This document discusses myths and facts about aging, physical and psychological changes that occur with aging, and care considerations for various body systems in older adults. Key points include:
- Common myths about aging include ideas that all elderly live in poverty or nursing homes, when in reality aging is gradual and varies between individuals.
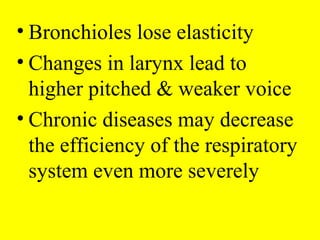
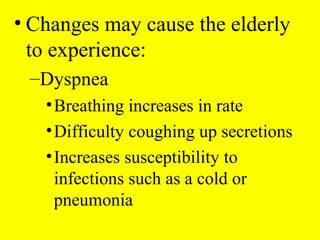
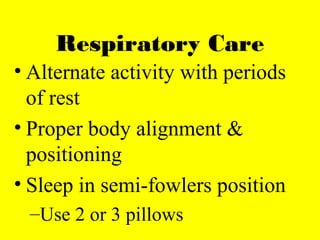
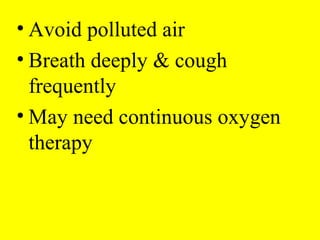
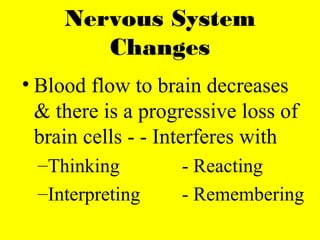
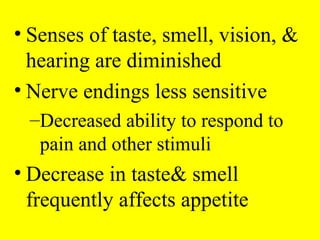
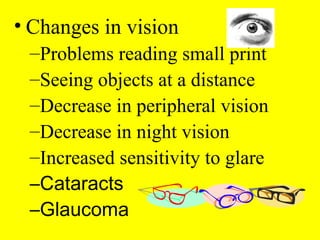
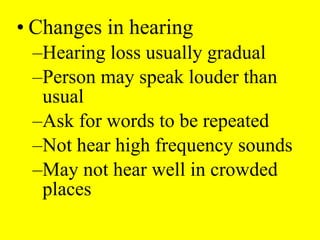
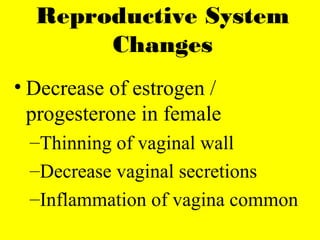
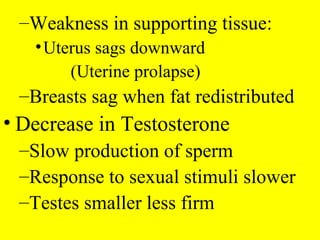
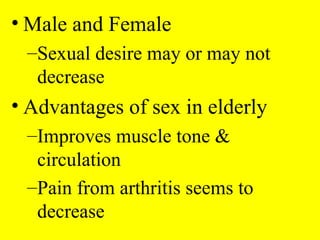
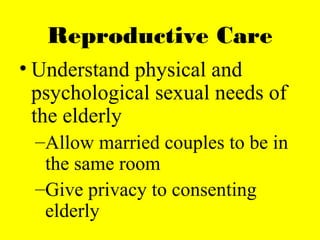
- Physical changes with aging include decreased skin elasticity, circulation, and function of respiratory, digestive and urinary systems. Care focuses on exercise, nutrition, hygiene and preventing infections.
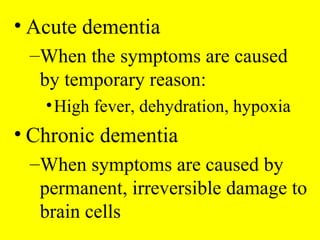
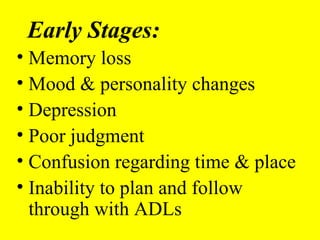
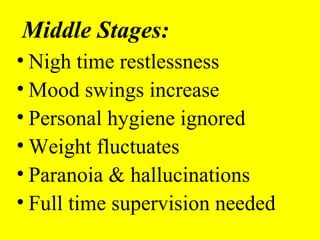
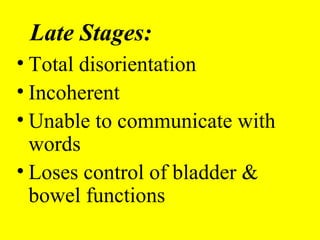
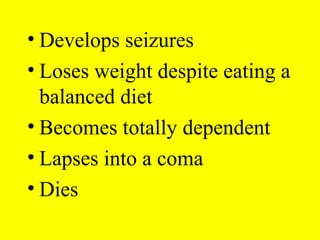
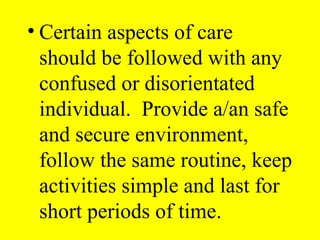
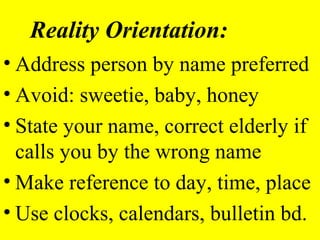
- Psychological changes can include increased confusion, depression and dementia. Providing a routine, reality orientation and avoiding overstimulation are important for care.
- Meeting cultural, religious and safety needs of older adults


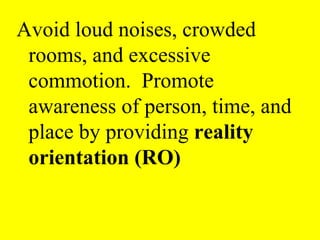
![• Keep individual oriented to day
night cycles:
–Regular clothes during the day
–Open curtains during the day]
–Close curtains at night
–Pajamas at night](https://image.slidesharecdn.com/geriatricsppt-160807191450/85/Geriatrics-ppt-54-320.jpg)