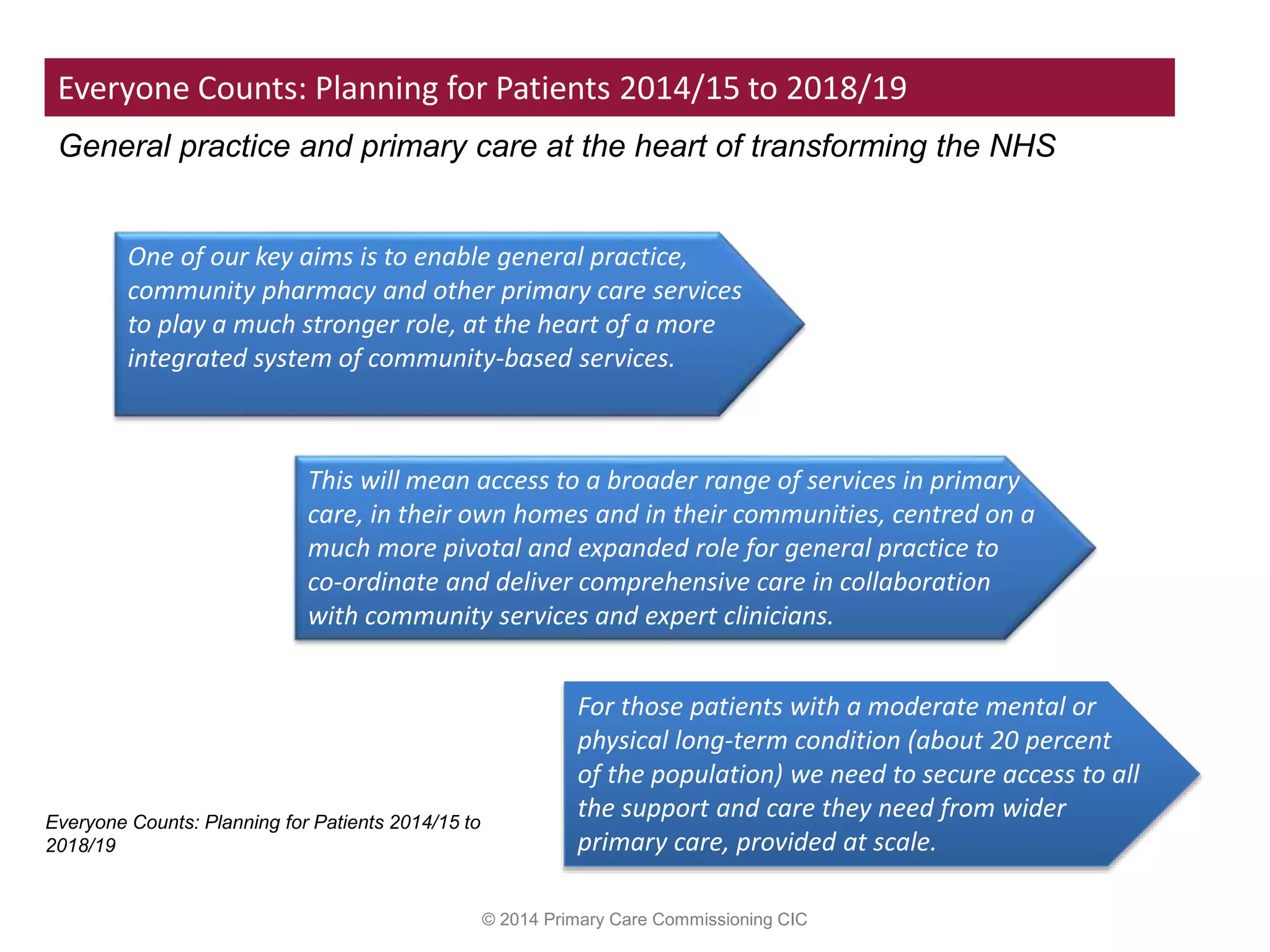
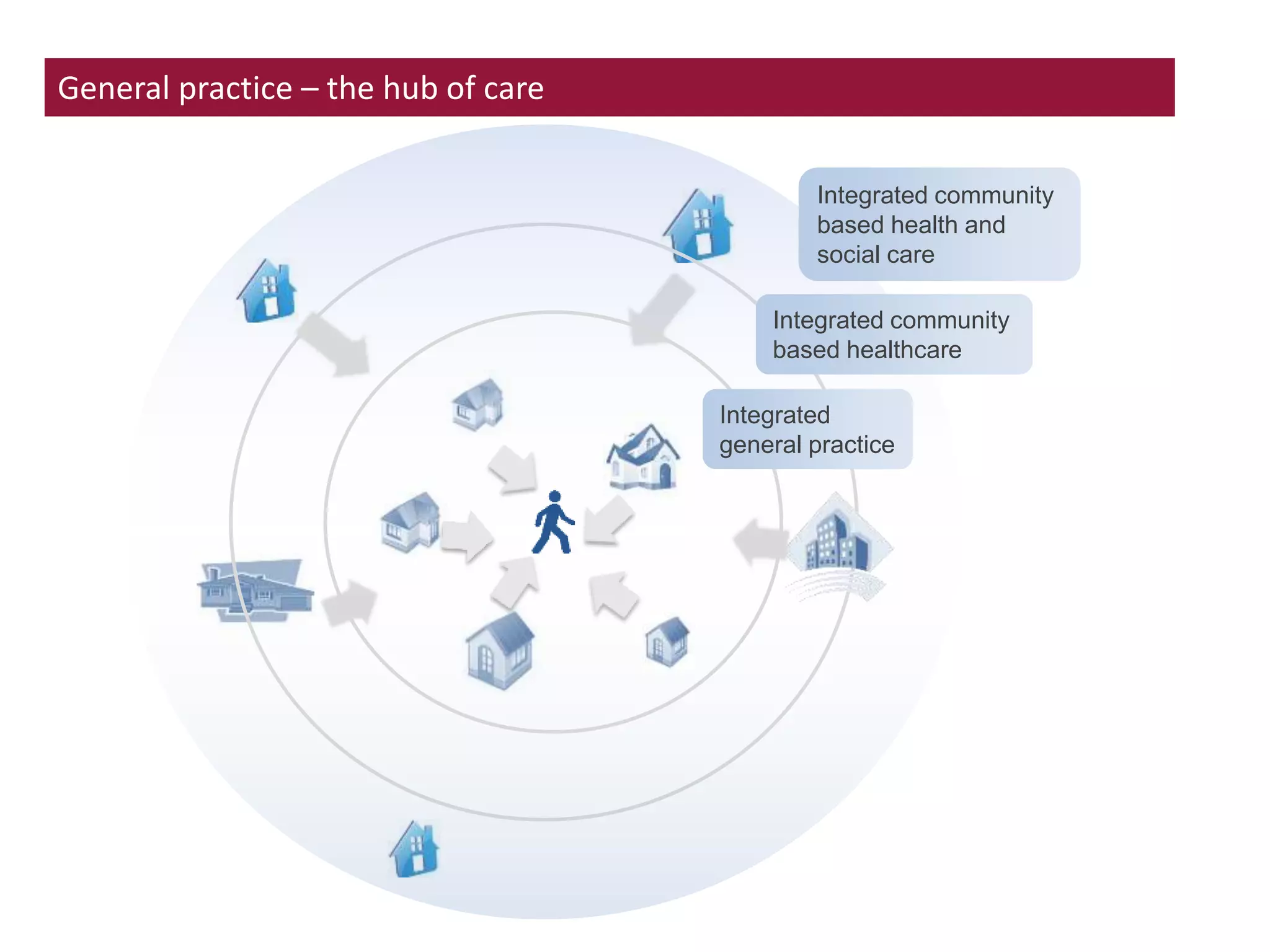
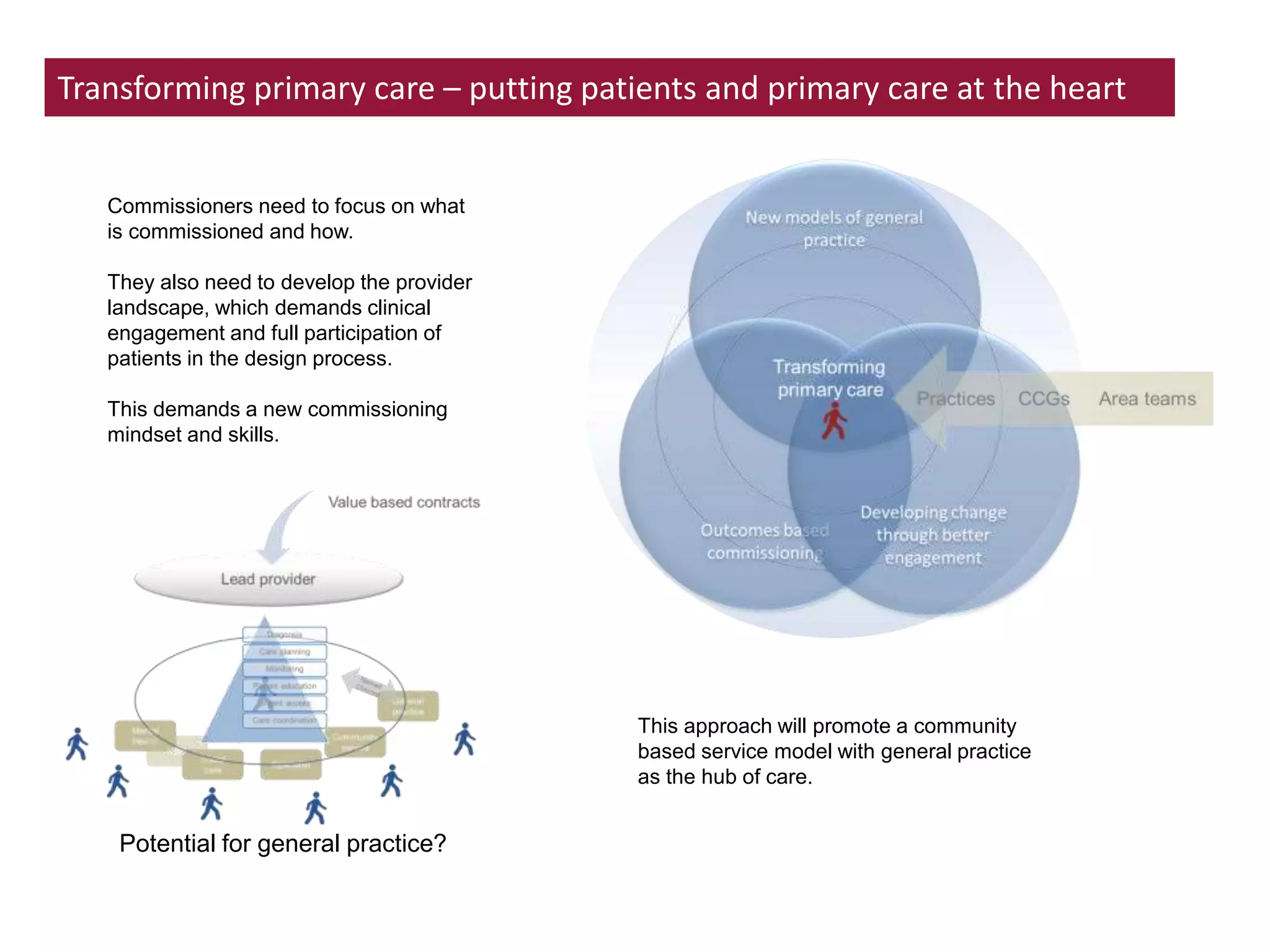
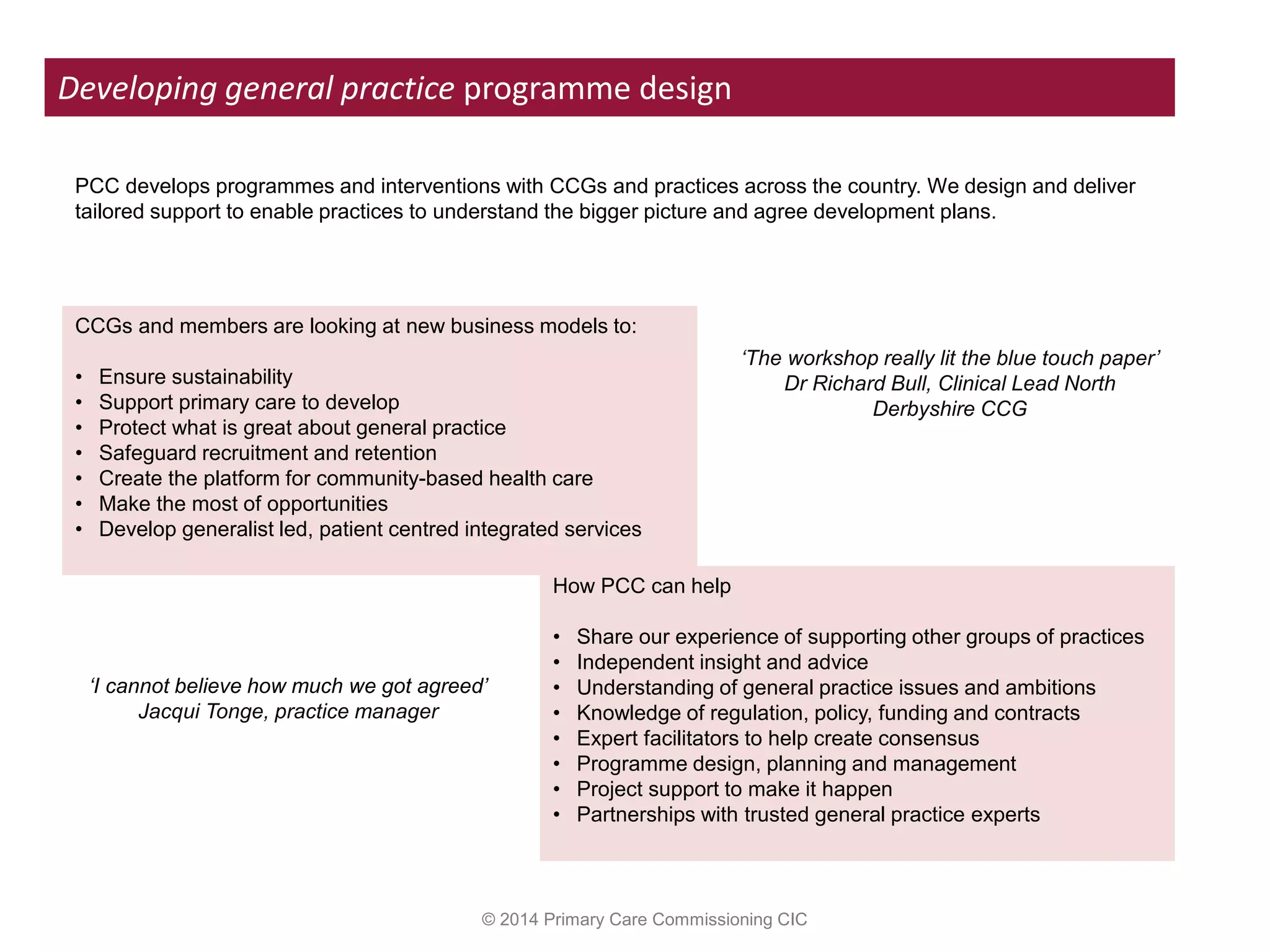
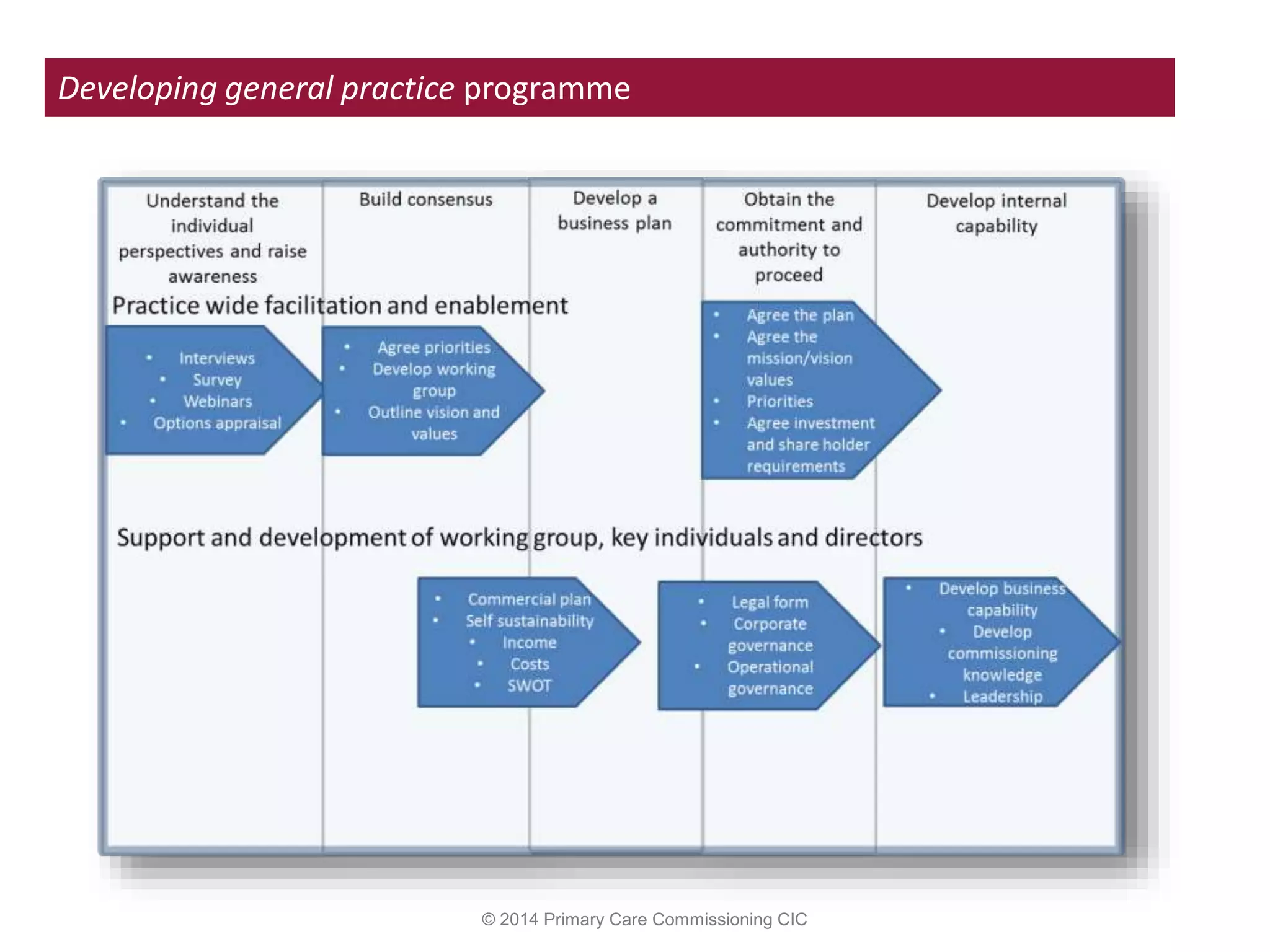
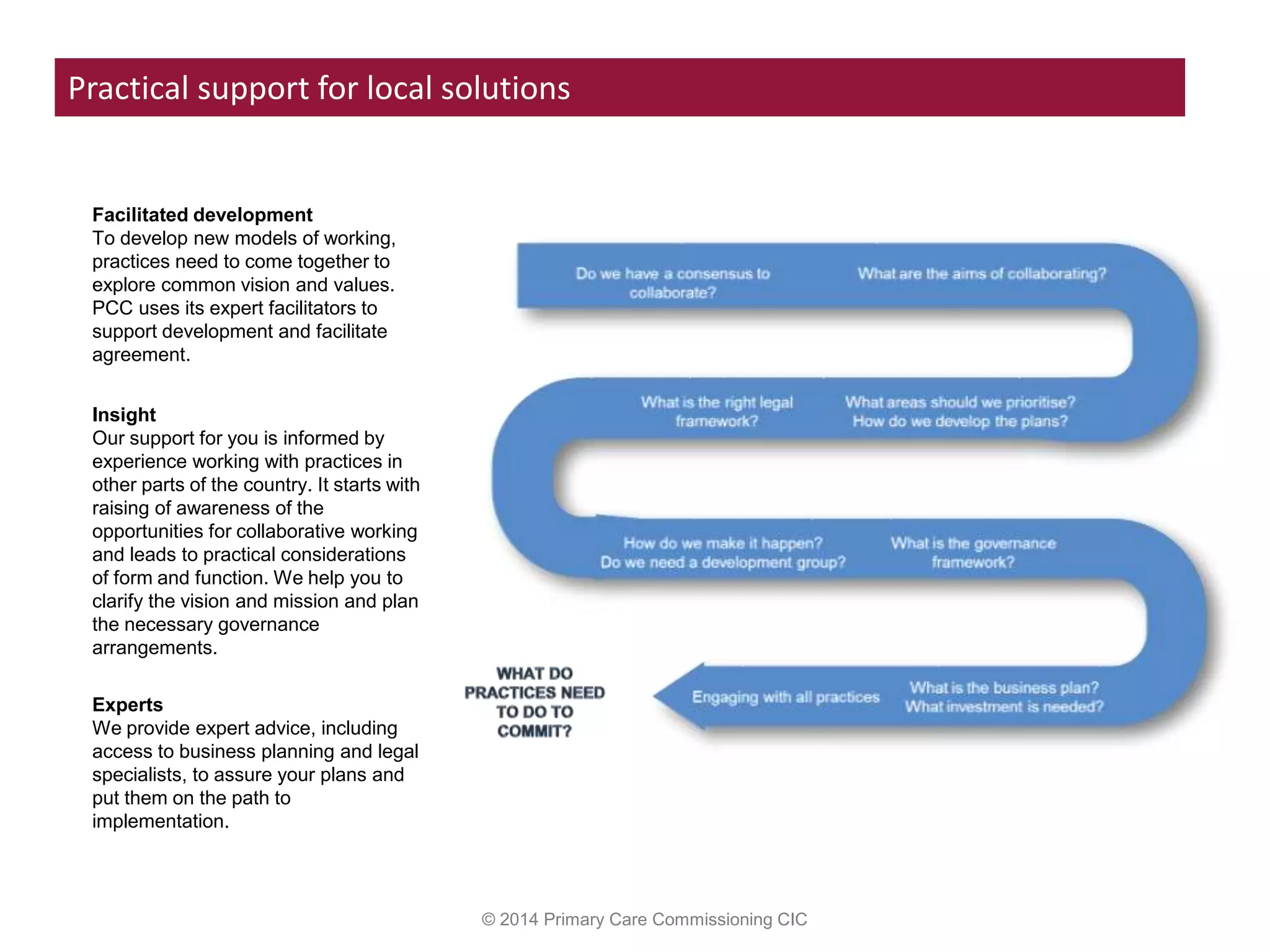
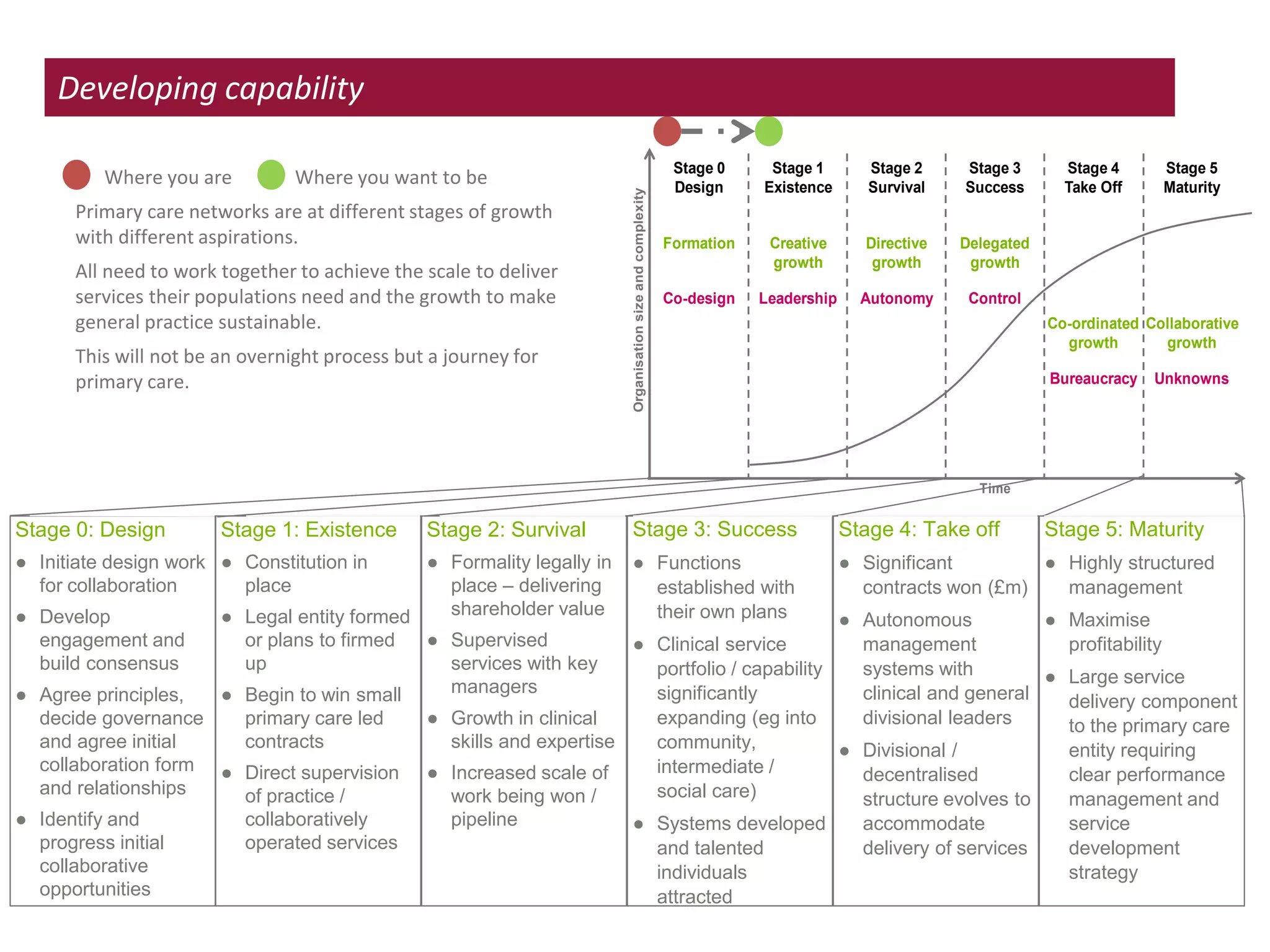
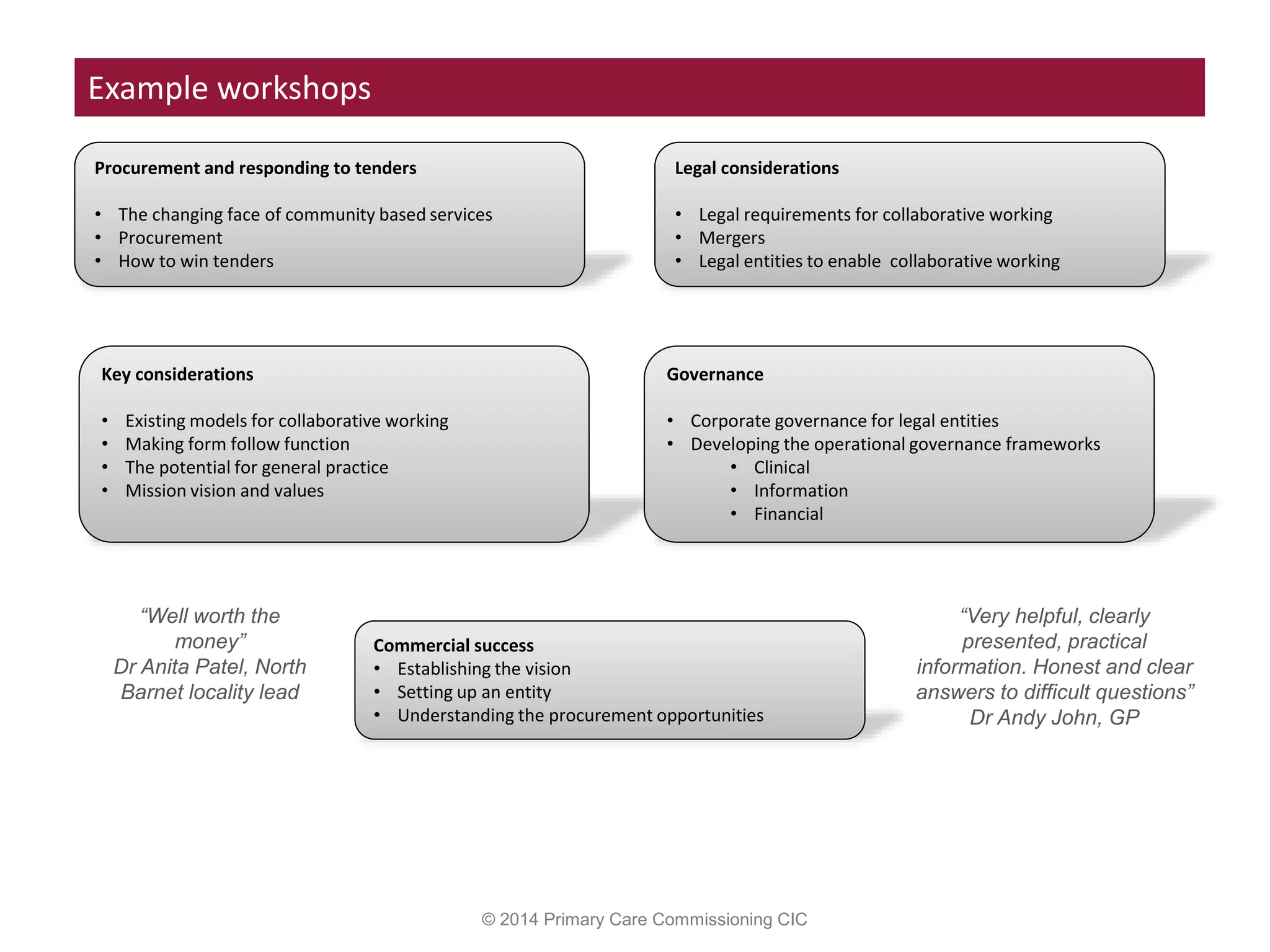
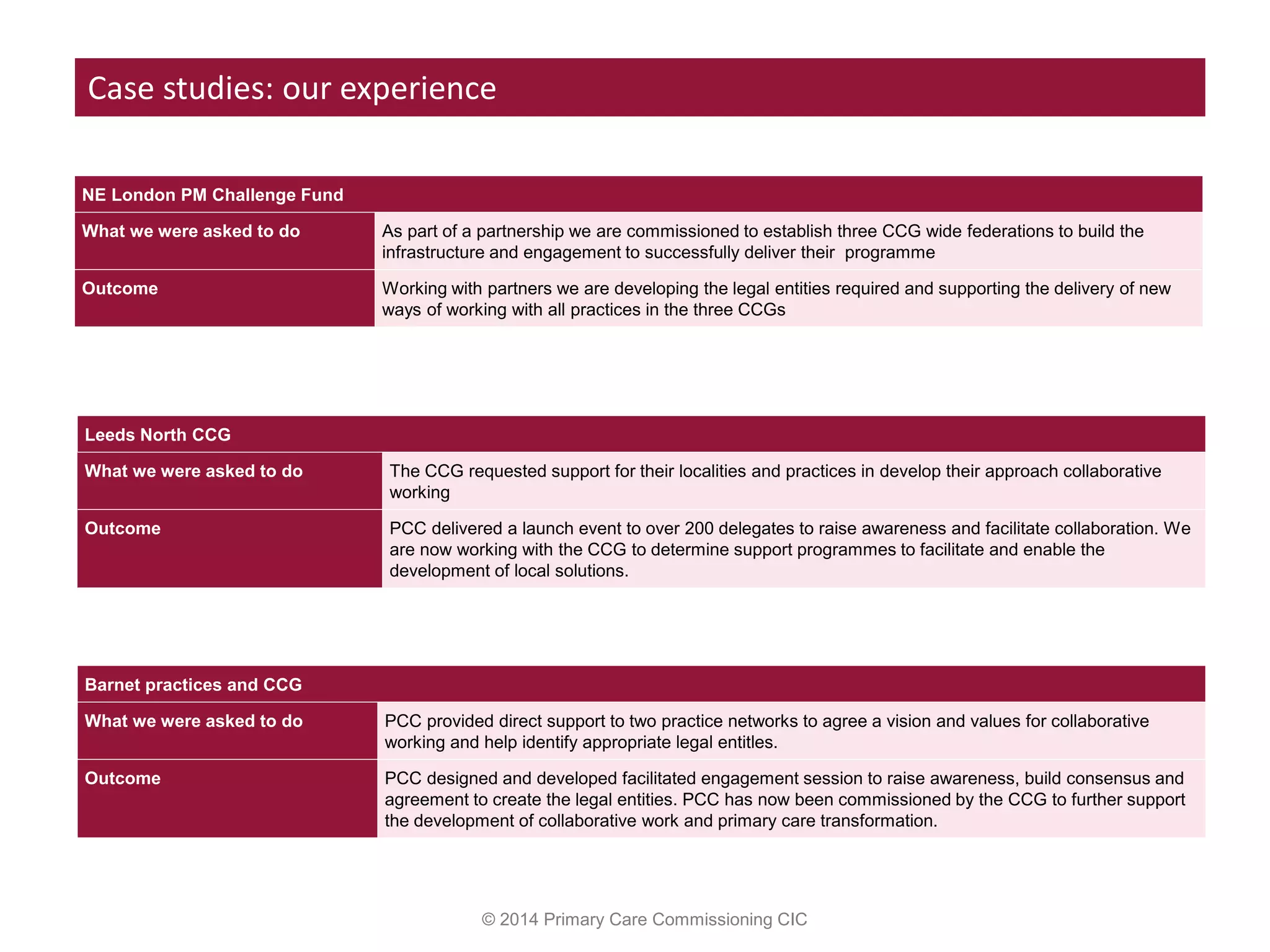
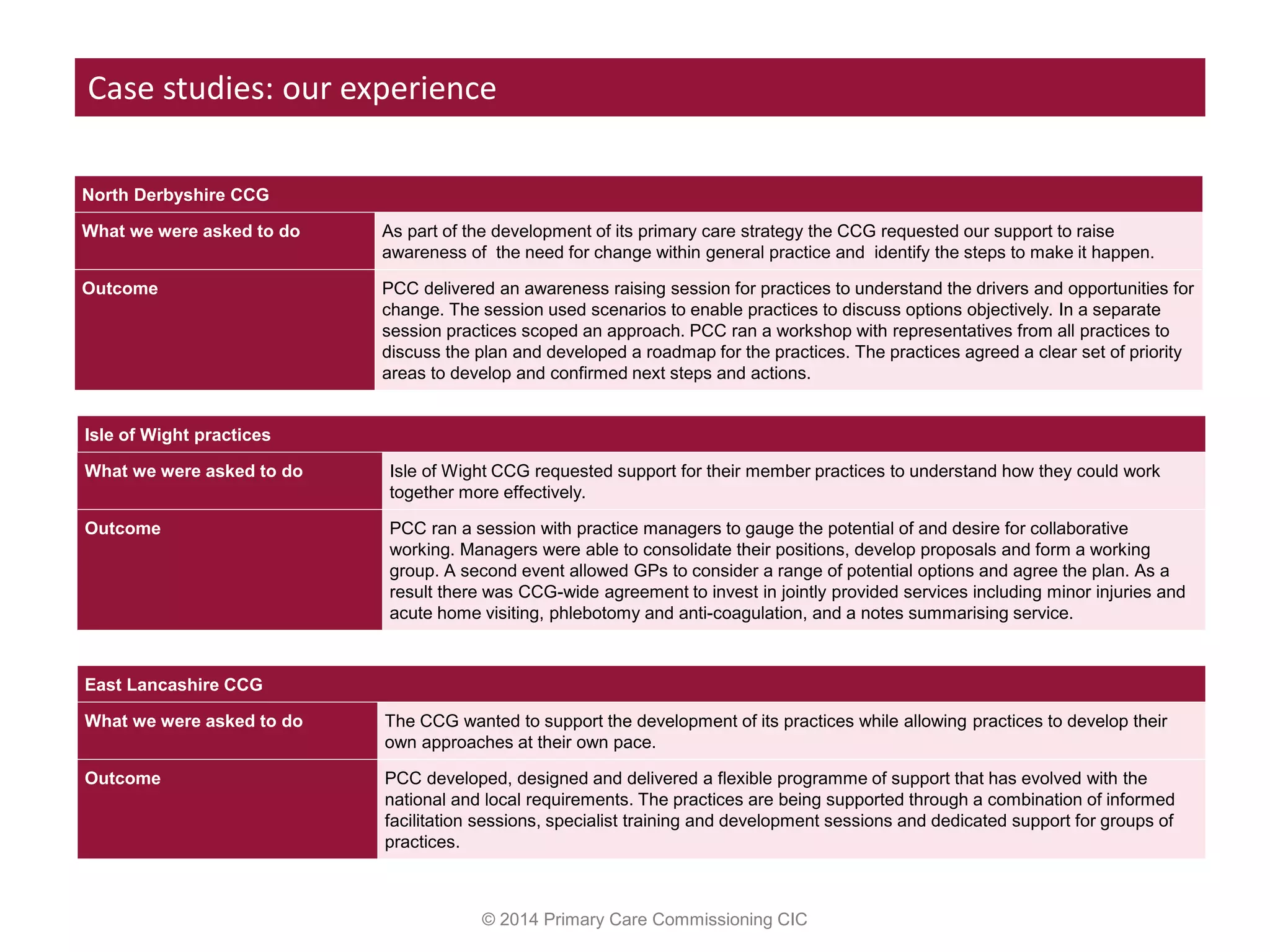
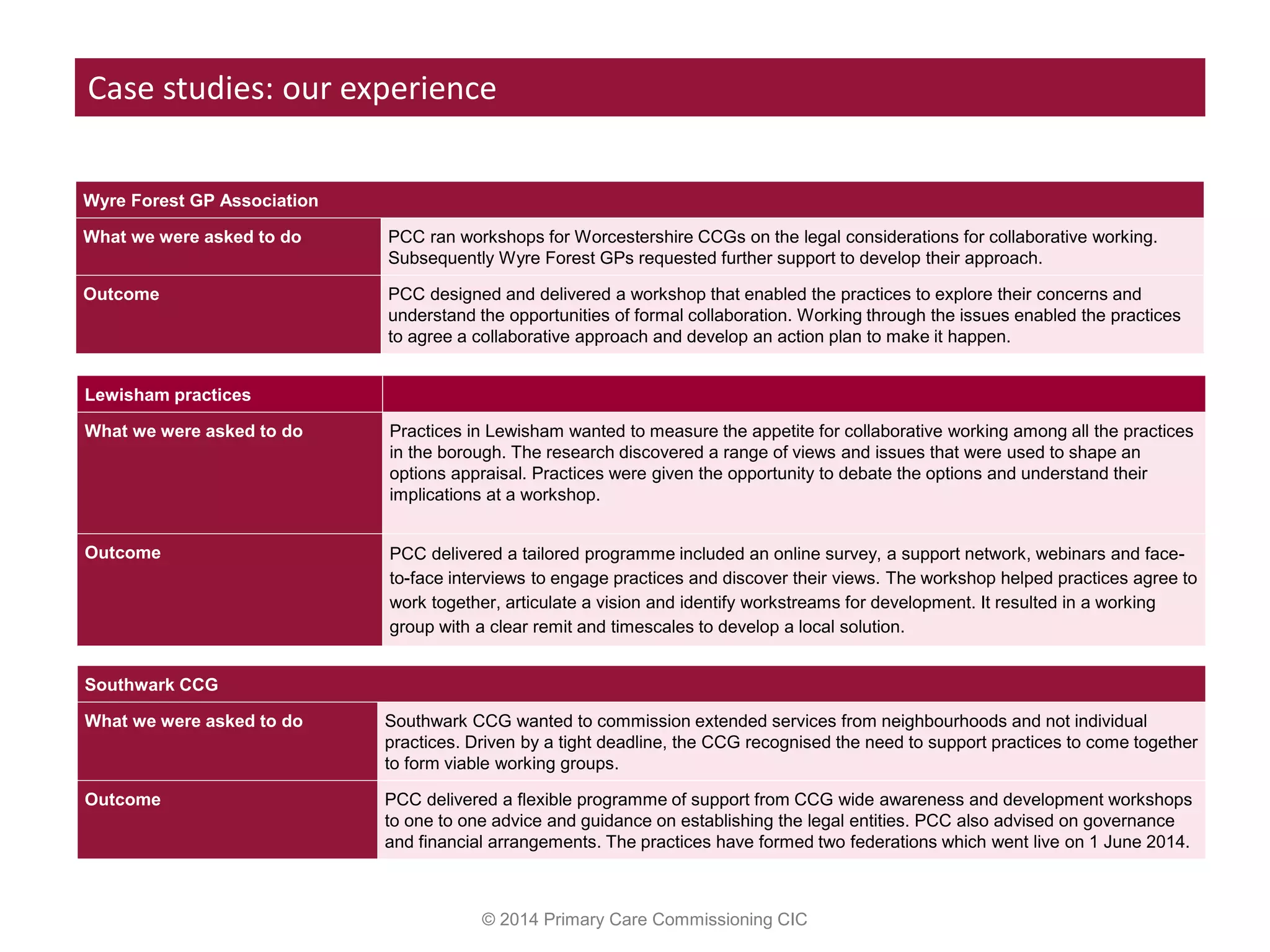
This document discusses transforming primary care by putting patients and primary care at the heart of the healthcare system. It advocates for a more integrated system with general practice coordinating comprehensive care in collaboration with community services. For patients with long-term conditions, the goal is to secure access to all necessary primary care and community support. Commissioners need to focus on what is commissioned and how, developing new provider models with clinical and patient engagement. This will promote a community-based service model with general practice as the central hub of care. The Primary Care Commissioning CIC can help by facilitating agreement among practices to develop new collaborative models through their expertise and experience supporting other practices.