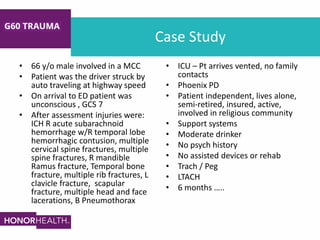
This document discusses discharge planning considerations for the geriatric (G-60) trauma population. It notes that this population is aging and experiencing increasing traumatic injury. A multidisciplinary team conducts early assessments to determine baseline capabilities and develop individualized discharge plans. Barriers to timely discharge include insurance approval delays. The document reviews potential post-acute settings like skilled nursing facilities, acute rehabilitation hospitals, and long-term acute care hospitals. It provides a case study example and emphasizes the importance of early multidisciplinary collaboration and discharge planning.