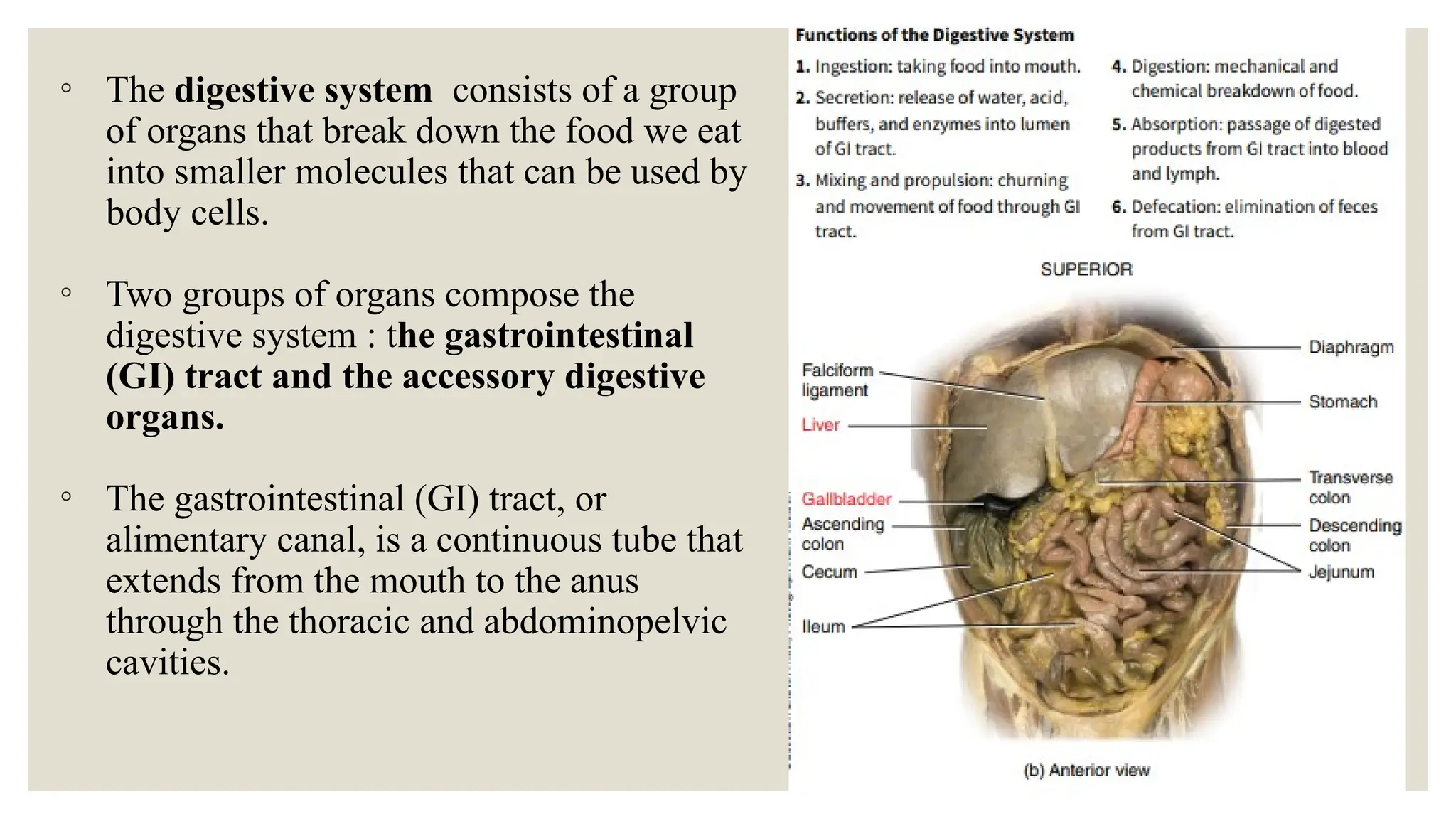
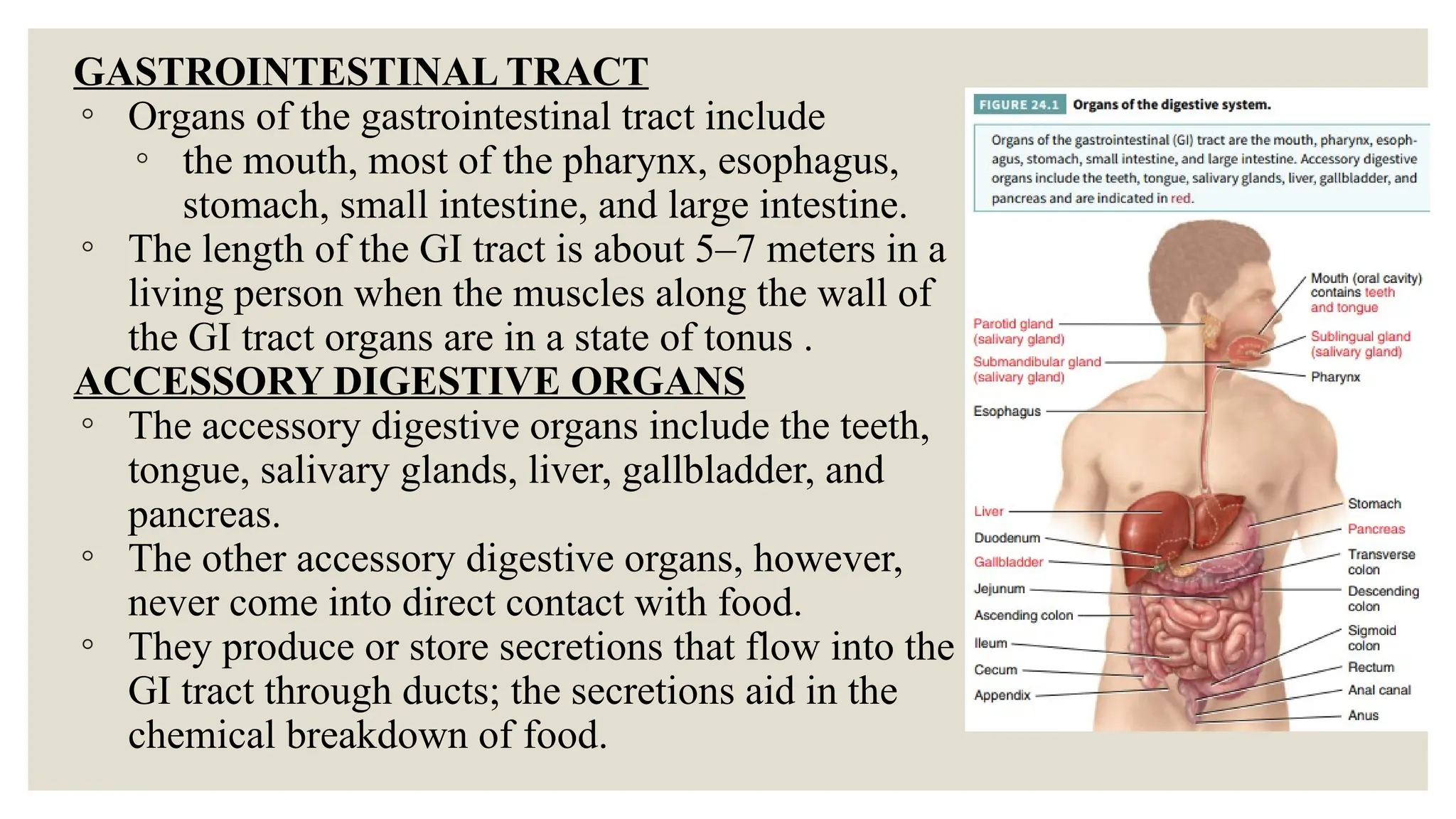
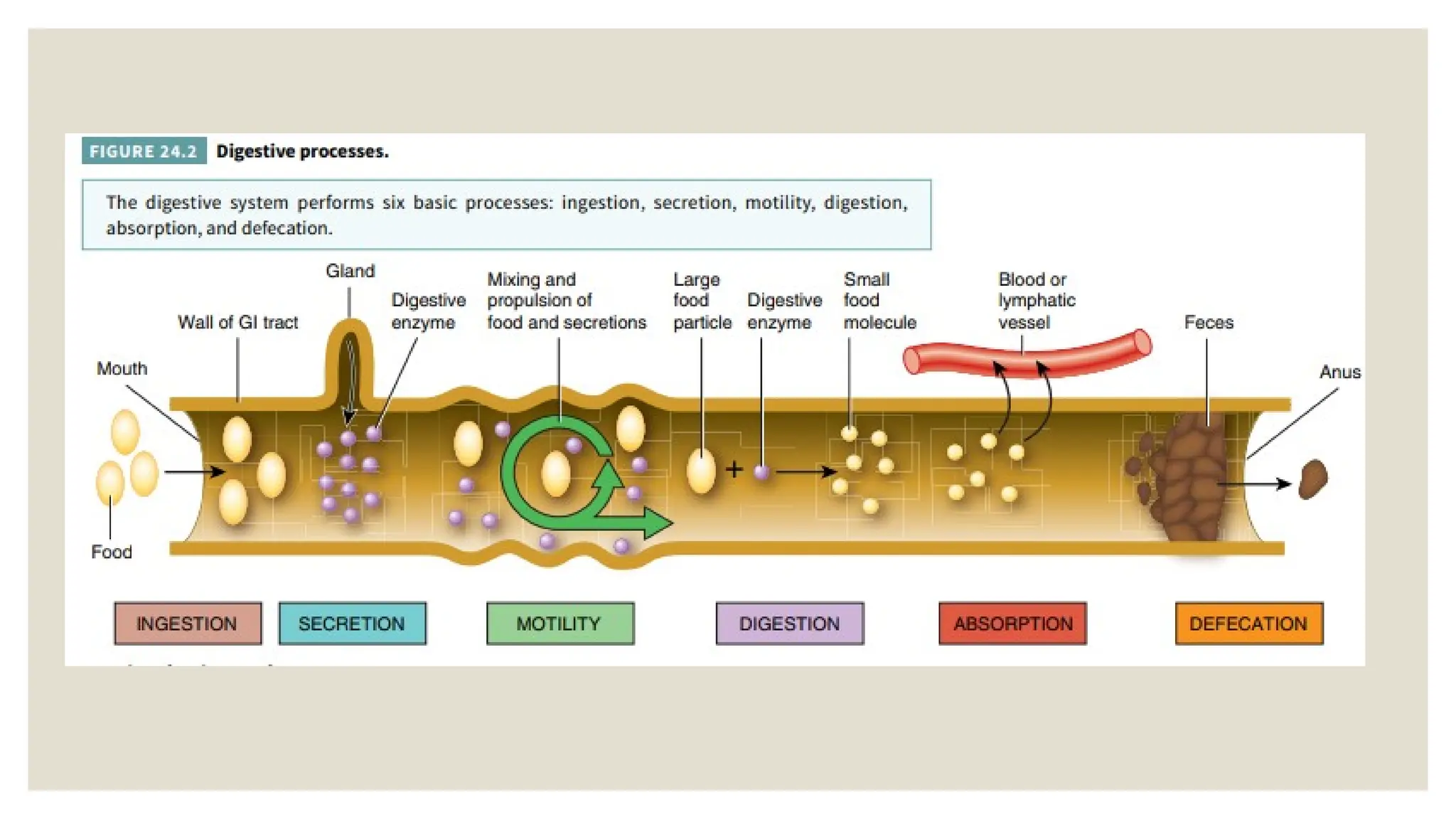
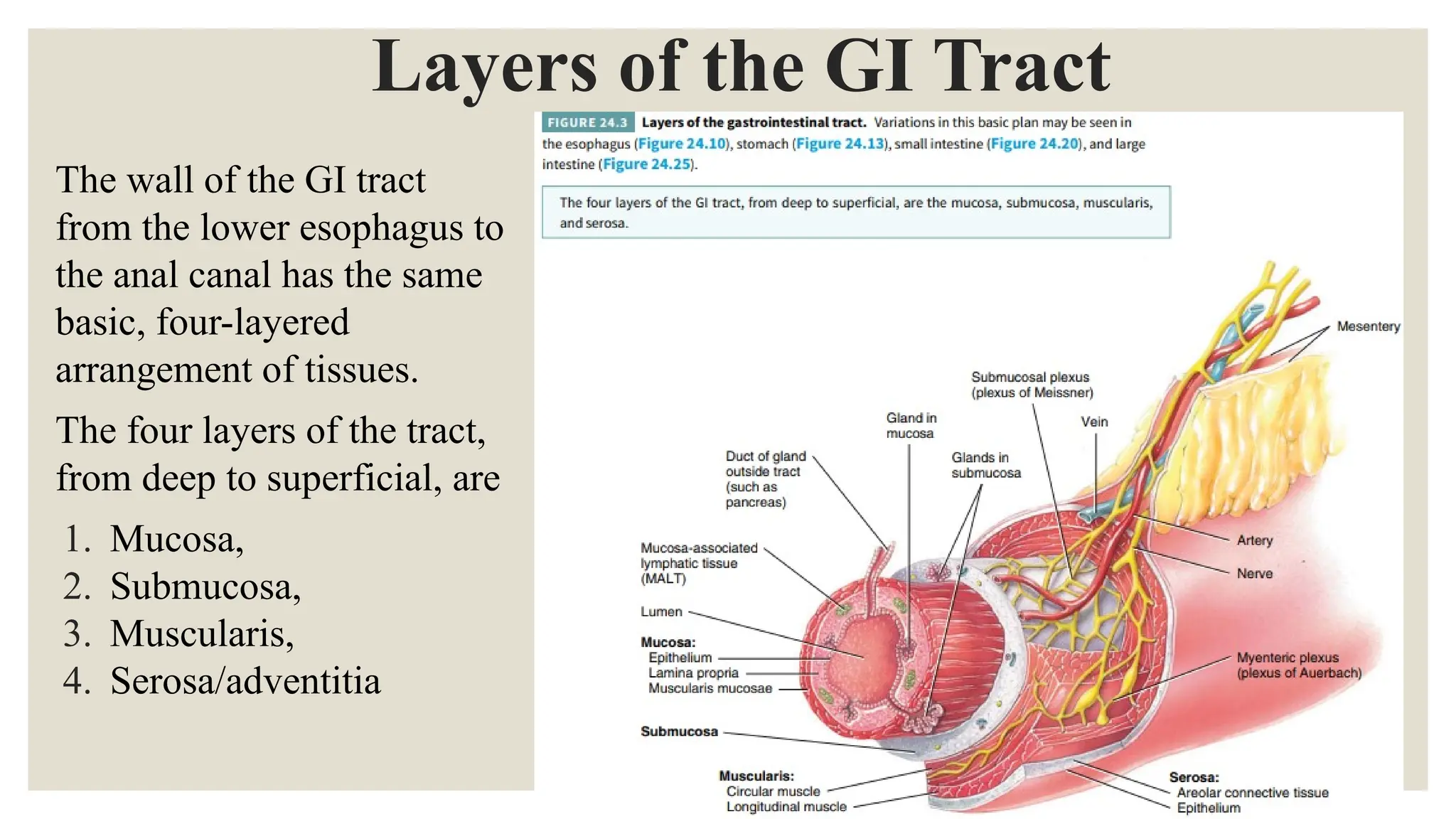
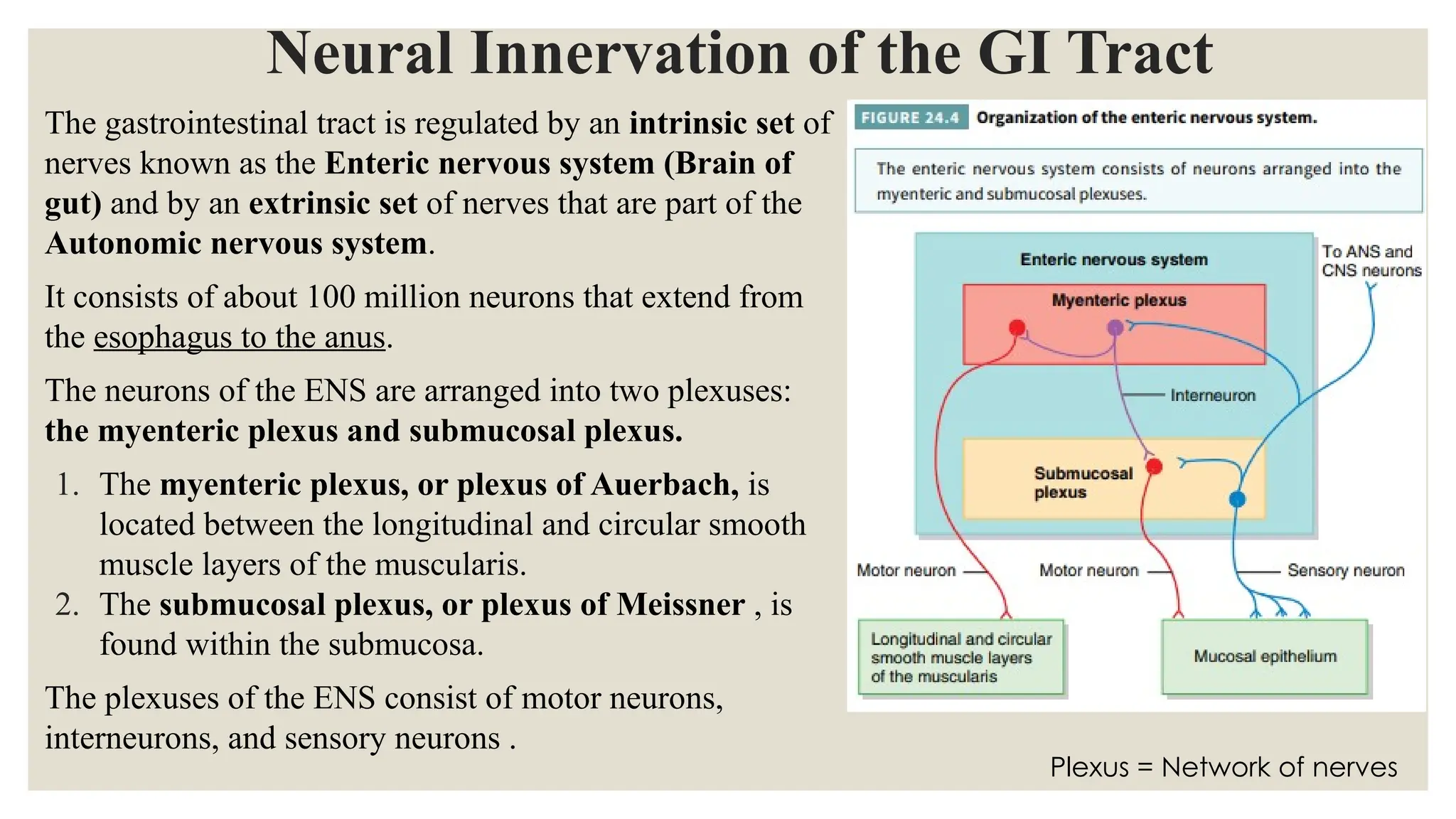
The document provides a comprehensive overview of the anatomy and physiology of the digestive system, outlining the structure and functions of the gastrointestinal (GI) tract and accessory digestive organs. It details the digestive processes including ingestion, secretion, motility, digestion, absorption, and defecation, along with the four-layered arrangement of tissues in the GI tract and the neural innervation by the enteric nervous system. Additionally, the document discusses the effects of the autonomic nervous system on GI tract functions and the reflex pathways that regulate digestive processes.