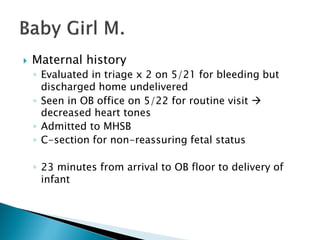
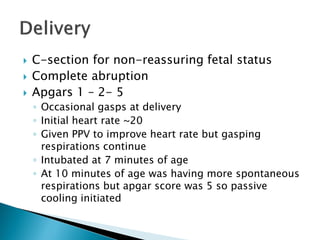
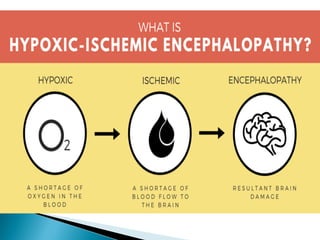
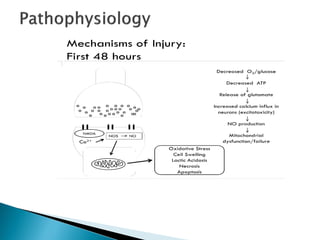
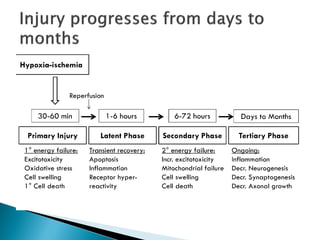
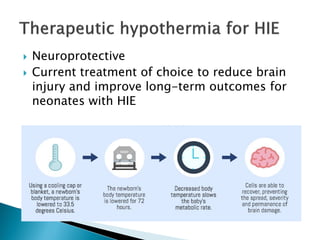
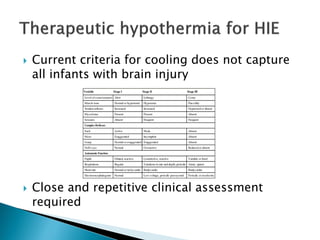
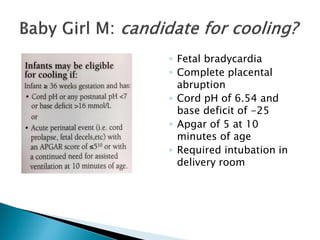
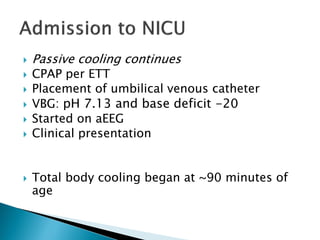
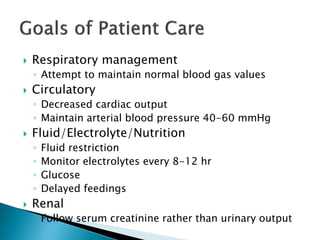
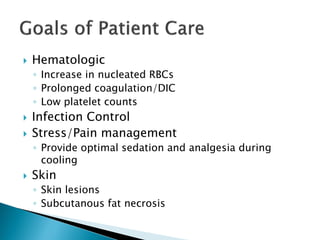
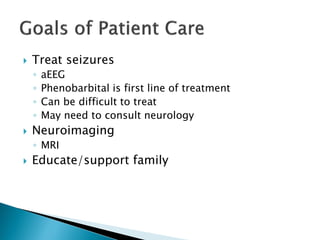
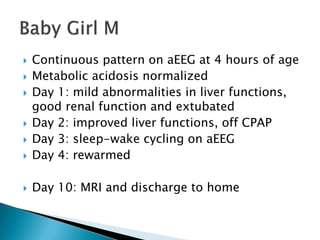
This document summarizes the resuscitation, admission, and treatment of an infant named Baby Girl M who experienced hypoxic-ischemic encephalopathy (HIE) due to a placental abruption and complete fetal bradycardia. It reviews the criteria for therapeutic hypothermia treatment of HIE and the goals of cooling infants with HIE to reduce brain injury. It then details Baby Girl M's resuscitation in the delivery room, admission to the NICU, initiation of cooling treatment, management over several days, and discharge home after improvement.