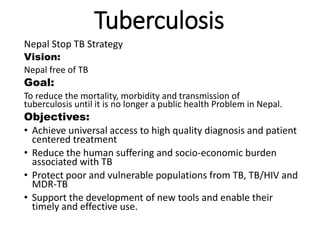
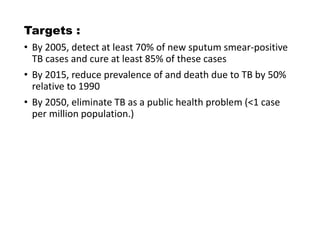
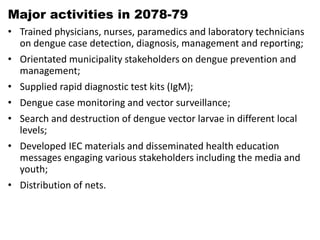
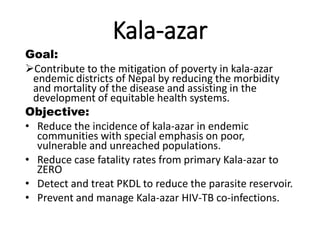
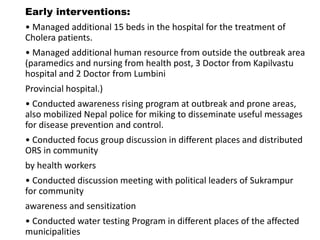
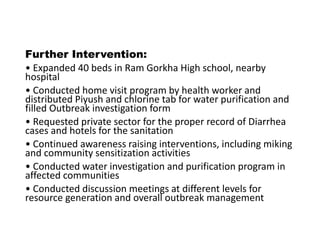
The document summarizes the major disease control programs in Nepal, including their goals, objectives, strategies and current status. It discusses programs for tuberculosis, HIV/AIDS, dengue, leprosy, scrub typhus, lymphatic filariasis, malaria, kala-azar, cholera and zoonotic diseases. The key goals are to reduce incidence, mortality and transmission of these diseases and ensure universal access to diagnosis and treatment. Strategies involve prevention, surveillance, vector control, social mobilization and strengthening health systems.