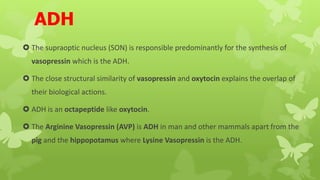
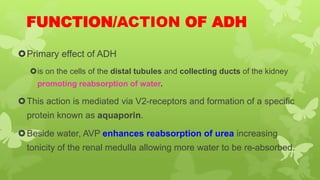
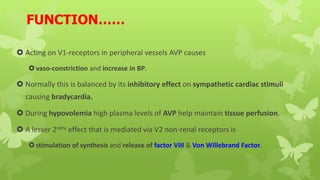
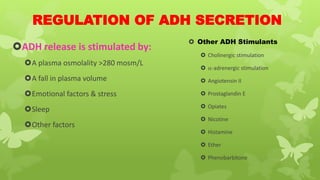
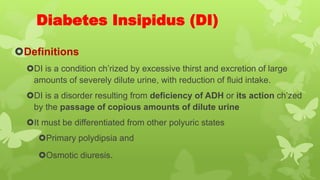
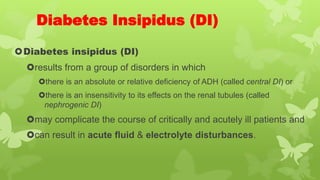
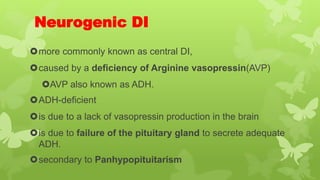
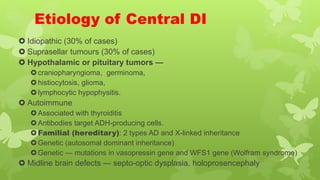
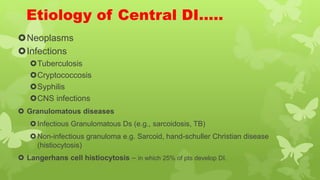
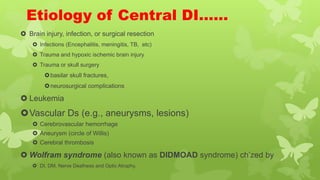
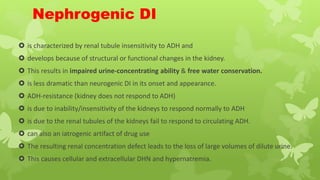
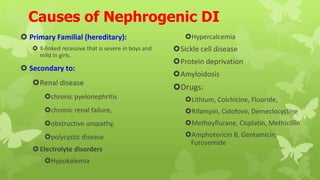
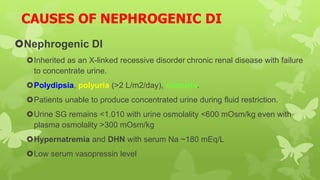
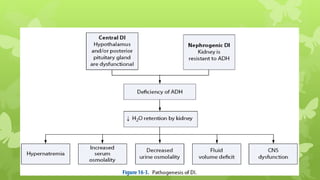
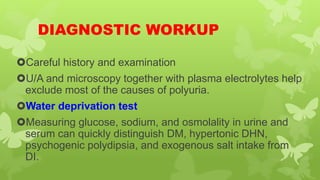
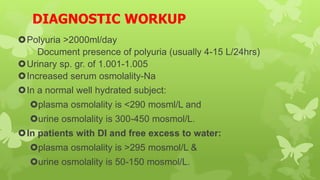
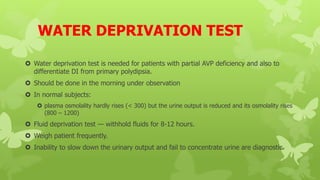
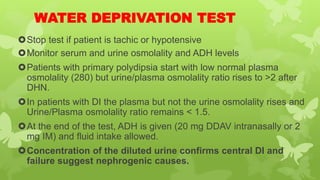
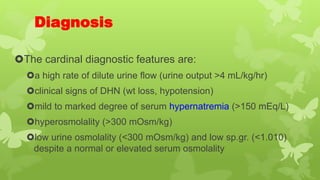
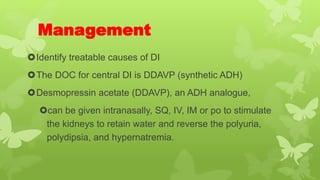
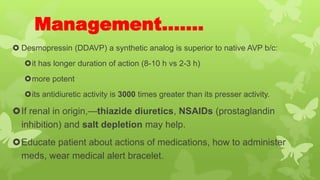
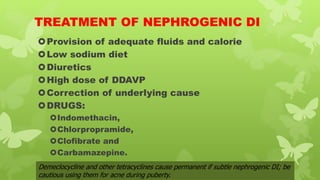
This document provides an overview of disorders of the pituitary gland, with a focus on diabetes insipidus. It defines diabetes insipidus as a condition characterized by excessive thirst and urine output. It describes the two main types as central/neurogenic DI, caused by a deficiency of the antidiuretic hormone ADH, and nephrogenic DI, caused by the kidneys' insensitivity to ADH. The document discusses the causes, symptoms, diagnostic process involving water deprivation tests, and management typically involving the ADH analogue desmopressin.