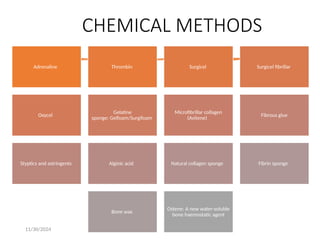
The document discusses various methods of achieving hemostasis in dental and surgical procedures, including mechanical, chemical, and thermal methods. Specific agents and techniques such as sutures, adrenaline, thrombin, and electrocautery are detailed, along with considerations for managing medically compromised patients. It emphasizes the importance of careful patient management in those with conditions such as hypertension, angina, and diabetes during dental treatment.