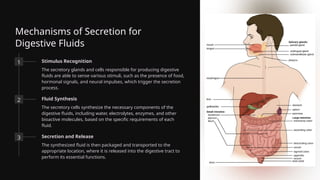
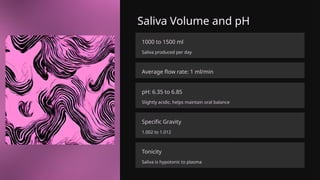
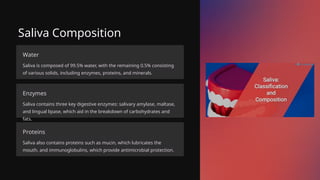
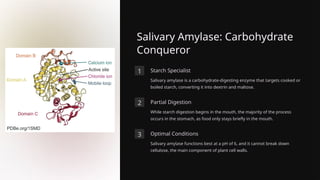
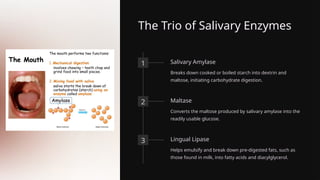
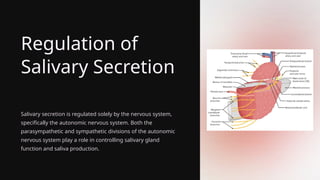
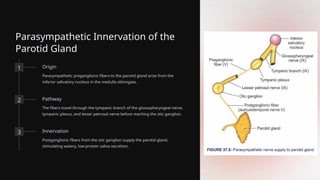
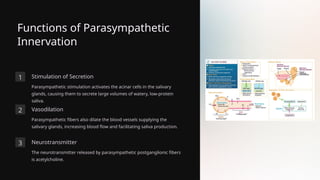
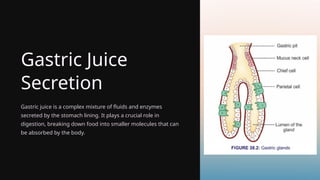
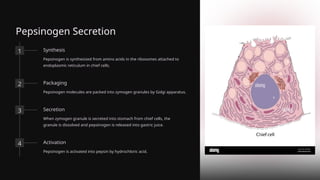
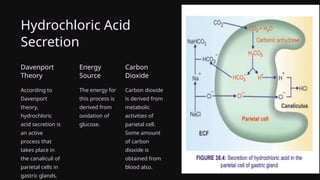
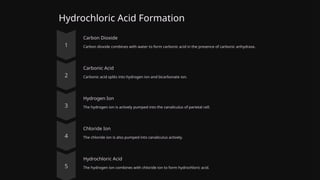
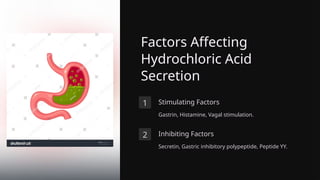
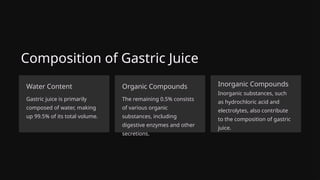
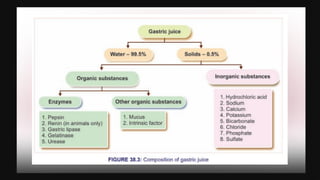
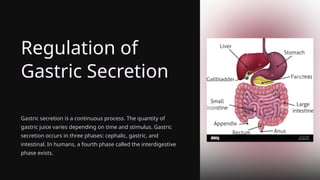
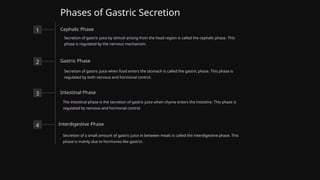
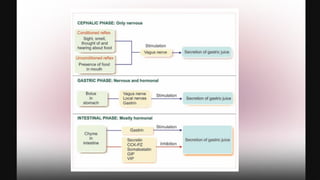
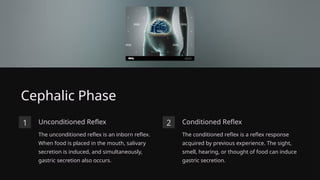
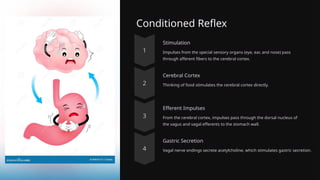
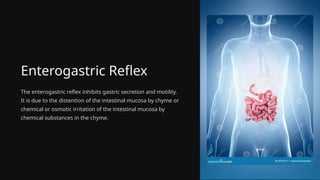
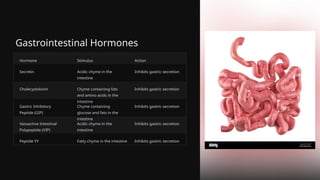
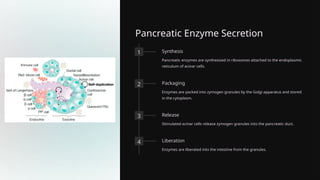
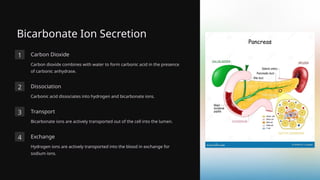
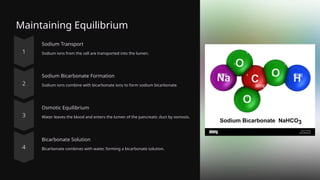
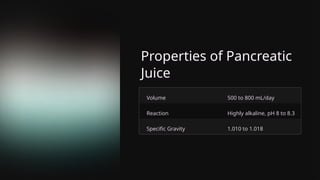
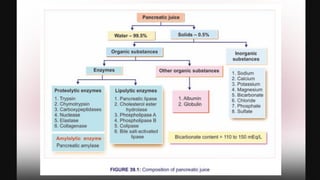
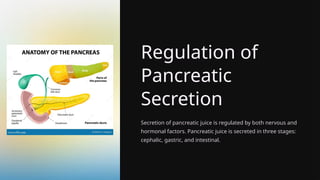
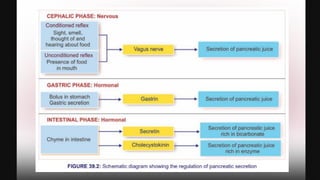
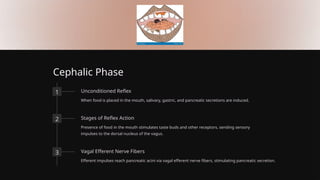
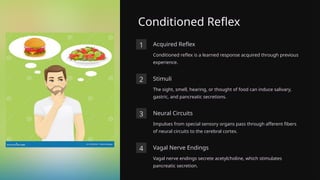
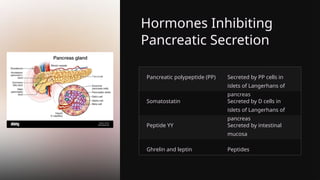
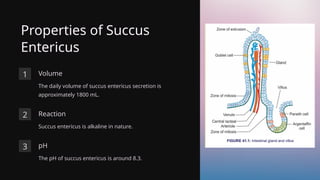
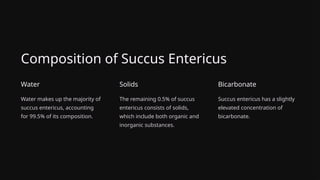
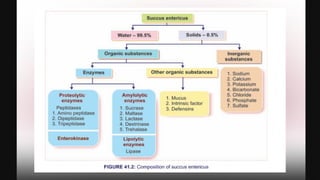
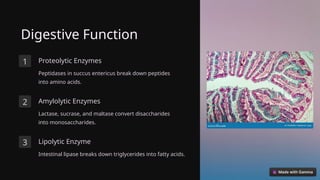
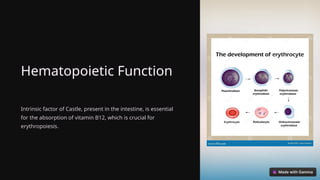
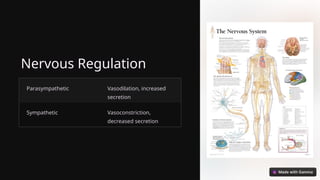
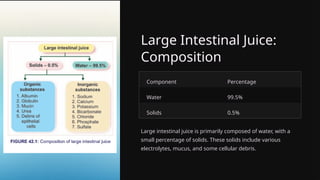
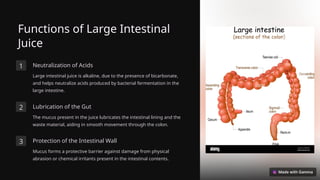
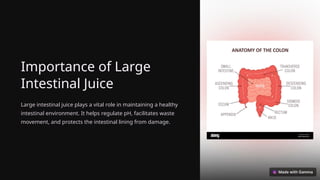
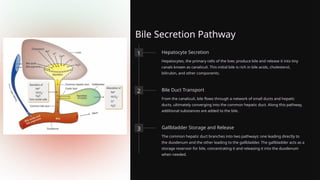
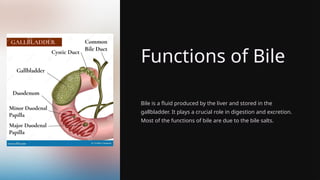
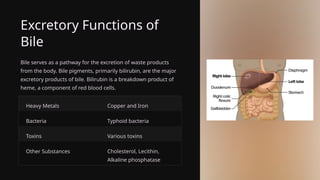
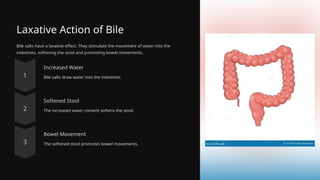
The document presents an in-depth analysis of digestive secretions, focusing on their roles, composition, mechanisms of secretion, and regulation within the human digestive system. It describes key fluids such as saliva, gastric juice, and others, detailing their components, functions, and the nervous system's role in managing secretion. The presentation serves as an educational resource on the importance of these fluids in digestion, absorption, and overall oral health.