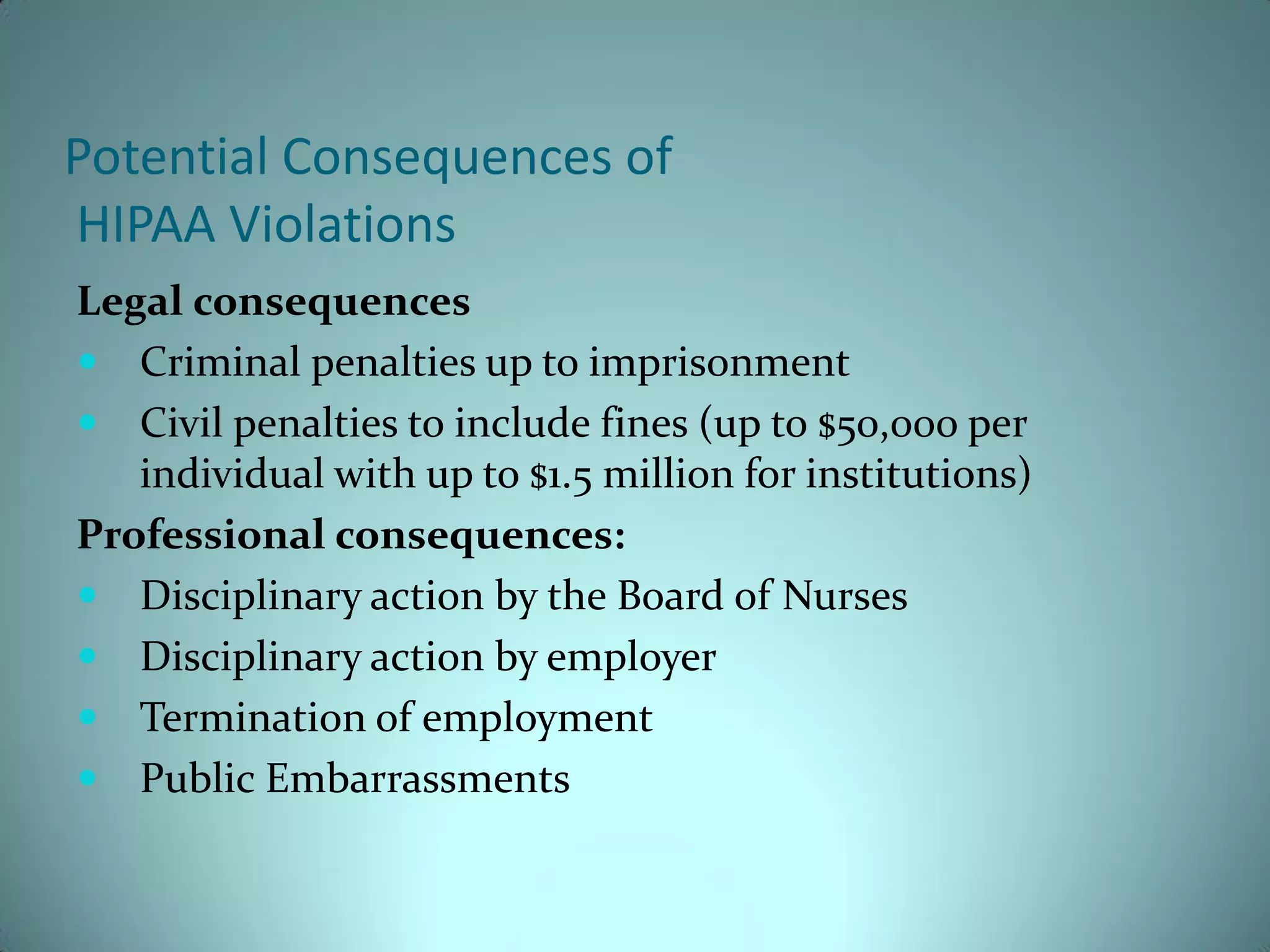
This document summarizes the key aspects of the Health Insurance Portability and Accountability Act (HIPAA) regulations regarding patient privacy and the handling of protected health information. It notes that HIPAA was passed as a federal law in 1996 and outlines regulations to protect individuals' health information privacy and ensure security of electronic personal data transfers. The document then discusses how health information is used by various medical professionals and entities involved in patient care and lists some examples. It also provides an overview of the objectives of HIPAA, patients' rights to their information, and consequences for violations.