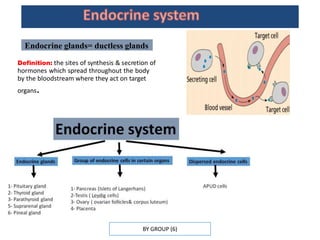
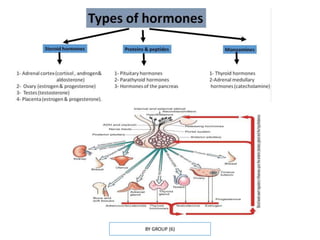
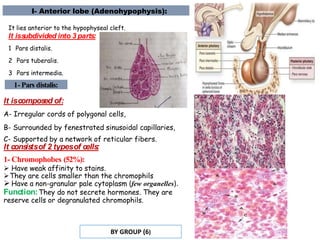
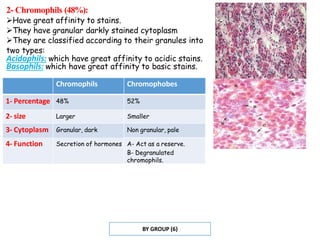
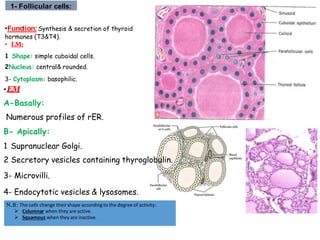
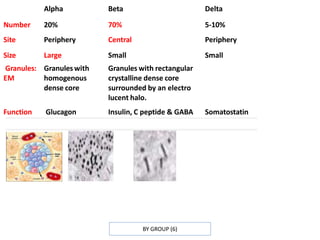
The document summarizes the structure and function of several endocrine glands, including the pituitary gland, thyroid gland, parathyroid gland, and adrenal glands. The pituitary gland has an anterior and posterior lobe. The anterior lobe contains chromophils that secrete hormones like growth hormone and prolactin, and chromophobes that act as reserve cells. The thyroid gland contains follicles lined with follicular cells that secrete thyroid hormones and parafollicular cells that secrete calcitonin. The parathyroid glands contain chief cells that secrete parathyroid hormone. The adrenal glands have an outer cortex that produces steroid hormones and an inner medulla that secretes catecholamines.