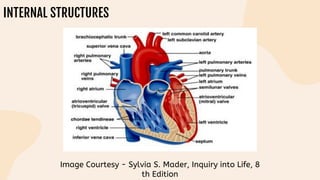
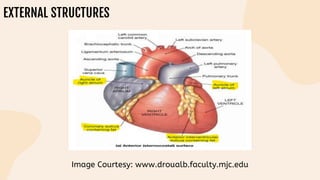
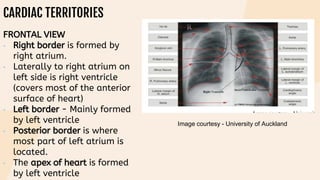
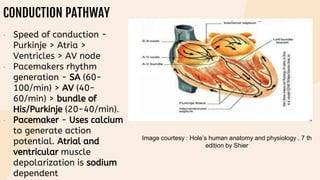
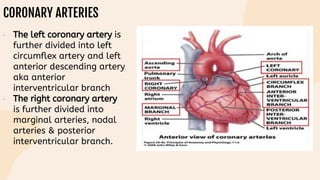
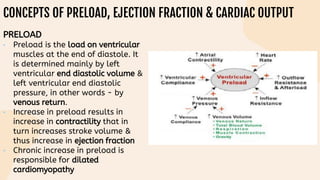
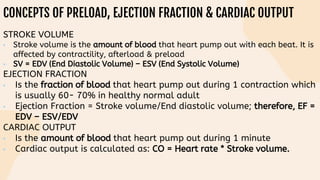
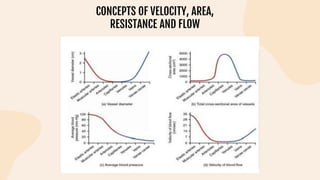
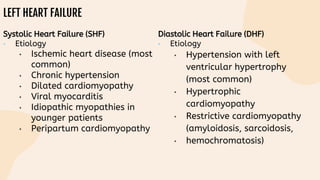
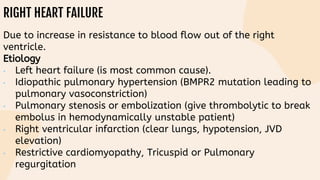
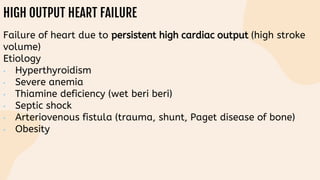
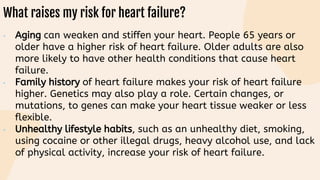
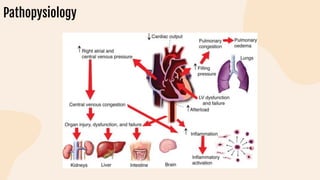
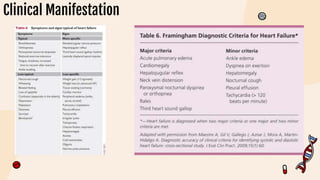
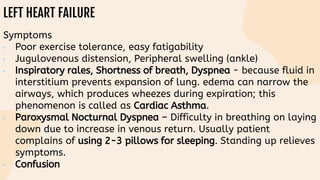
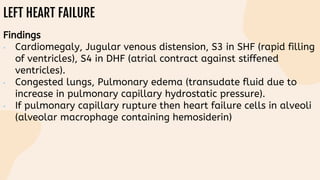
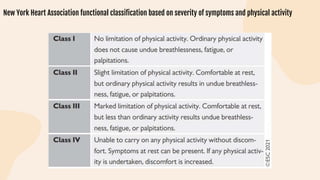
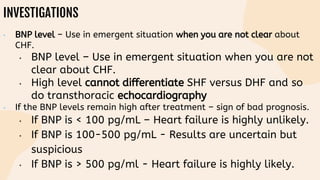
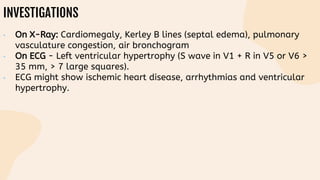
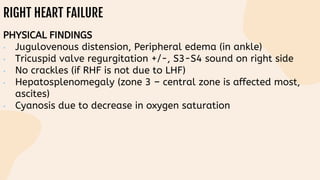
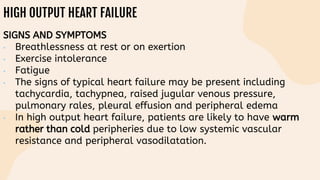
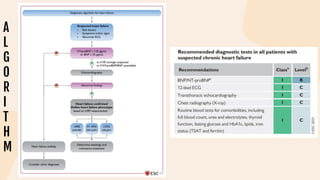
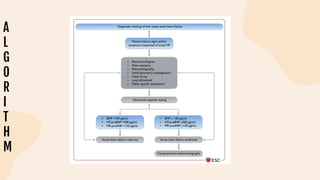
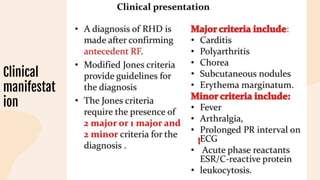
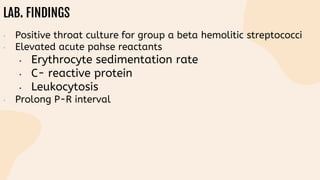
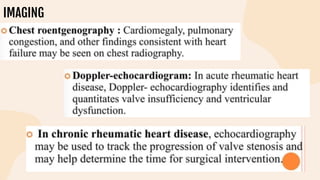
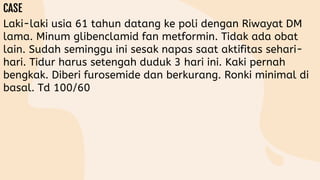
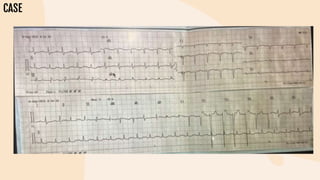
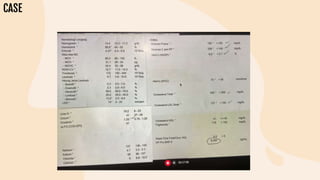
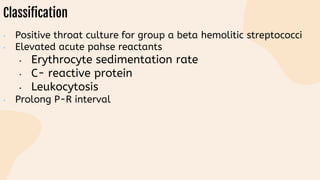
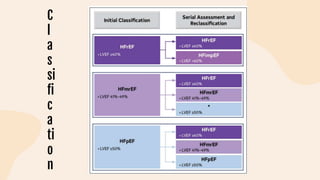
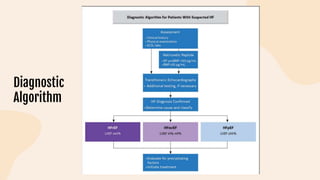
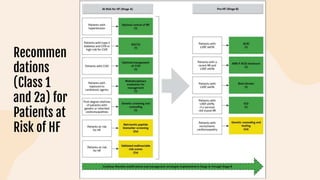
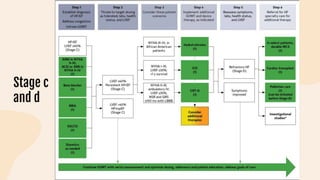
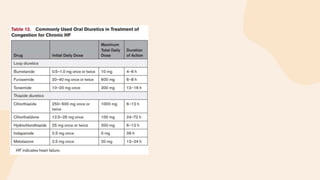
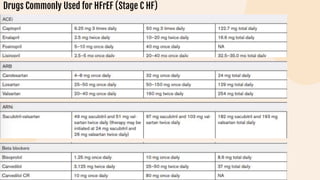
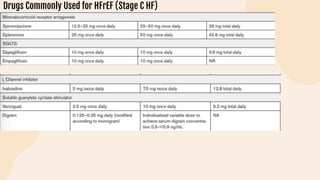
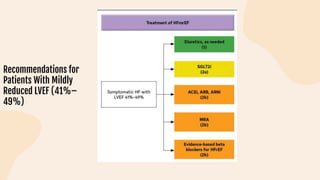
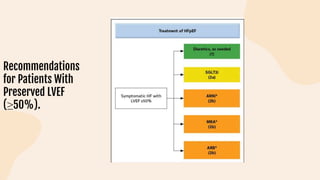
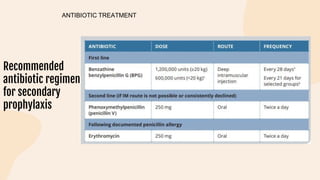
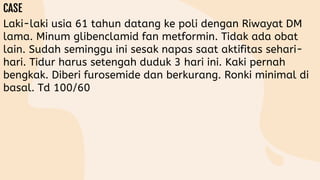
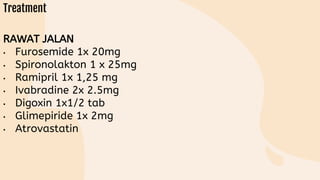
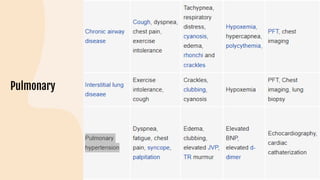
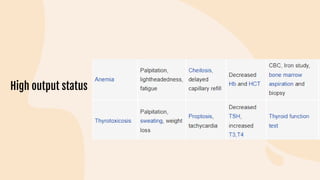
This document provides information on heart failure including its physiology, definition, classification, etiology, risk factors, pathophysiology, clinical manifestation, diagnosis, treatment, and differential diagnosis. It discusses the anatomy of the heart and mediastinum. It defines left heart failure with systolic and diastolic types, right heart failure, and high output heart failure. Risk factors for heart failure include aging, family history, unhealthy lifestyle, and underlying heart/lung conditions. Clinical exams may reveal jugular venous distension, lung crackles, edema. Diagnostic tests include BNP, ECG, echocardiogram, and chest x-ray. Treatment involves drugs like ACE inhibitors, ARBs, beta-blockers, di