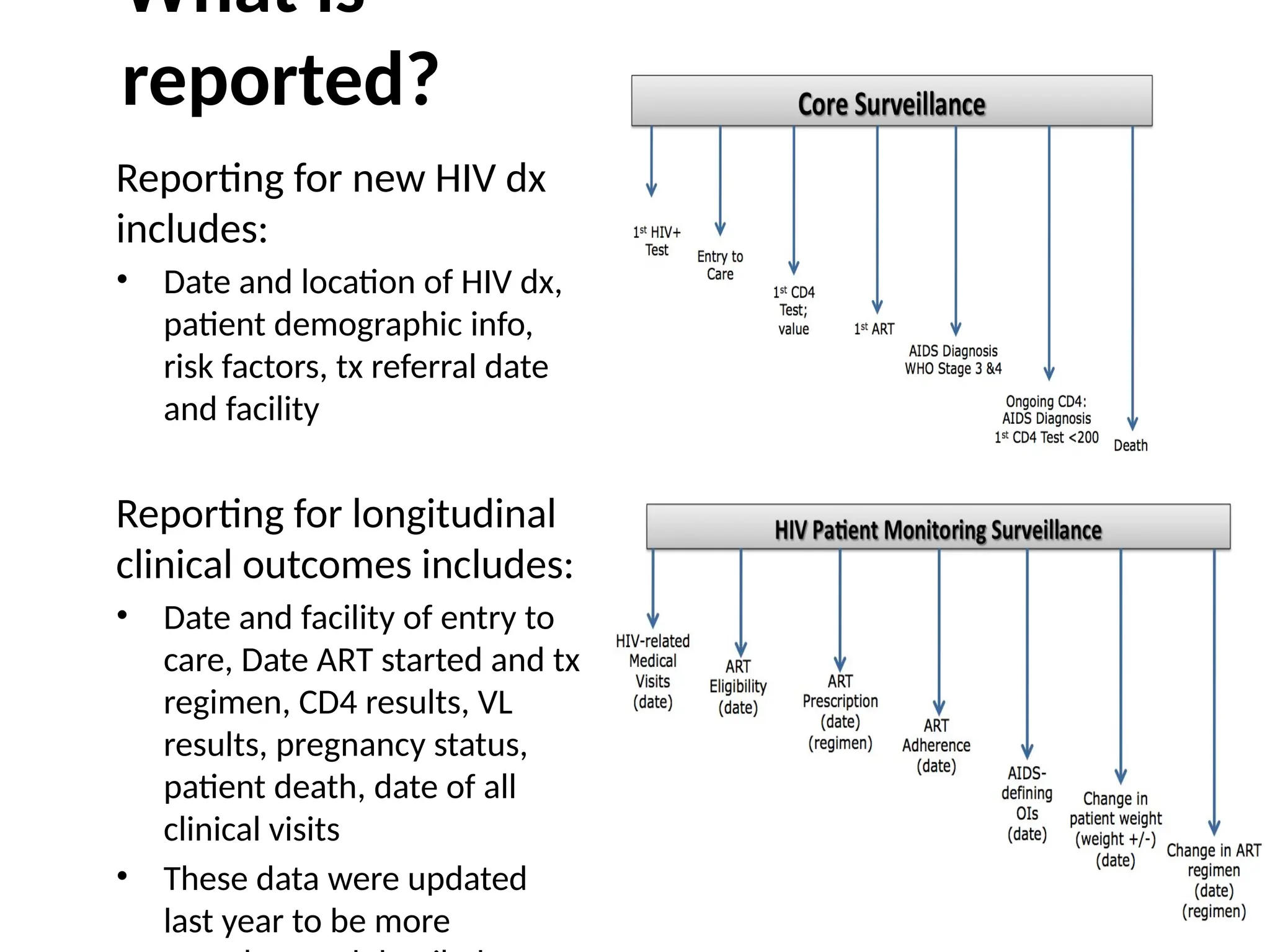
The document discusses HIV case-based surveillance (CBS) as a method for systematically collecting and analyzing data on newly diagnosed HIV cases, highlighting its importance in understanding and monitoring the HIV epidemic. It details various types of surveillance, including biological and behavioral surveillance, as well as sentinel and routine surveillance systems, and emphasizes the role of electronic medical records (EMR) in tracking patient data over time. CBS aims to improve resource allocation for treatment, enhance understanding of the epidemic's trends, and monitor health outcomes for affected populations.