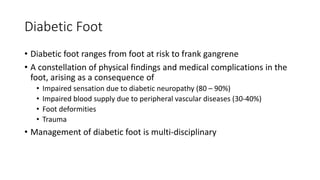
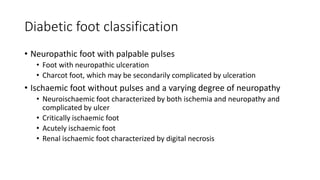
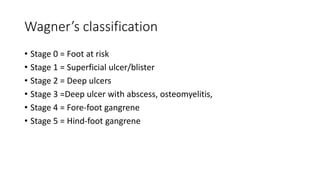
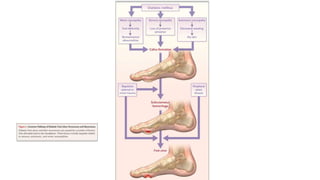
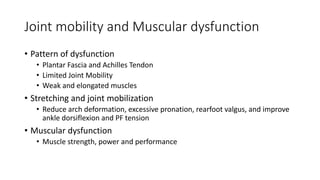
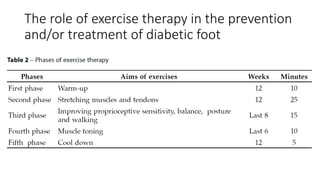
Diabetic foot results from neuropathy, vascular disease, foot deformities, and trauma which impair sensation and blood flow. It ranges from feet at risk to gangrene. Exercise therapy can help prevent and treat diabetic foot by reducing neuropathy and vascular disease risks, improving joint mobility and muscle strength, and enhancing balance and gait. A multi-disciplinary approach including exercises is needed to manage diabetic foot given its increasing problem and high costs, with the goal of prevention to spare feet for as long as possible.