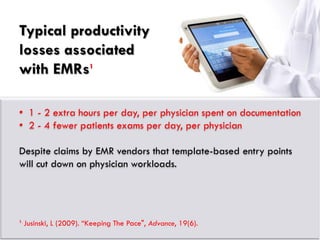
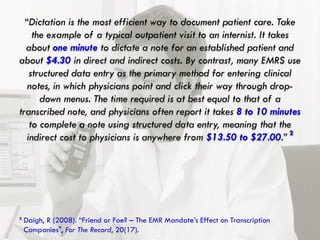
The document discusses the debate around replacing dictation with electronic medical record (EMR) systems. While EMRs promise benefits from automation and subsidies, replacing established dictation workflows with rigid EMR templates can significantly reduce physician productivity. Integrating flexible digital dictation systems that allow narrative notes with EMRs may offer the best of both technologies by maintaining productivity while gaining paperless benefits. The key is finding solutions that adapt to existing workflows rather than disrupt them.