The Gleason grading system originated in the 1960s-1970s as a way to histologically grade prostate adenocarcinoma based on architectural patterns. It defines five histological growth patterns (Gleason grades 1-5) that correlate with tumor differentiation and prognosis. The Gleason score, which is the sum of the primary and secondary grades, better correlates with tumor behavior. The system has undergone modifications over time to address new understandings of prostate cancer pathology. The 2005 ISUP consensus updated grading criteria and eliminated rare Gleason 1 patterns. It also moved some Gleason 3 cribriform patterns and poorly formed glands to Gleason 4. Reporting recommendations include including the highest grade when three patterns are present in a

![Gleason Pattern 1
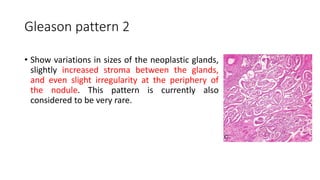
• characterized by a well-circumscribed,
nodular lesion composed of roughly
uniform, closely compacted, discrete,
well-differentiated glands of moderate
size.
• It has been recognized that this “pattern”
is extremely rare, if not non-existent, and
many of the ones defined by Dr. Gleason
in his original study may be mimicking
lesions [such as adenosis or atypical
adenomatous hyperplasia (AAH)] rather
than bona fide prostate cancer.](https://image.slidesharecdn.com/gleasongradingsystem-171209105910/85/Gleason-grading-system-6-320.jpg)