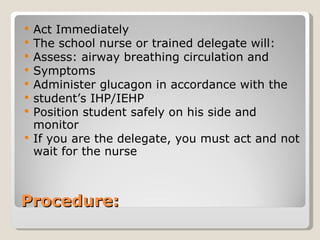
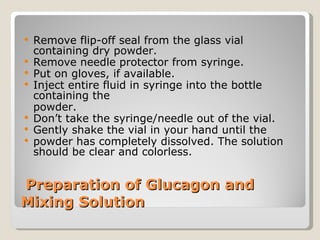
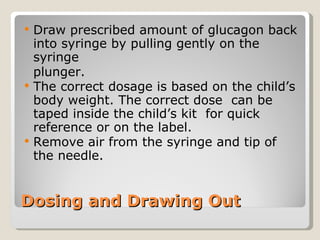
This document provides information about diabetes and how to care for students with diabetes in schools. It discusses what diabetes is, signs and symptoms of low and high blood sugar, new laws regarding diabetes care in schools, what glucagon is and how it is used to treat severe low blood sugar, proper storage and administration of glucagon, and what to do after administering glucagon. The overall purpose is to educate about diabetes and establish protocols for providing care to students with diabetes in schools.