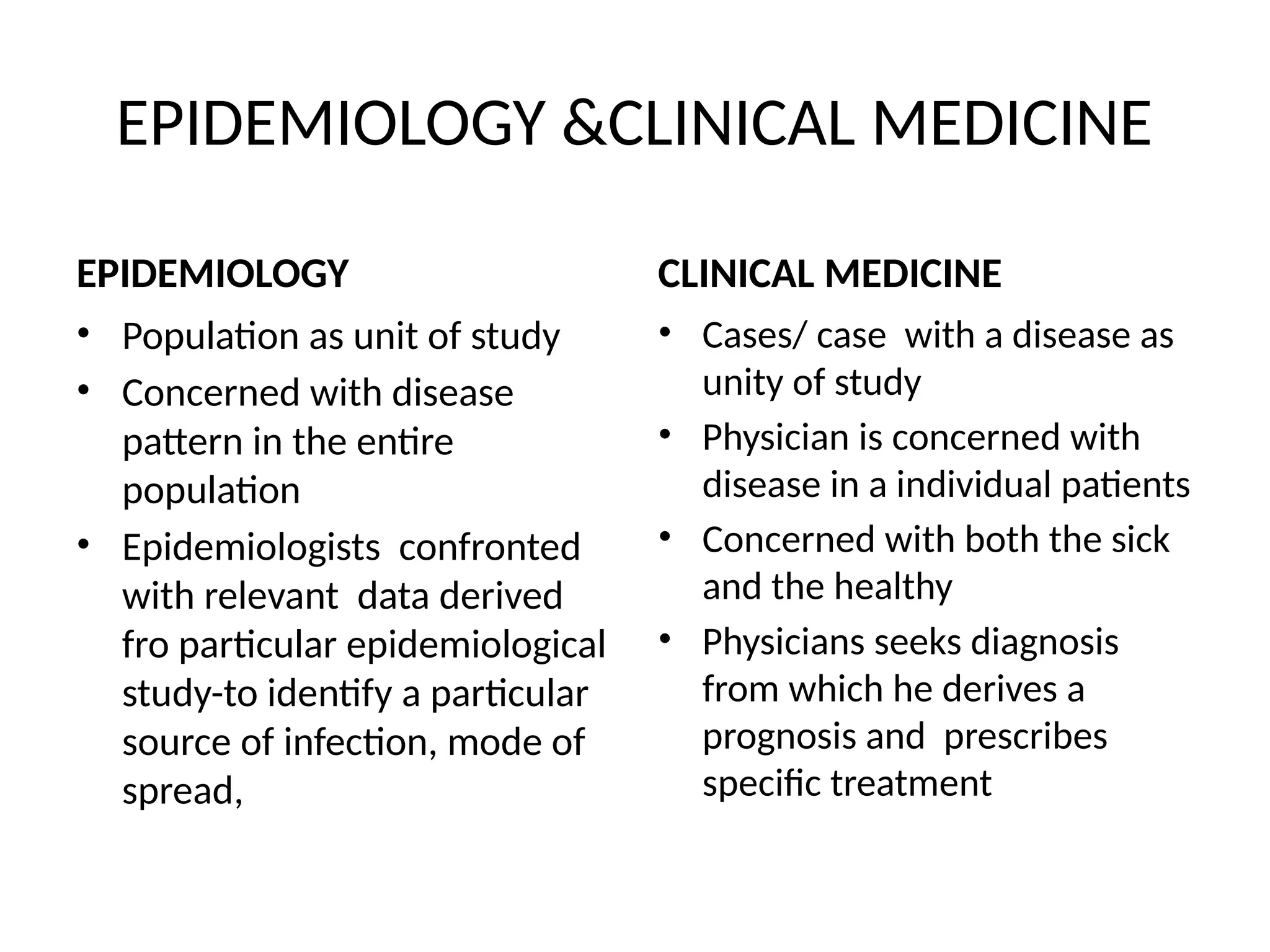
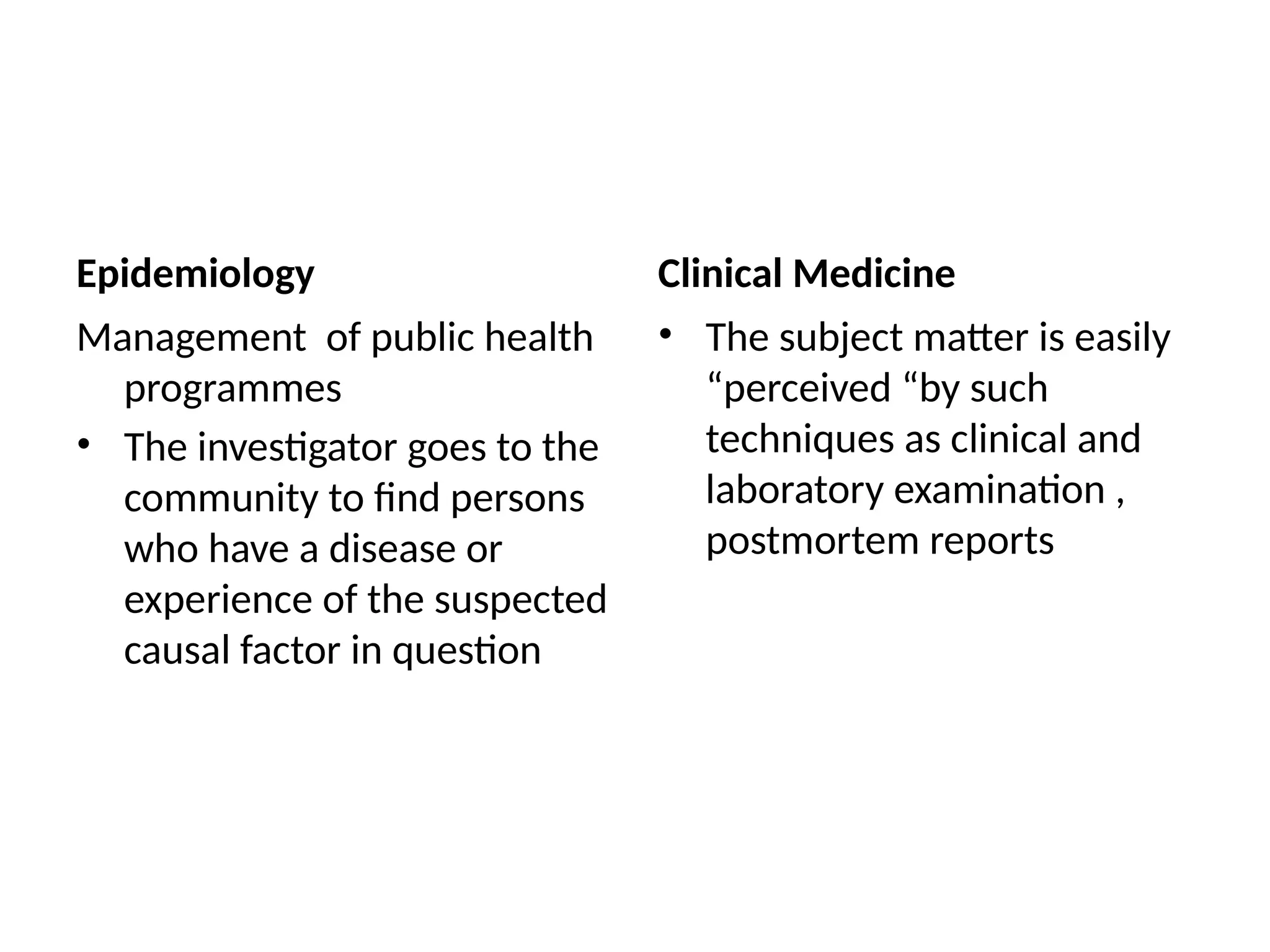
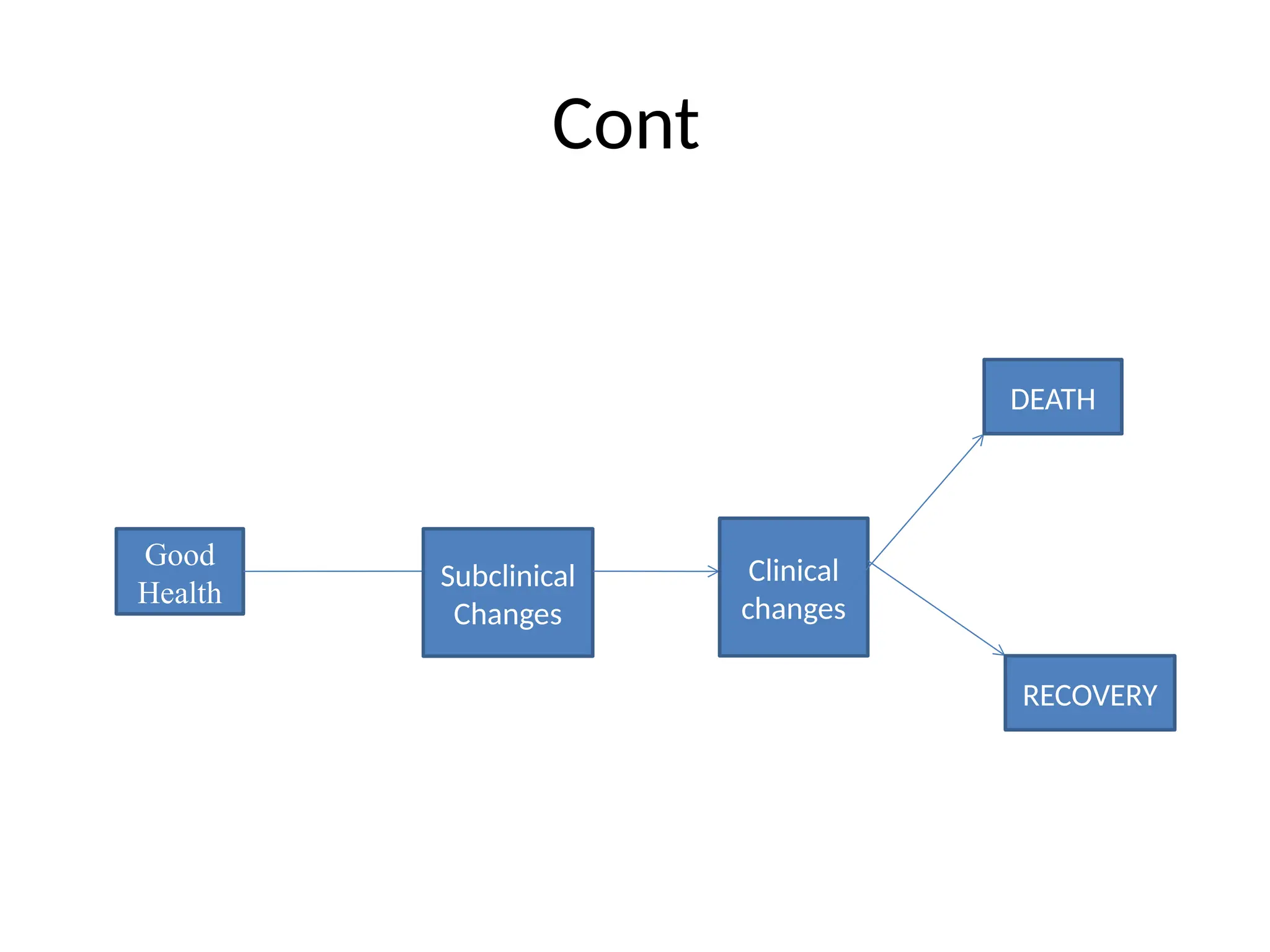
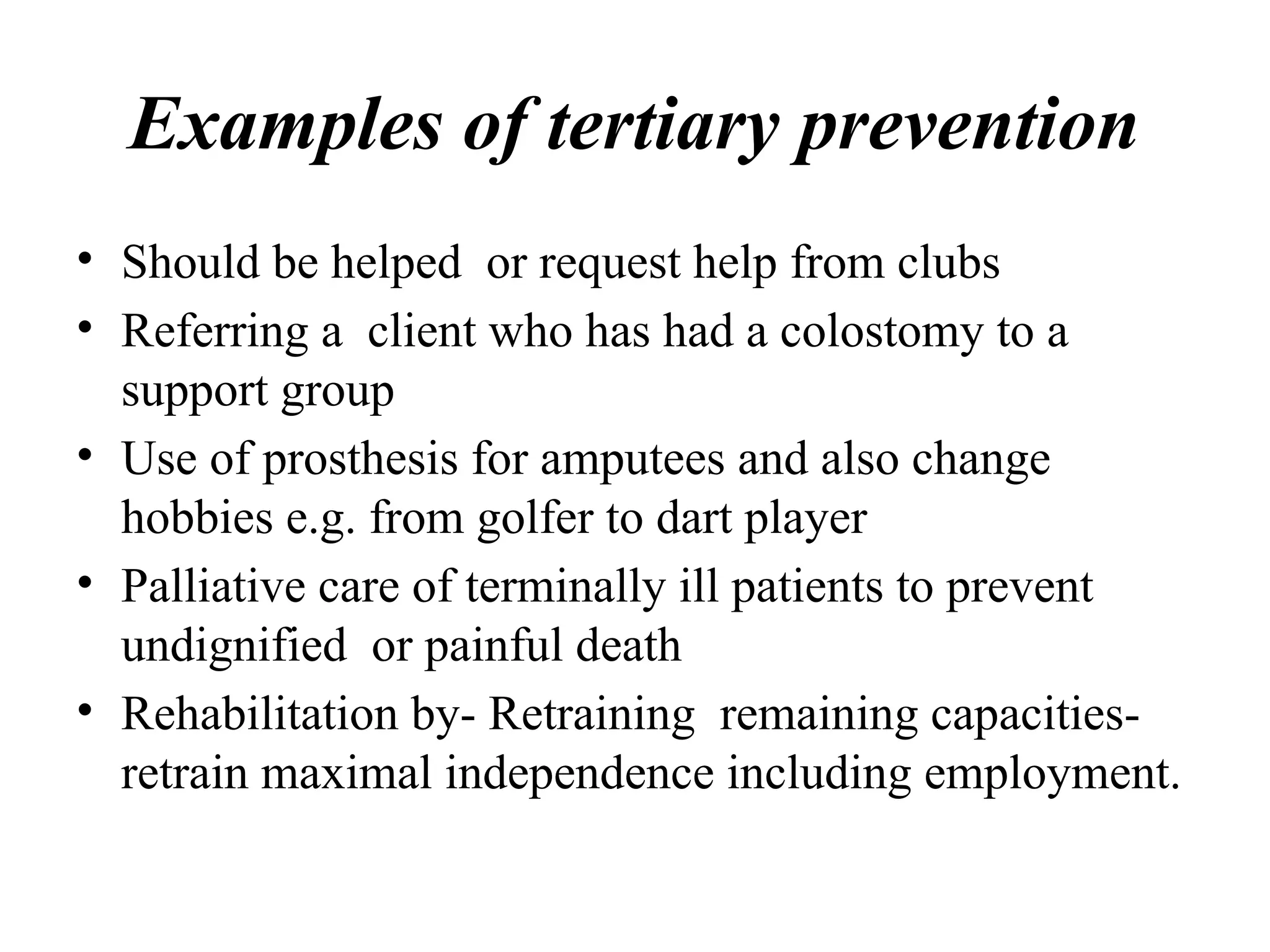
The document provides an introduction to epidemiology, detailing the objectives and foundational concepts, including its historical context and the evolution of the field. It defines epidemiology as the study of health-related states in populations to inform prevention and control measures. The document also outlines the levels of disease prevention and the significance of understanding disease patterns and transmission dynamics.