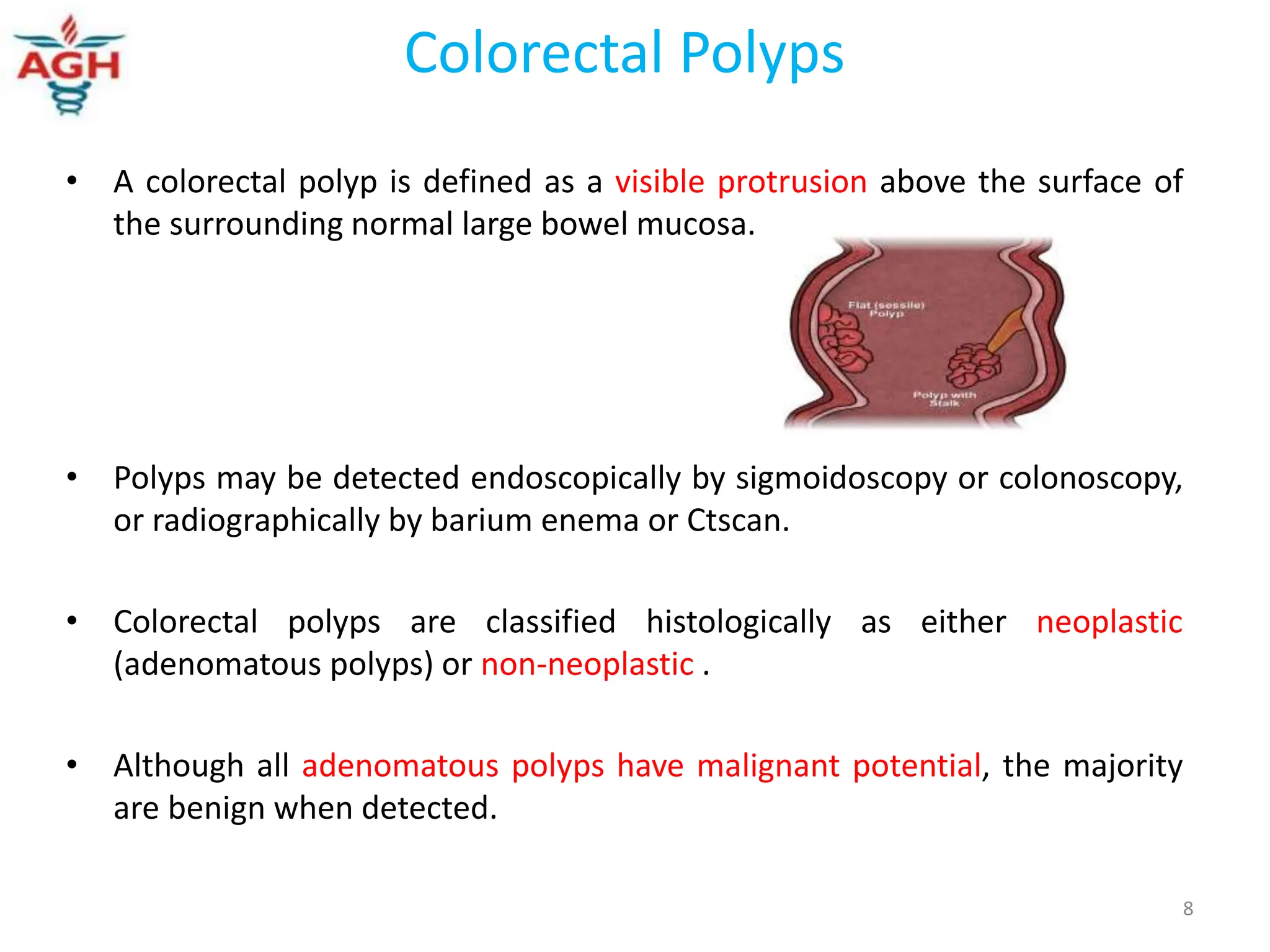
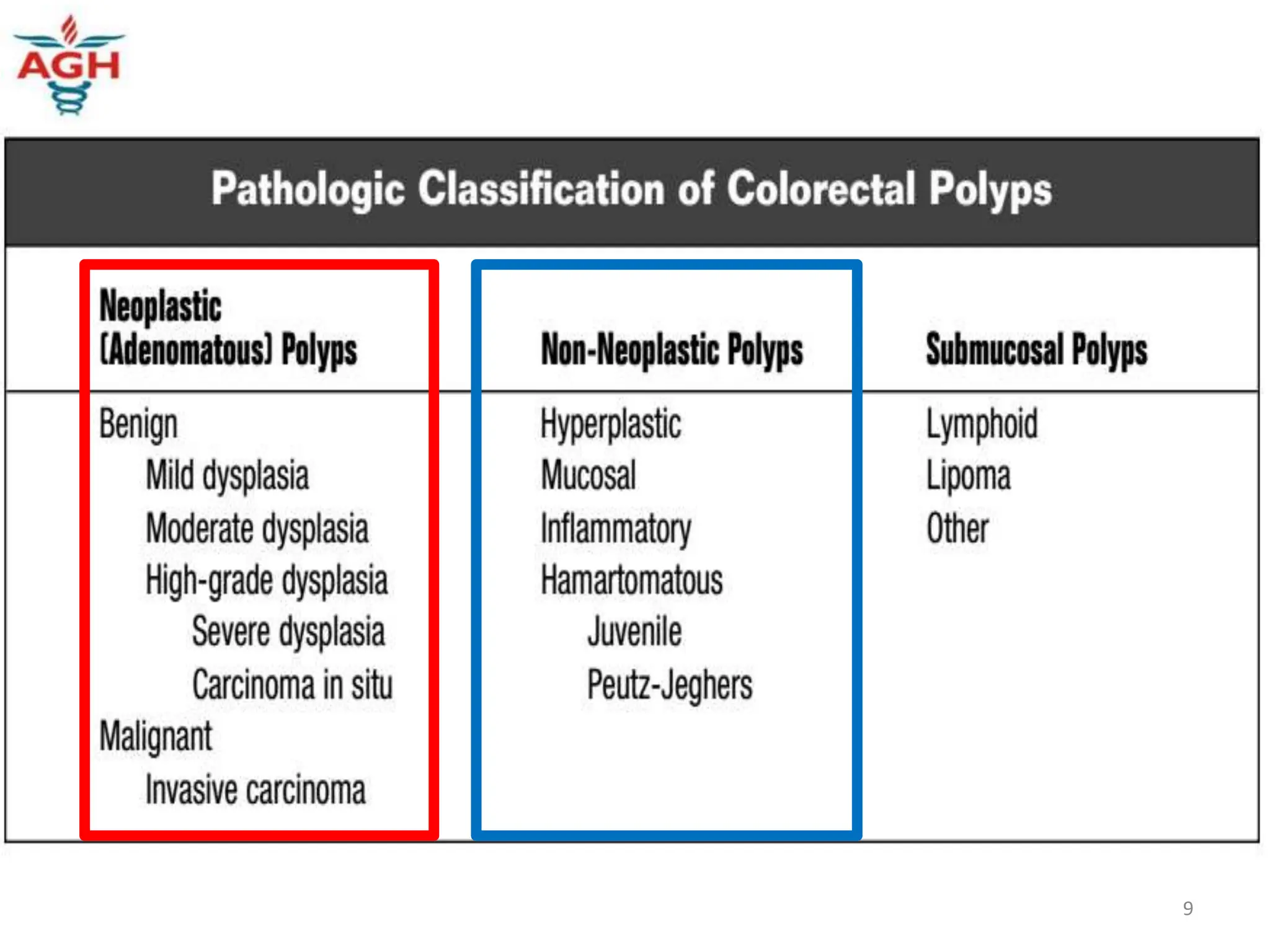
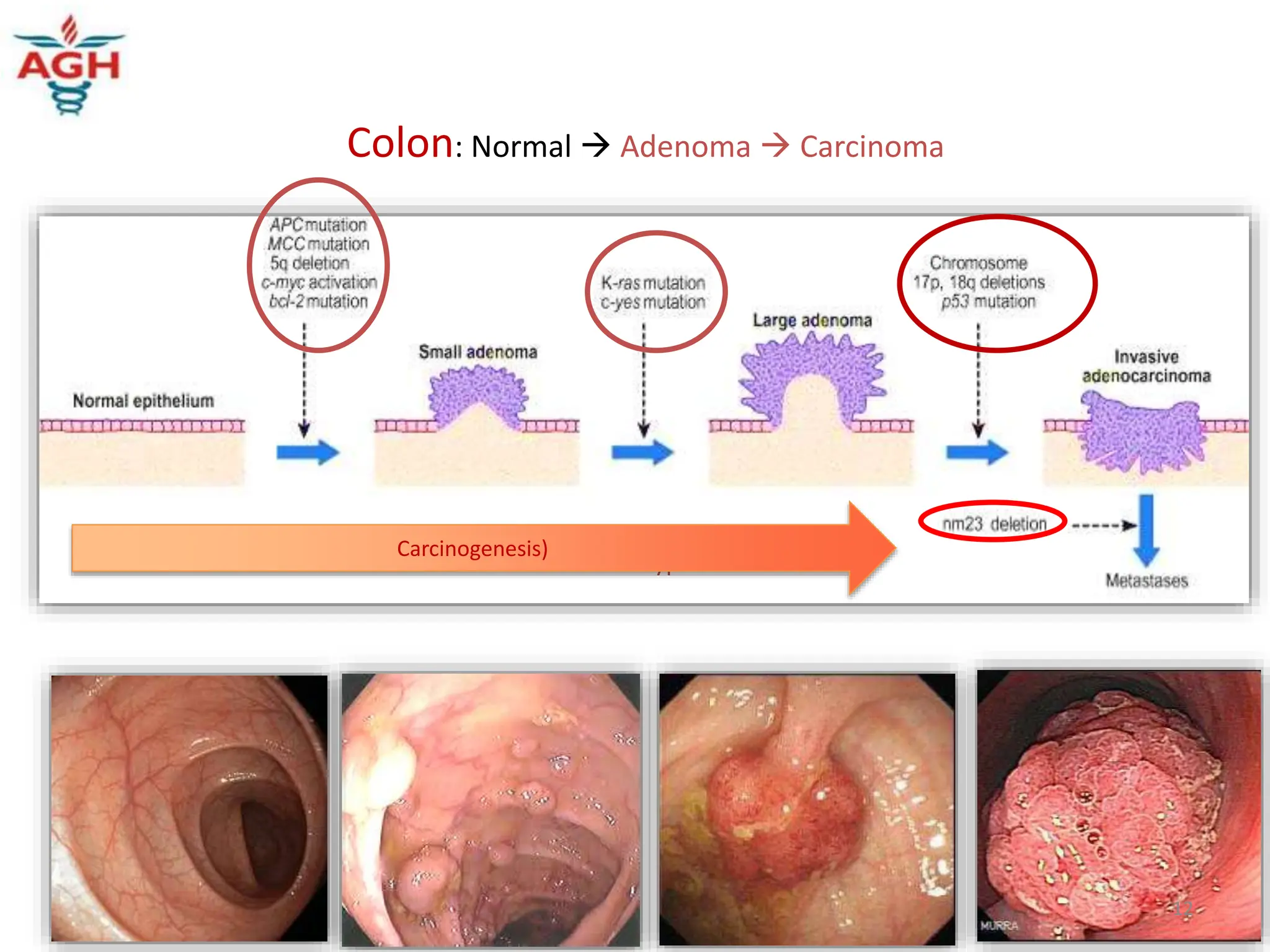
Colonoscopic polypectomy is a common procedure to remove colonic polyps. Polyps may develop into colon cancer over time through the adenoma-carcinoma sequence. Screening tools like colonoscopy allow for detection and removal of polyps, preventing progression to cancer. Risk factors for colon polyps include obesity, diet high in red and processed meats, smoking, and family history.