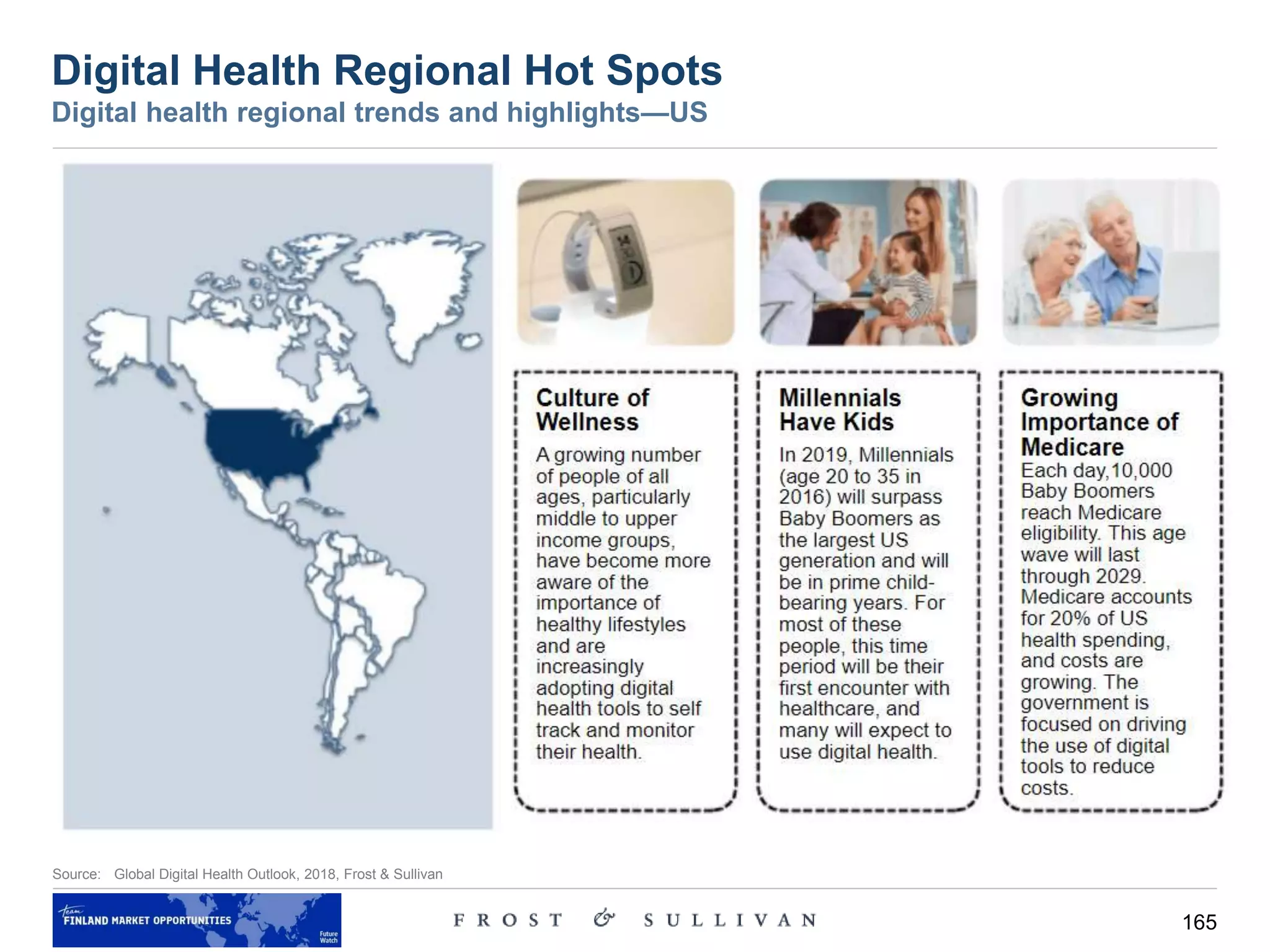
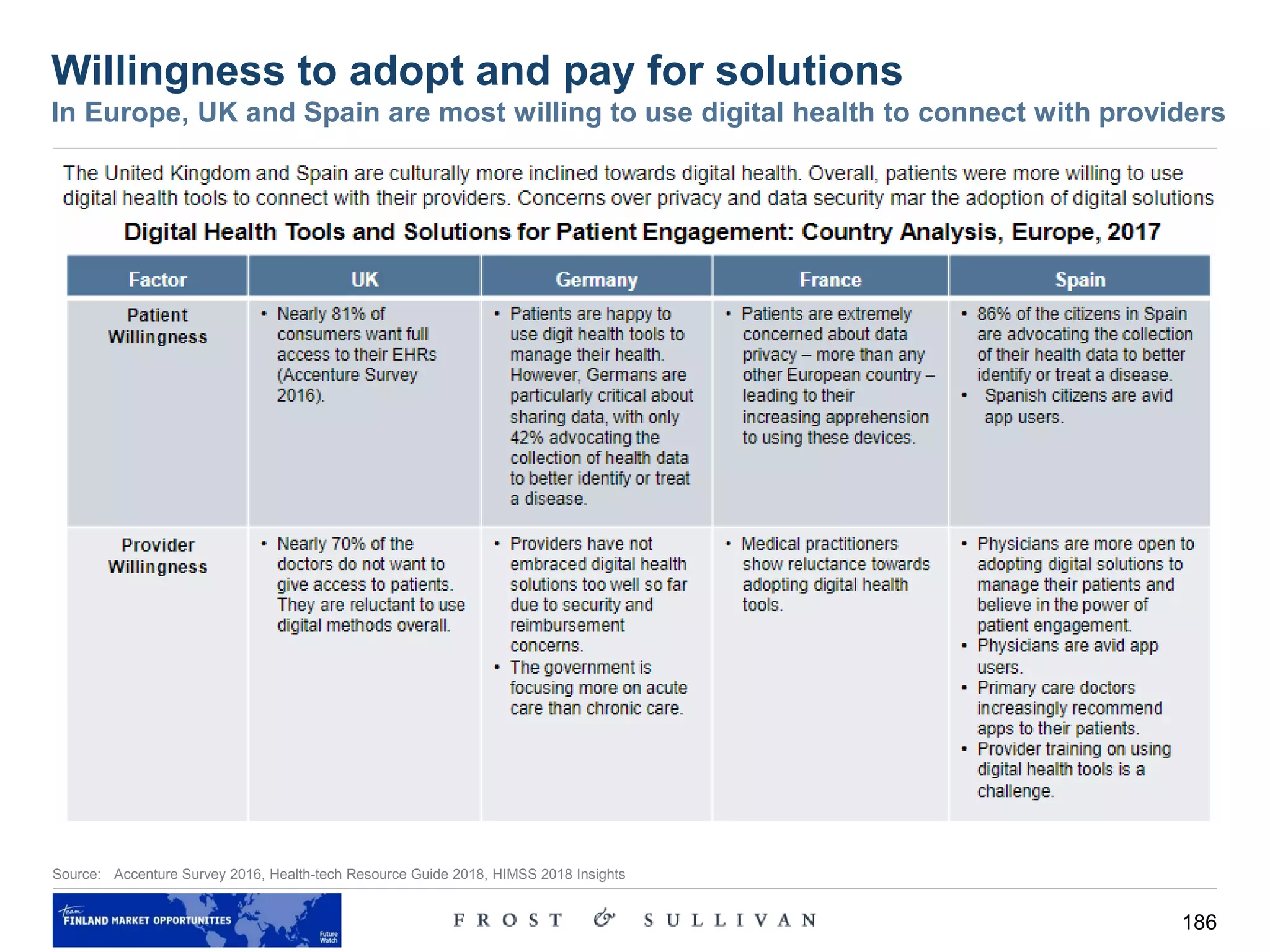
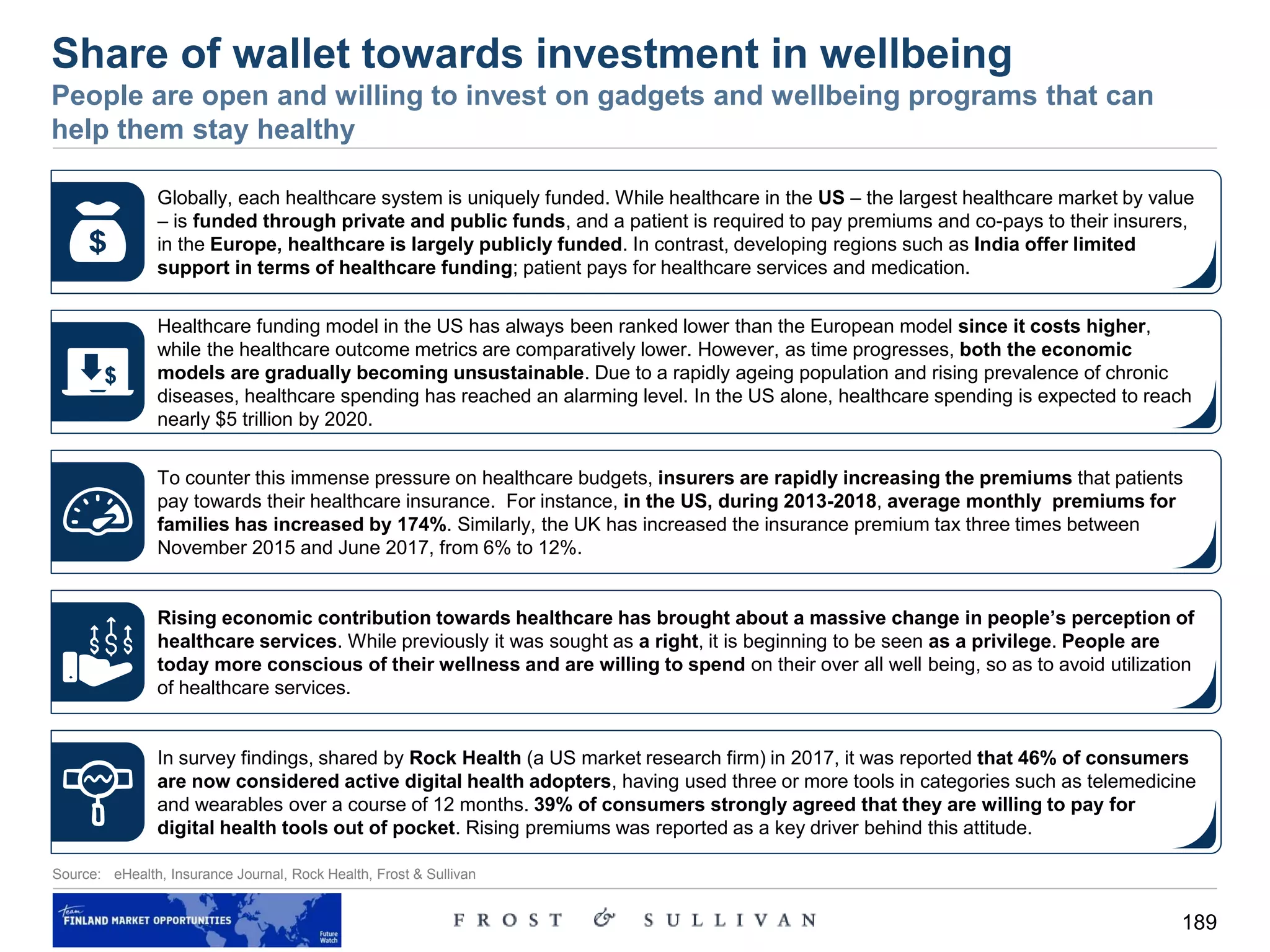
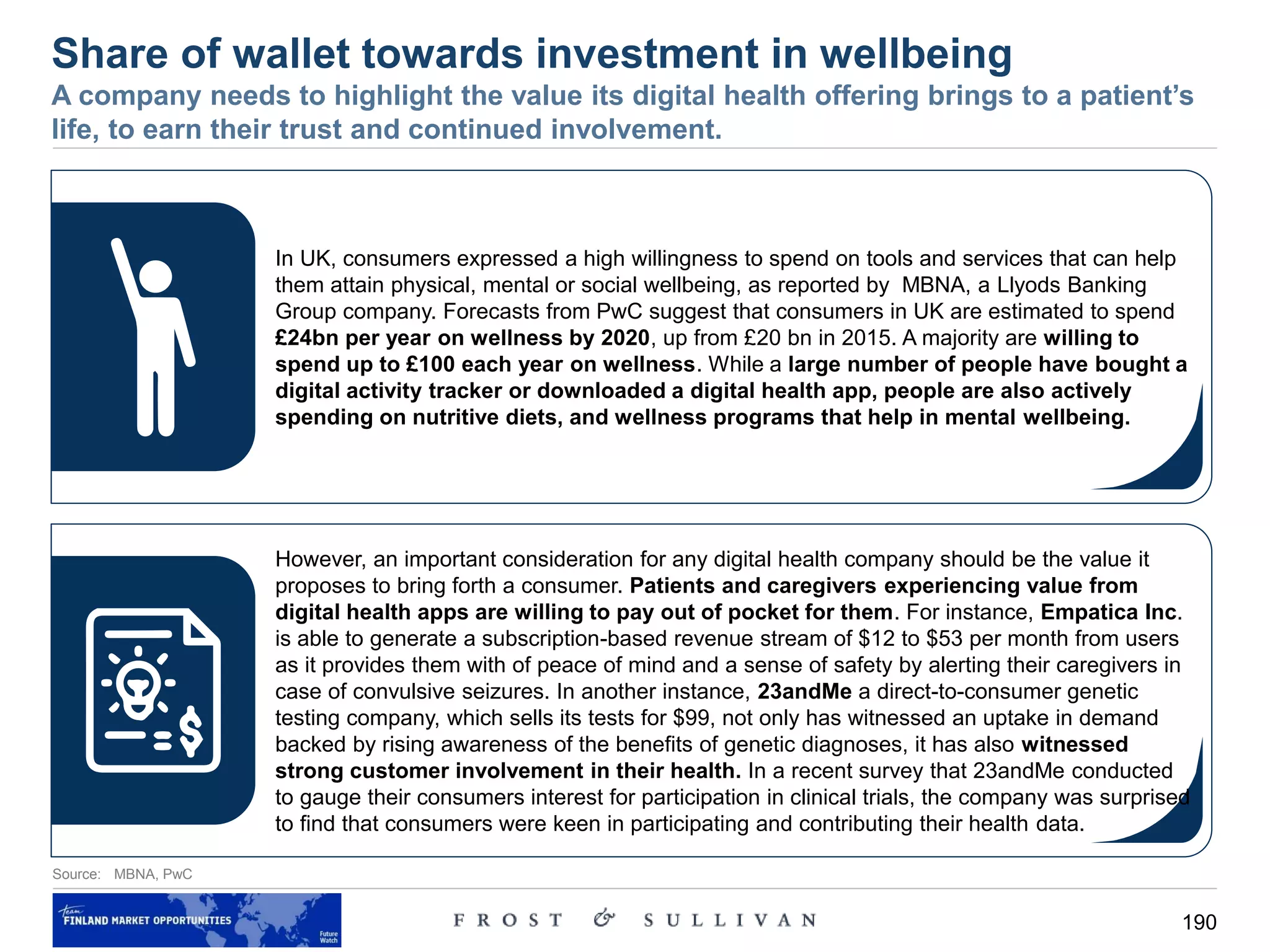
1) Developed countries aim to increase patient accountability and focus on education and awareness programs to promote healthier lifestyles.
2) Developing countries struggle to meet basic healthcare demands of large populations due to limited funding and infrastructure.
3) Examples provided of successful programs in Finland and the US that use incentives and competitions to encourage physical activity and reduce chronic diseases.



























![39
Source: Vision 2025 – Healthcare in the Smart Home, Frost & Sullivan, HealthCatalyst
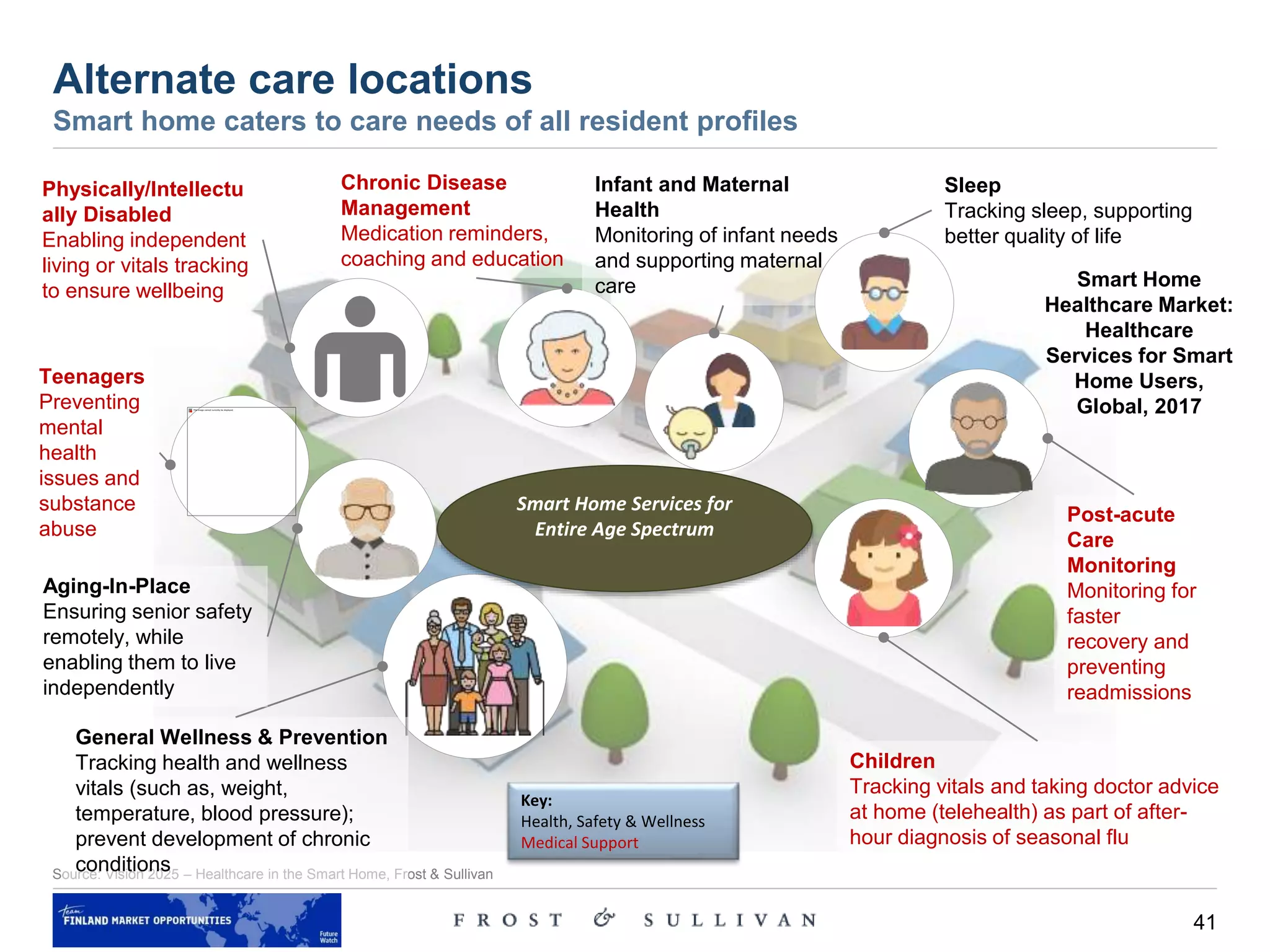
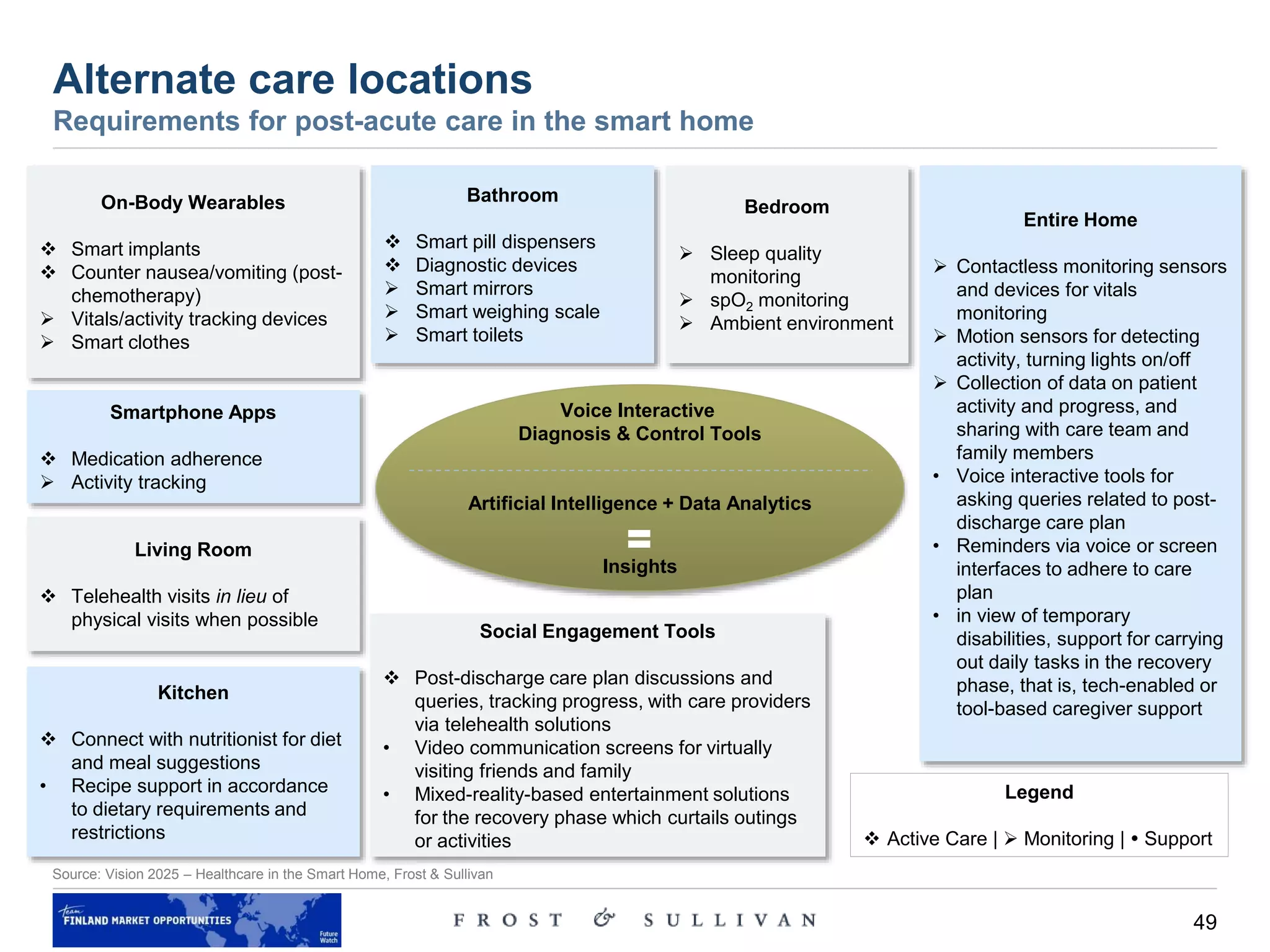
Alternate care locations – discussion
Care delivery moving to the home environment
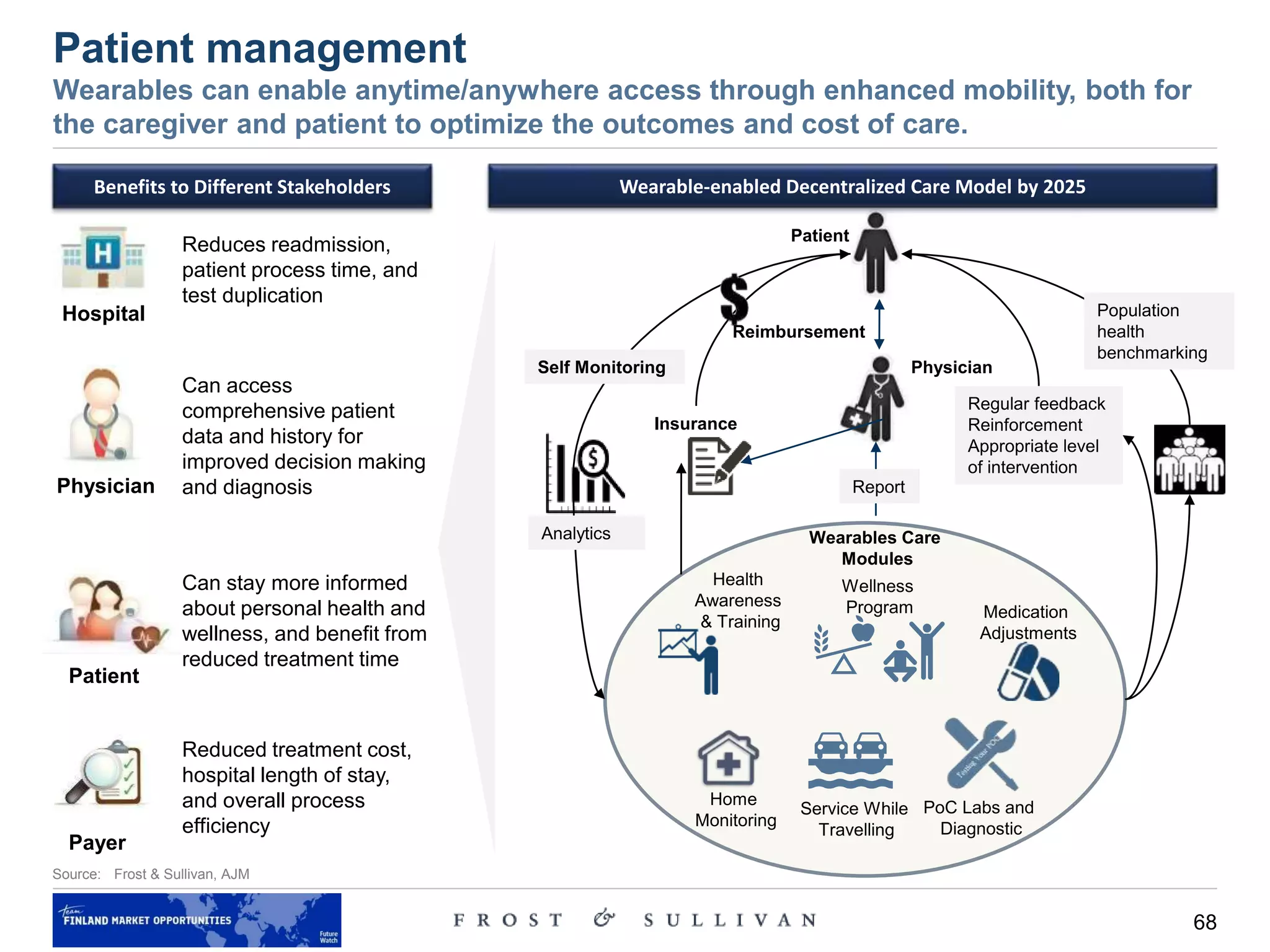
• The industry is gradually evolving to acknowledge the ‘anytime, anywhere care’ model, and the result is the remodeling
of healthcare services to suit this trend. Technological developments and the Internet of Things (IoT) enable a home to
evolve into a connected home. We believe that the convergence of these trends—focus on prevention and
wellness, care delivery moving in to the home and endless home automation possibilities—is imminent.
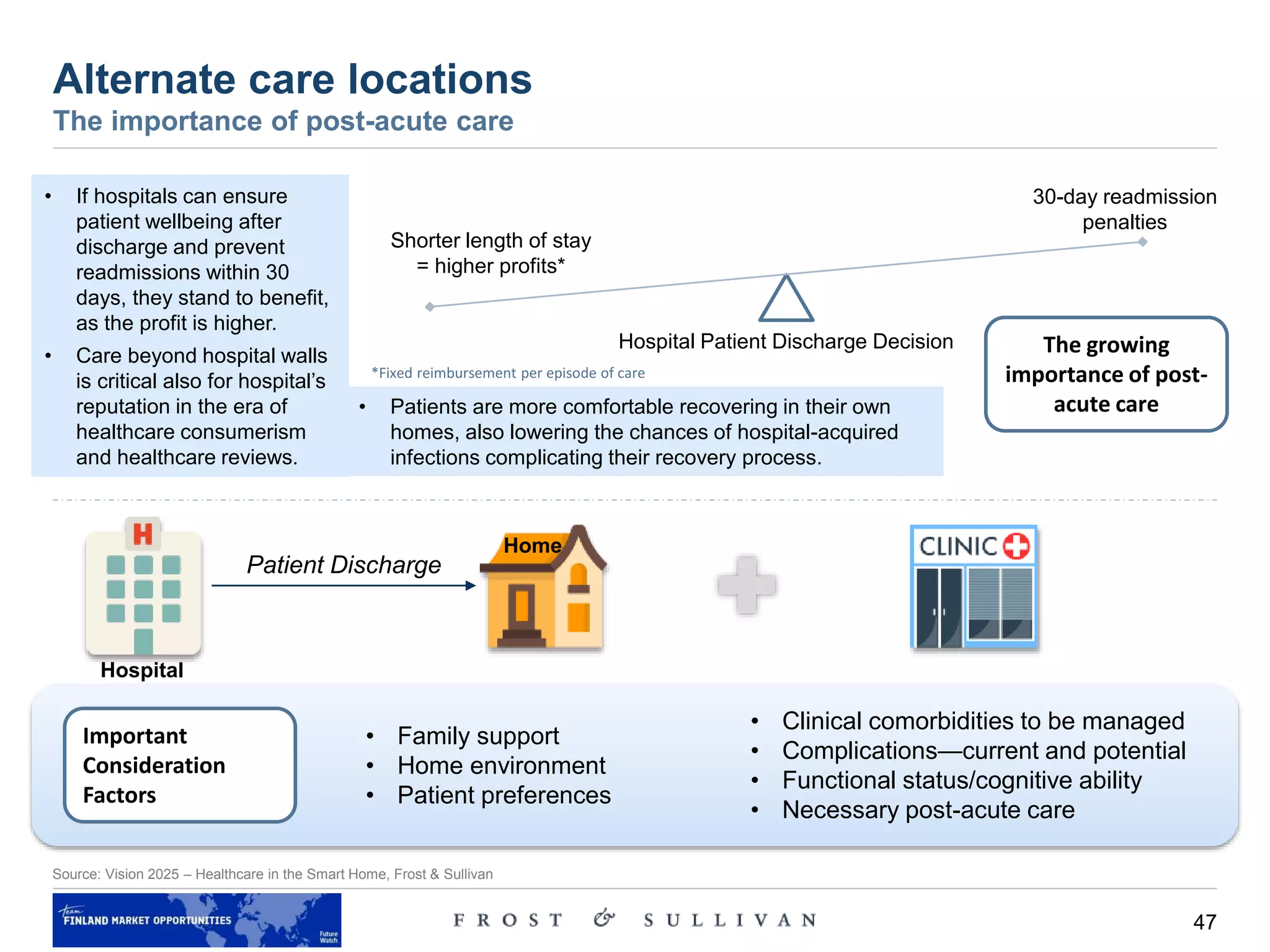
• According to a report on the Clinically Appropriate & Cost-Effective Placement Project (CACEP) from the Alliance for
Home Health Care Quality and Innovation, Medicare could reduce its spending by $34.7 billion over a 10-year period
by shifting patient care settings from facility-based care to home and community-based care. Additional $100 billion
could be saved if care delivery were restructured to be less wasteful and more effective.
Pharmacy
Patient
Visits
Path lab
Clinic
Health &
wellness
stores
Telemedicine
Home testing/collection
Online stores
[nutrition, wellness, medical devices]
House call
Products
and
Services
Visit
Patient.
ePharmacy/third-party delivery
Past Present
Healthcare Market: State of Care Delivery, Global, Past, Present & Future
In future, integration of
digital solutions will be
more concrete and visible](https://image.slidesharecdn.com/futurewatchhealthwellbeinginadigitalage-vision2025-190524094543/75/Future-Watch-Health-and-wellbeing-in-a-digital-age-vision-2025-39-2048.jpg)