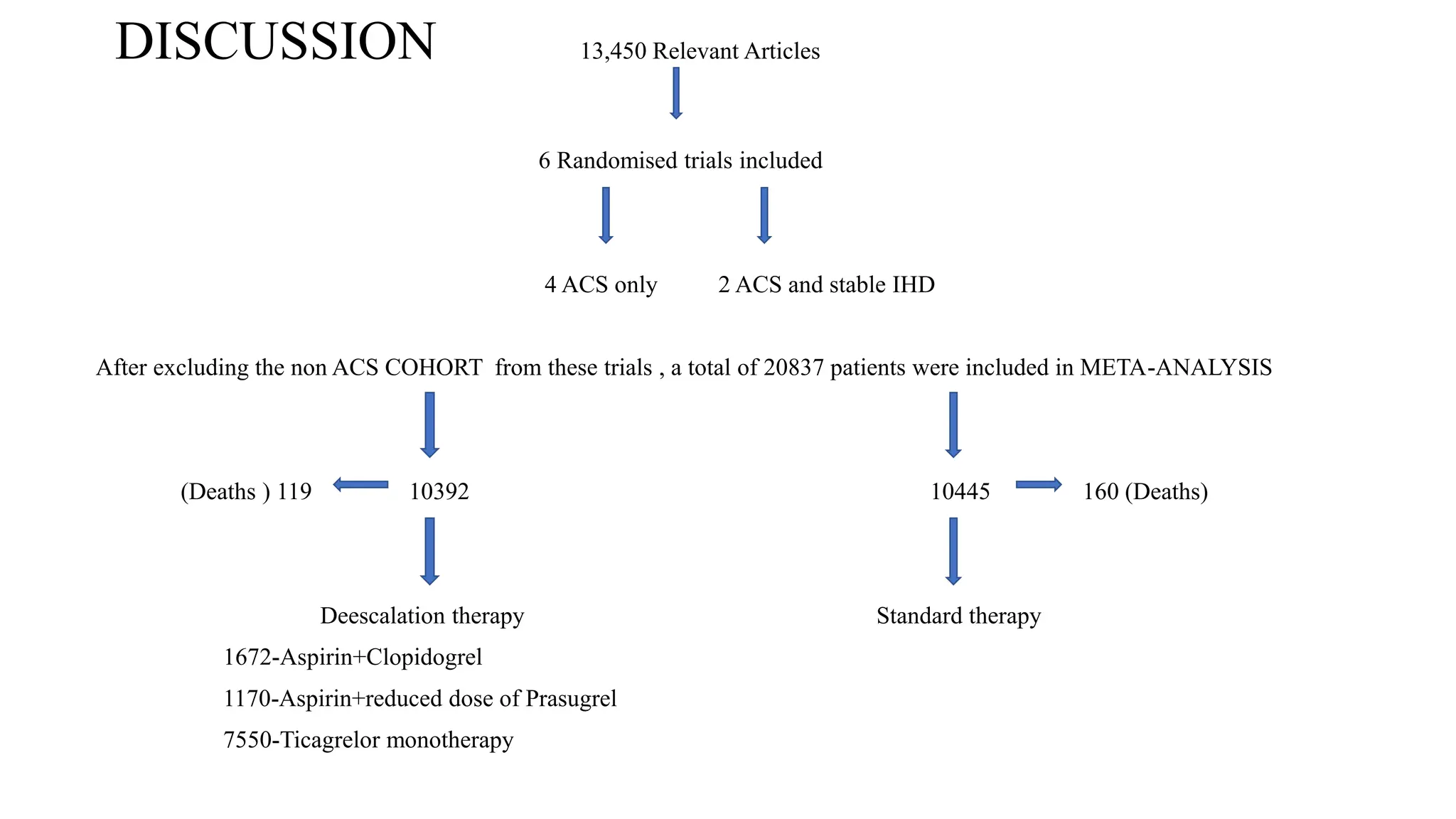
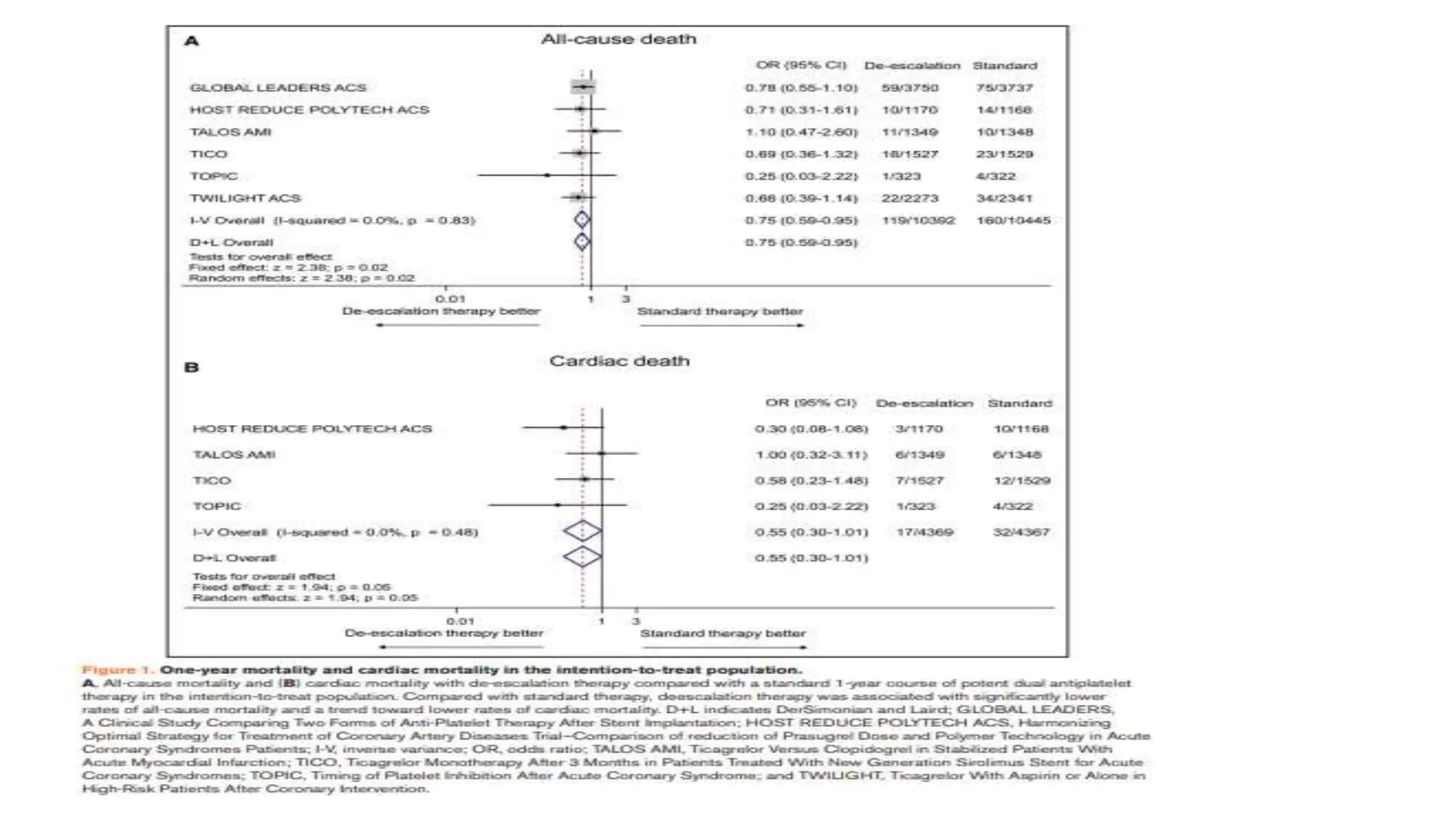
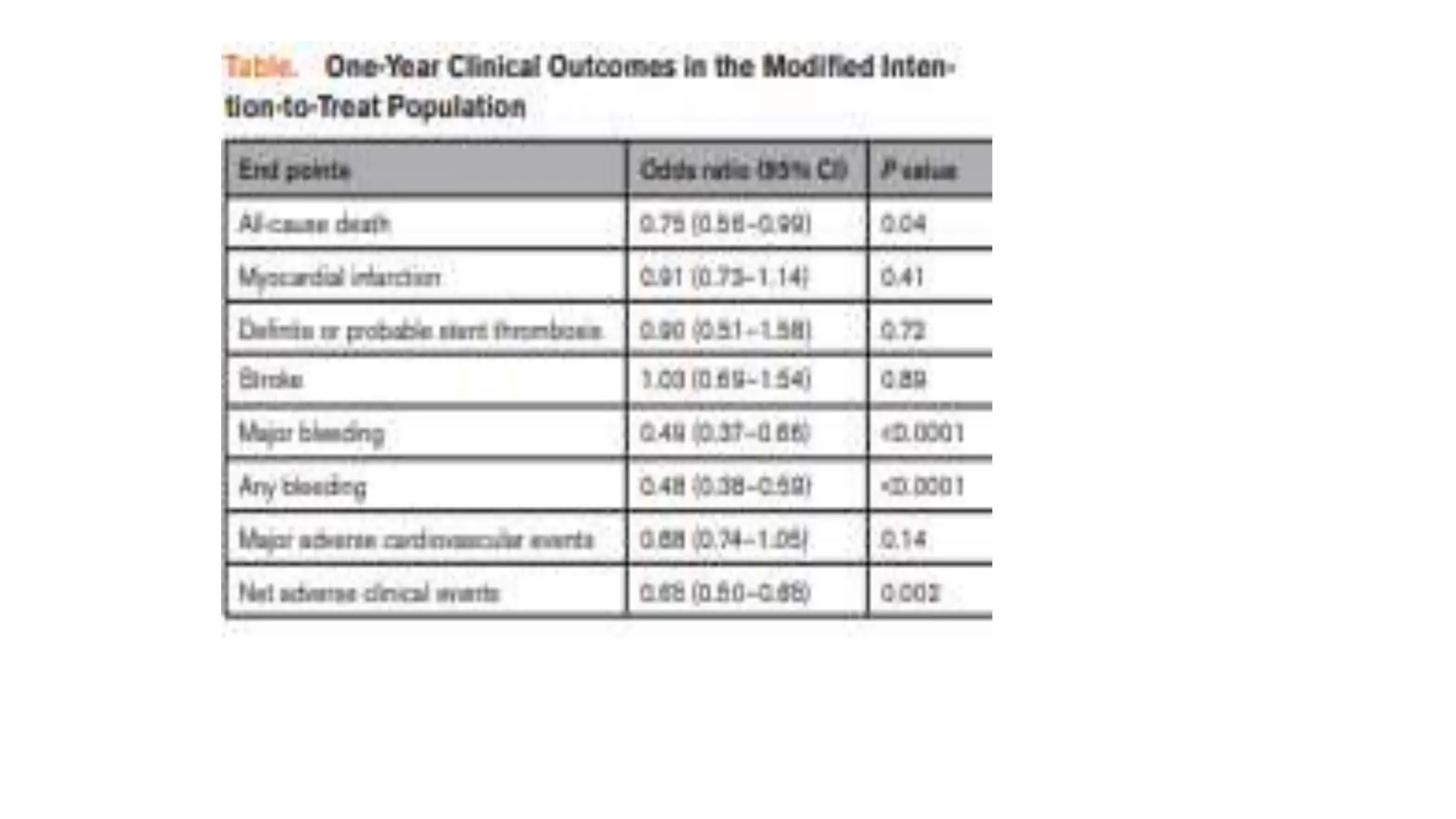
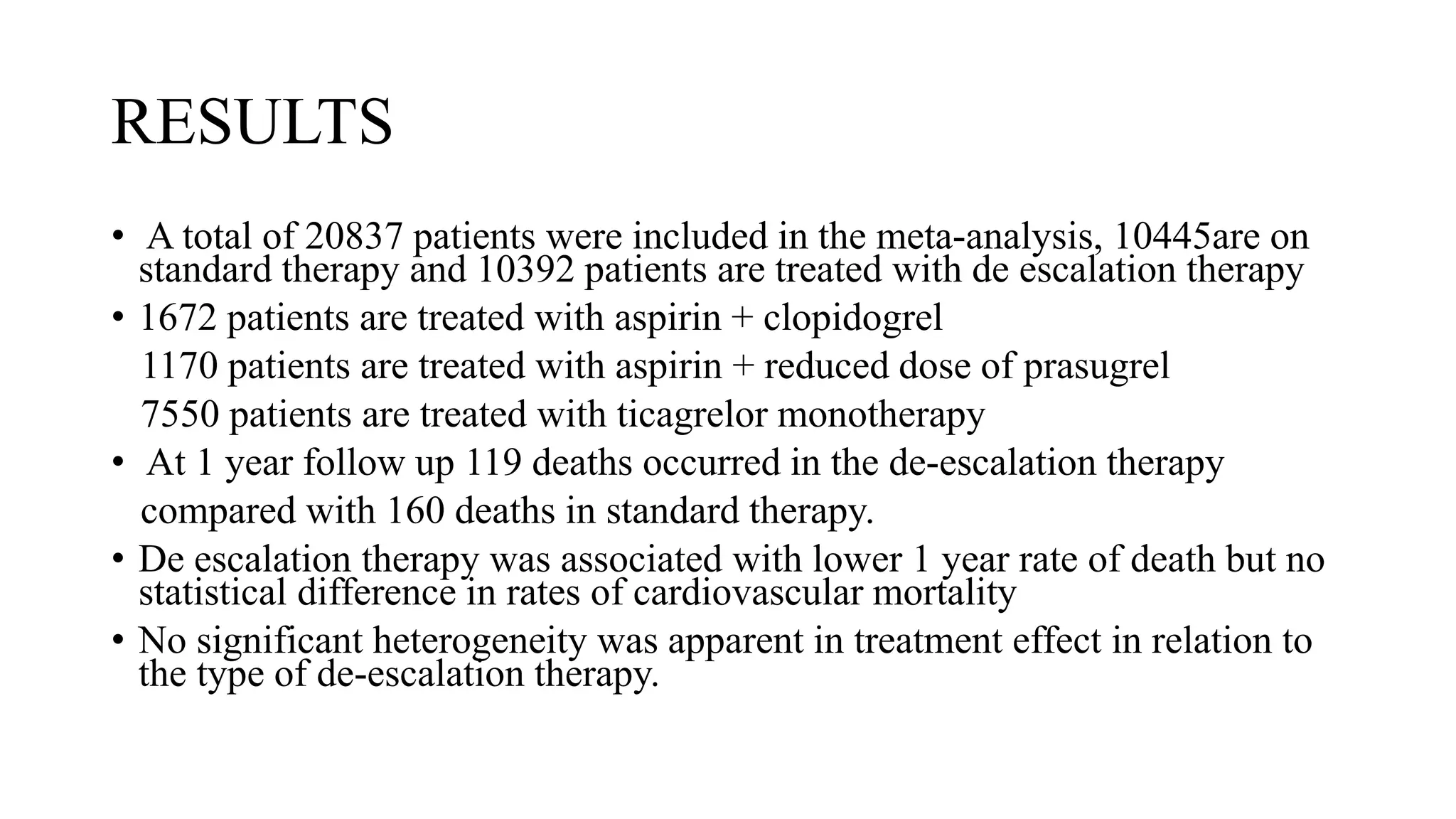
This journal club discusses a meta-analysis of 6 randomized controlled trials including over 20,000 patients with acute coronary syndrome undergoing percutaneous coronary intervention. The meta-analysis compared outcomes of standard potent dual antiplatelet therapy (DAPT) for 1 year to de-escalation strategies involving 1-3 months of potent DAPT followed by less potent DAPT or ticagrelor monotherapy. The results showed de-escalation therapy was associated with lower rates of all-cause mortality, major bleeding, and net adverse clinical events at 1 year, with no difference in cardiovascular mortality. However, the study was unable to examine timing of survival differences or identify subgroups that may benefit more from de-escalation