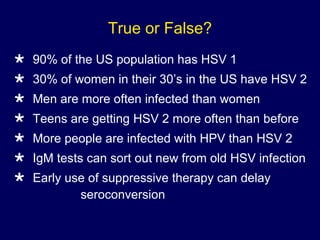
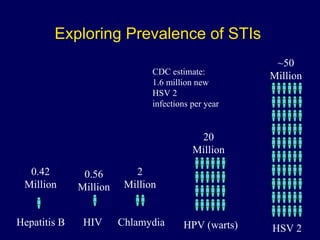
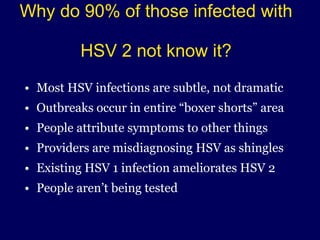
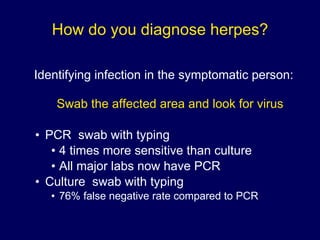
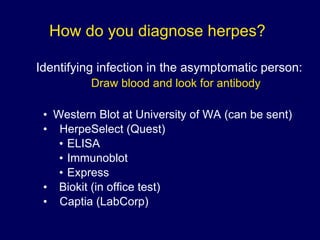
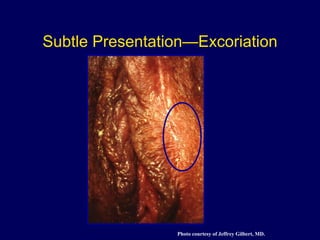
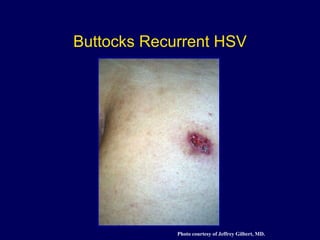
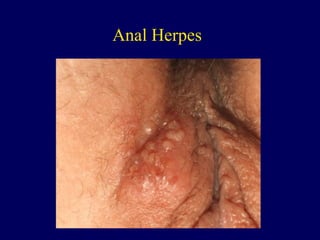
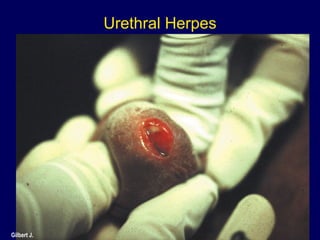
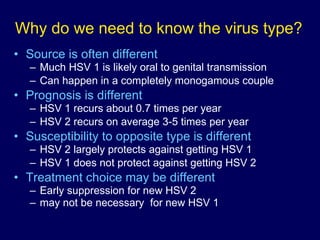
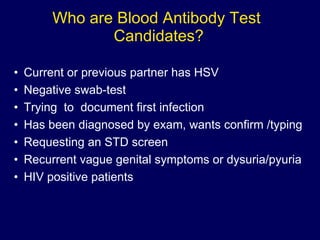
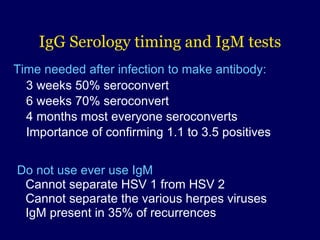
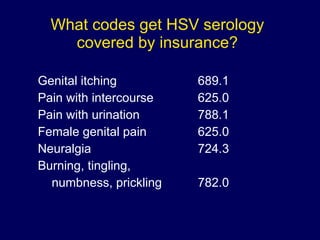
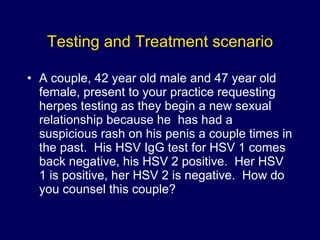
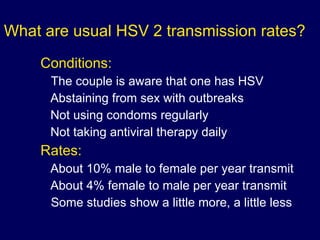
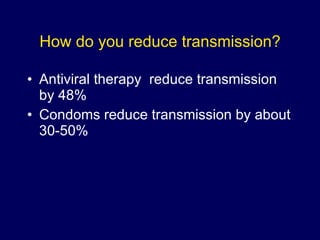
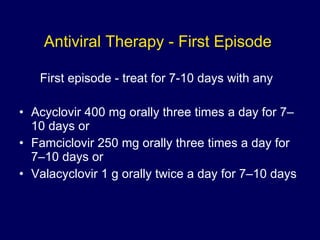
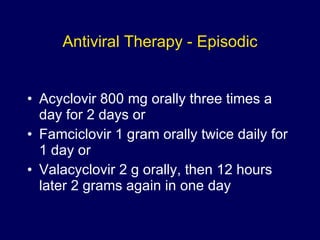
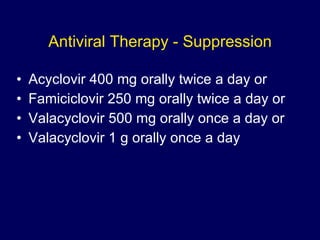
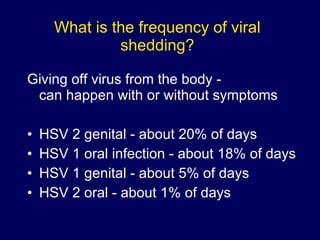
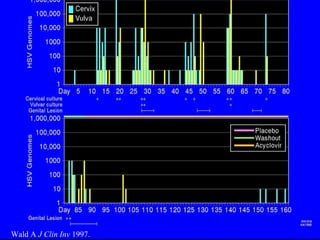
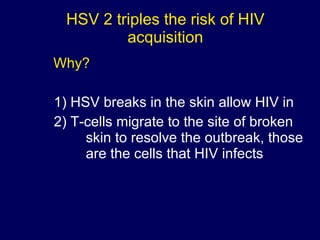
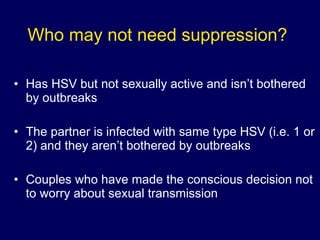
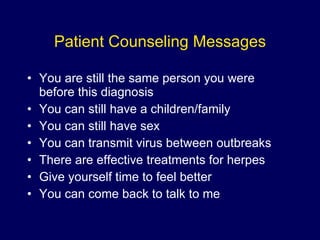
The document discusses the prevalence and testing of genital herpes, noting that a significant portion of the population is unaware of their HSV-2 infection. It outlines diagnostic methods, treatment options, and the importance of understanding virus types for management and transmission reduction. Additionally, it provides scenarios for patient counseling and addresses the impact of herpes on relationships and sexual health.