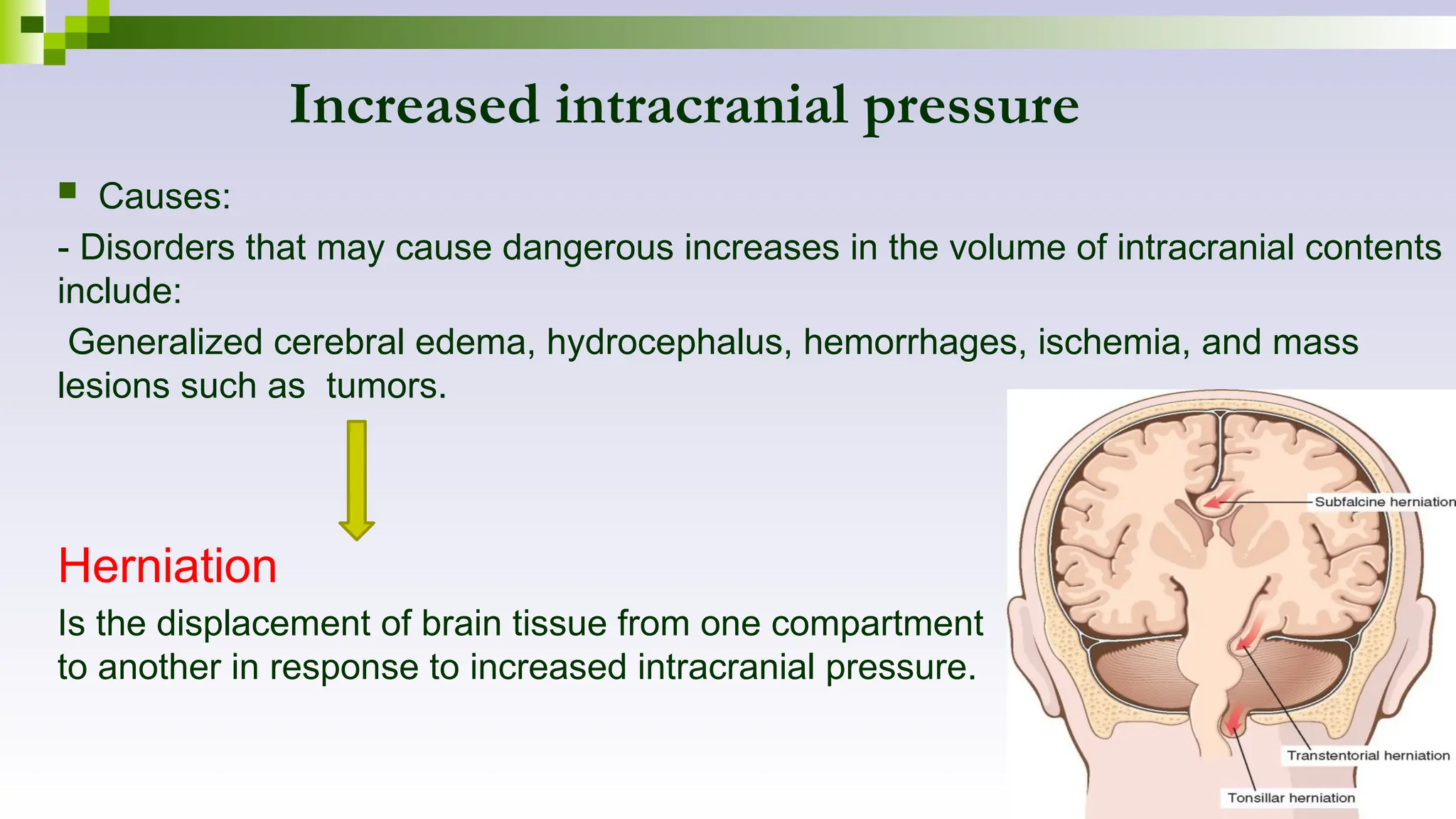
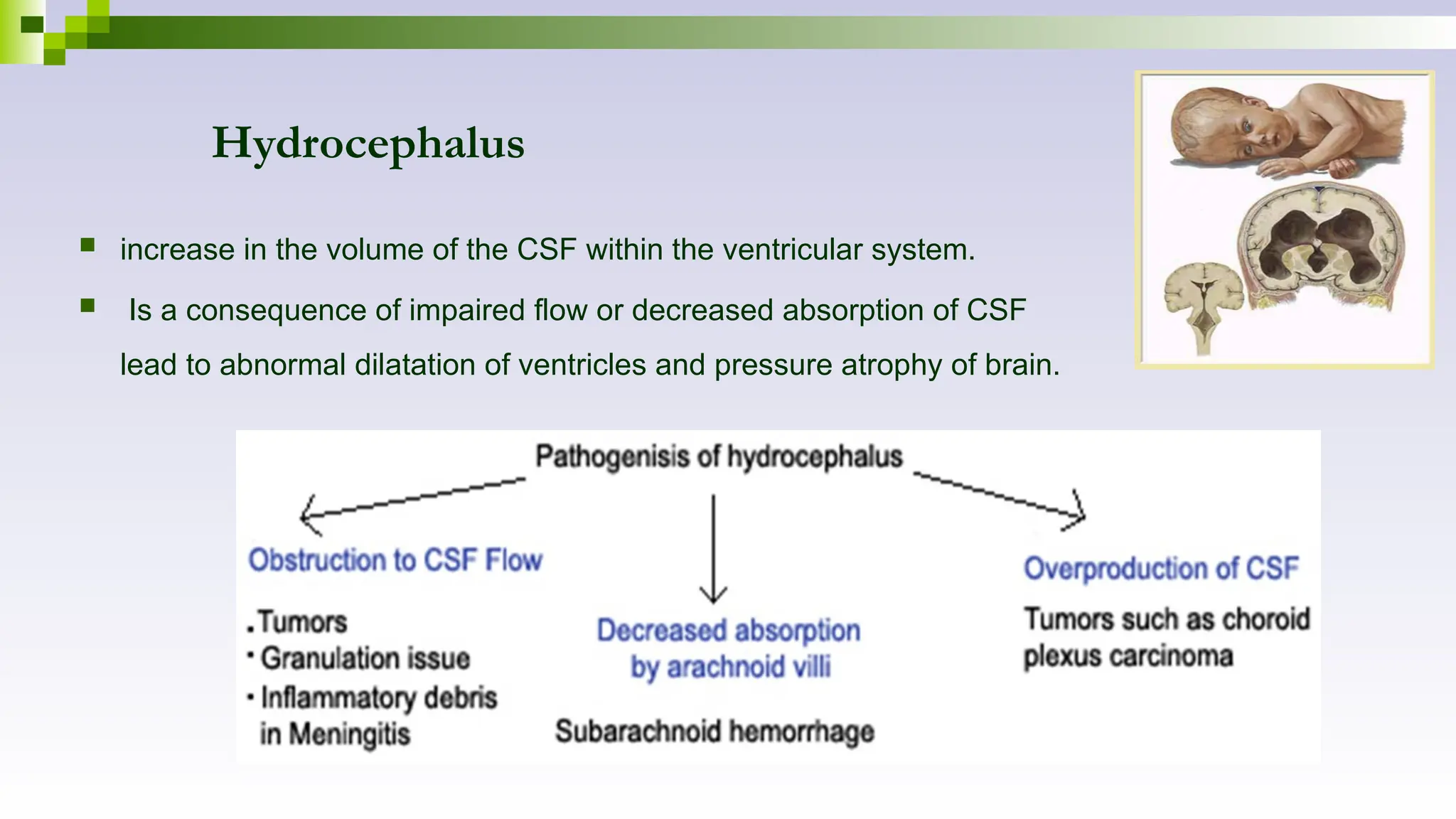
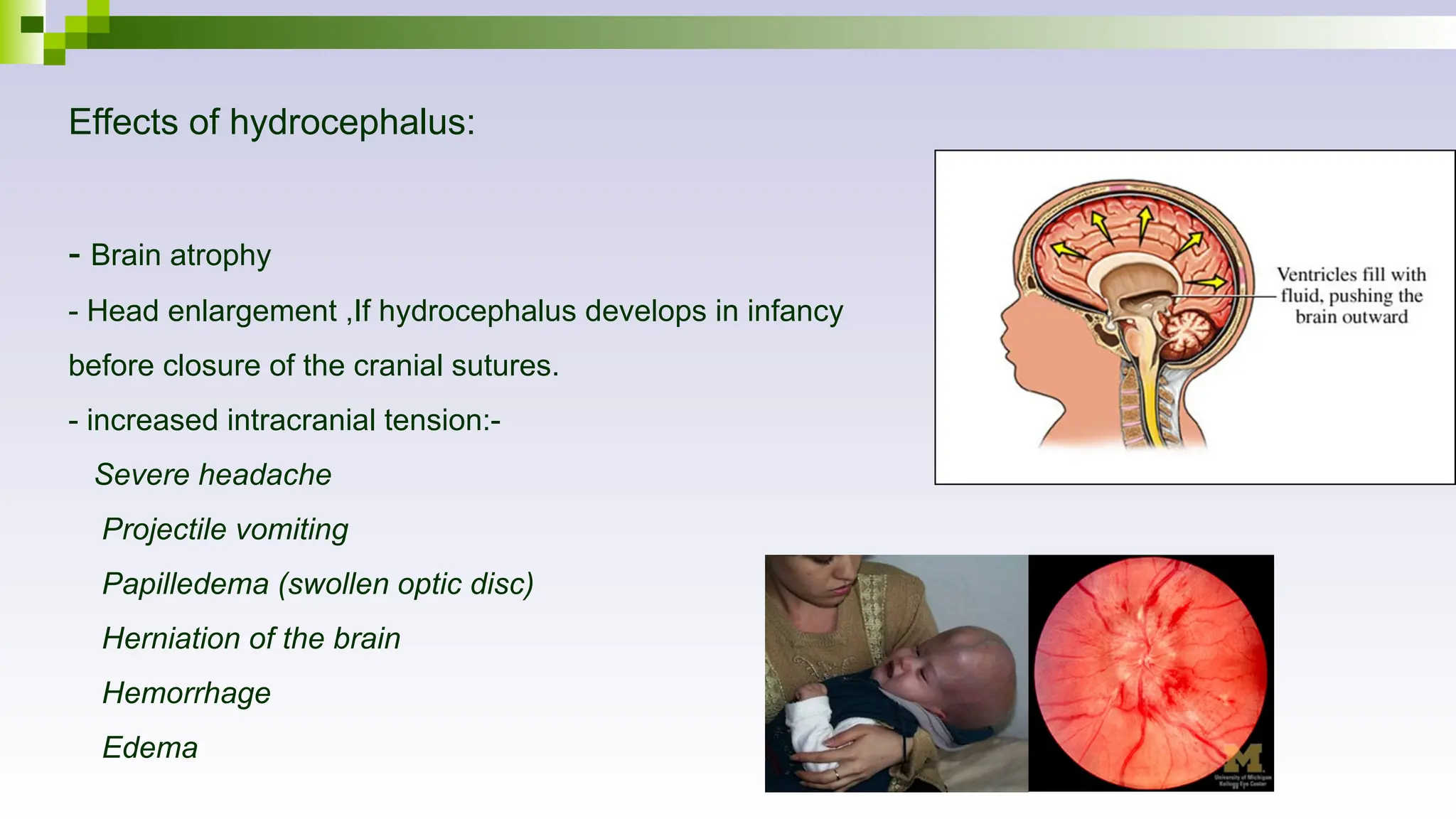
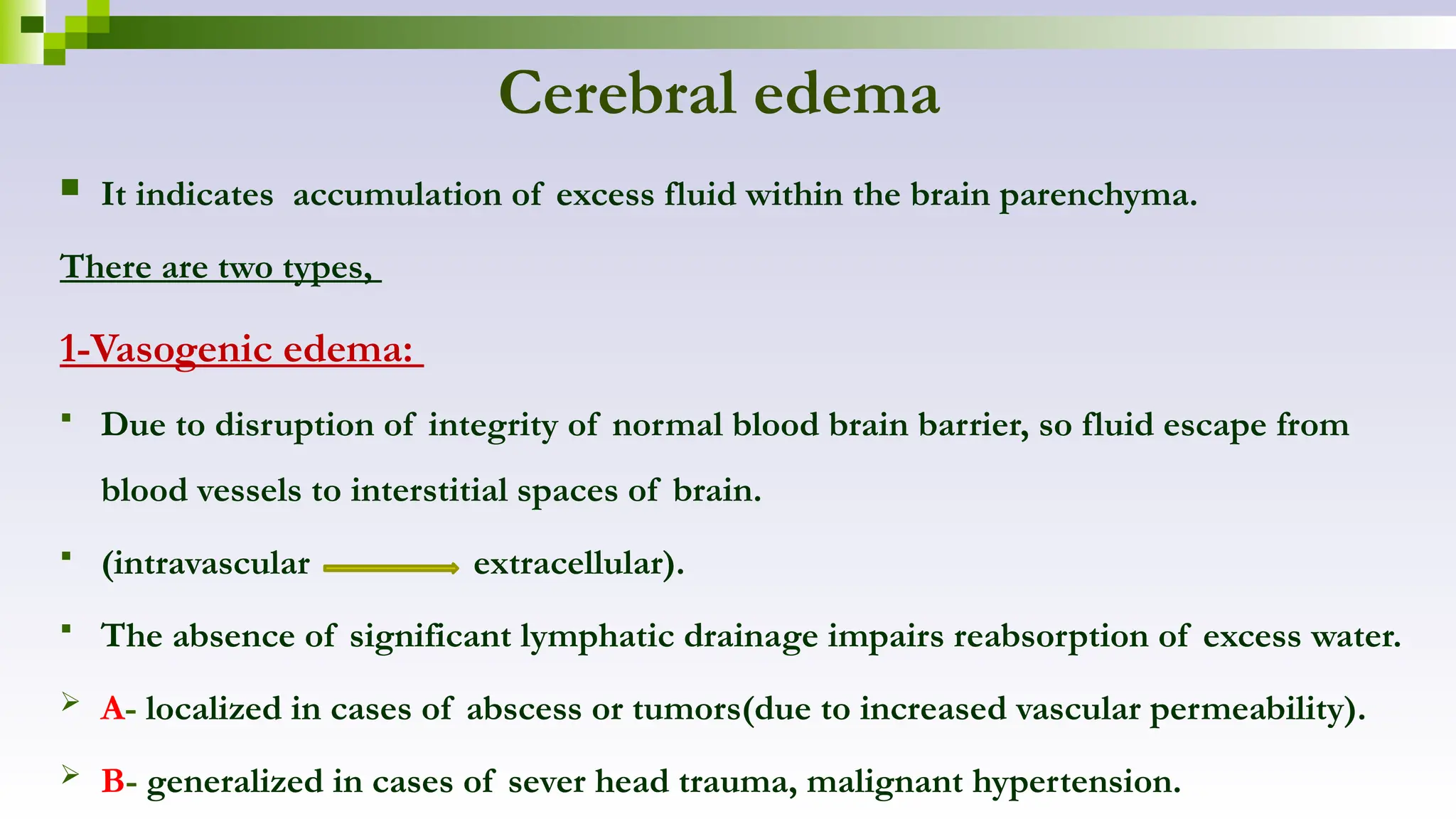
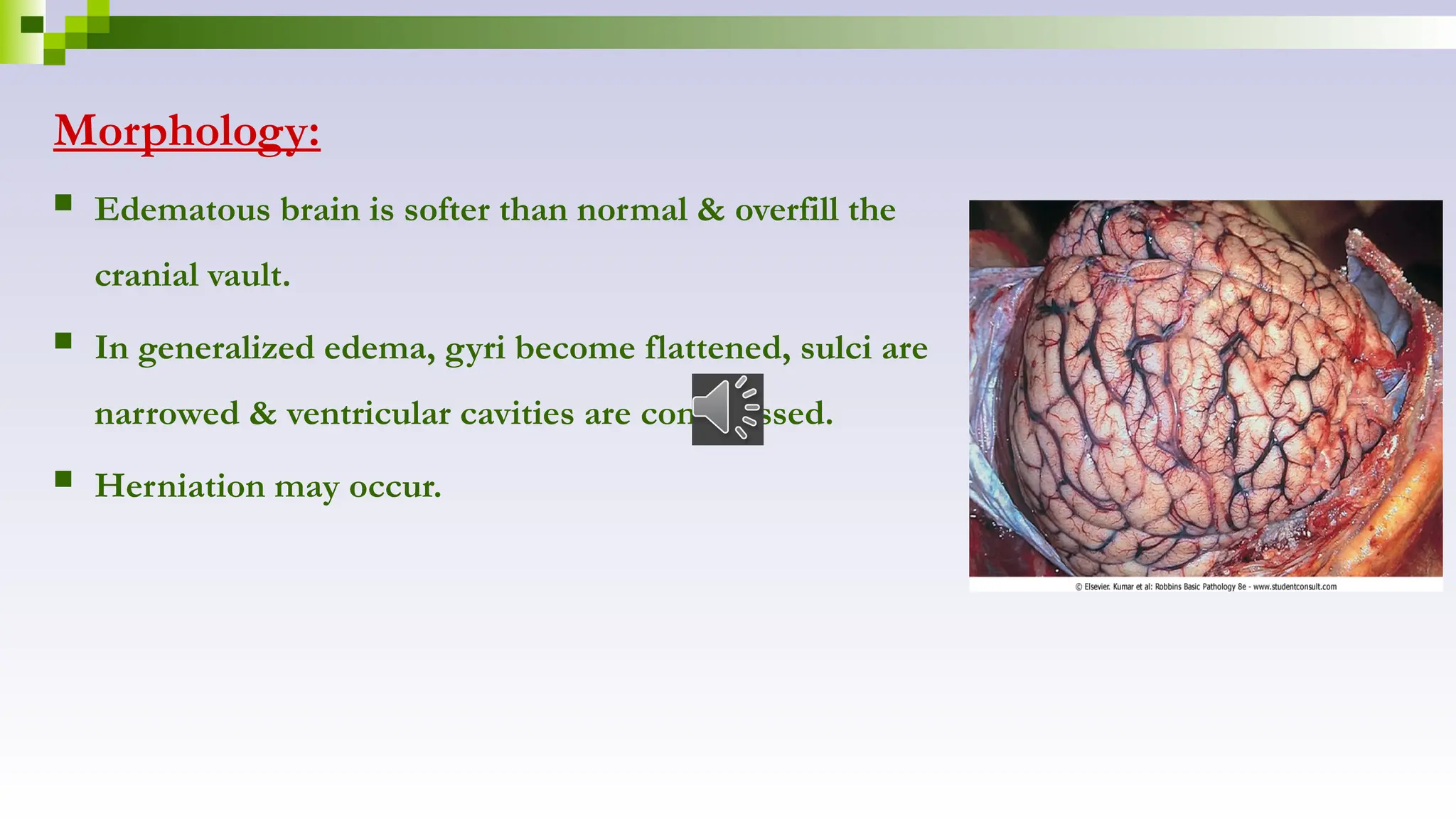
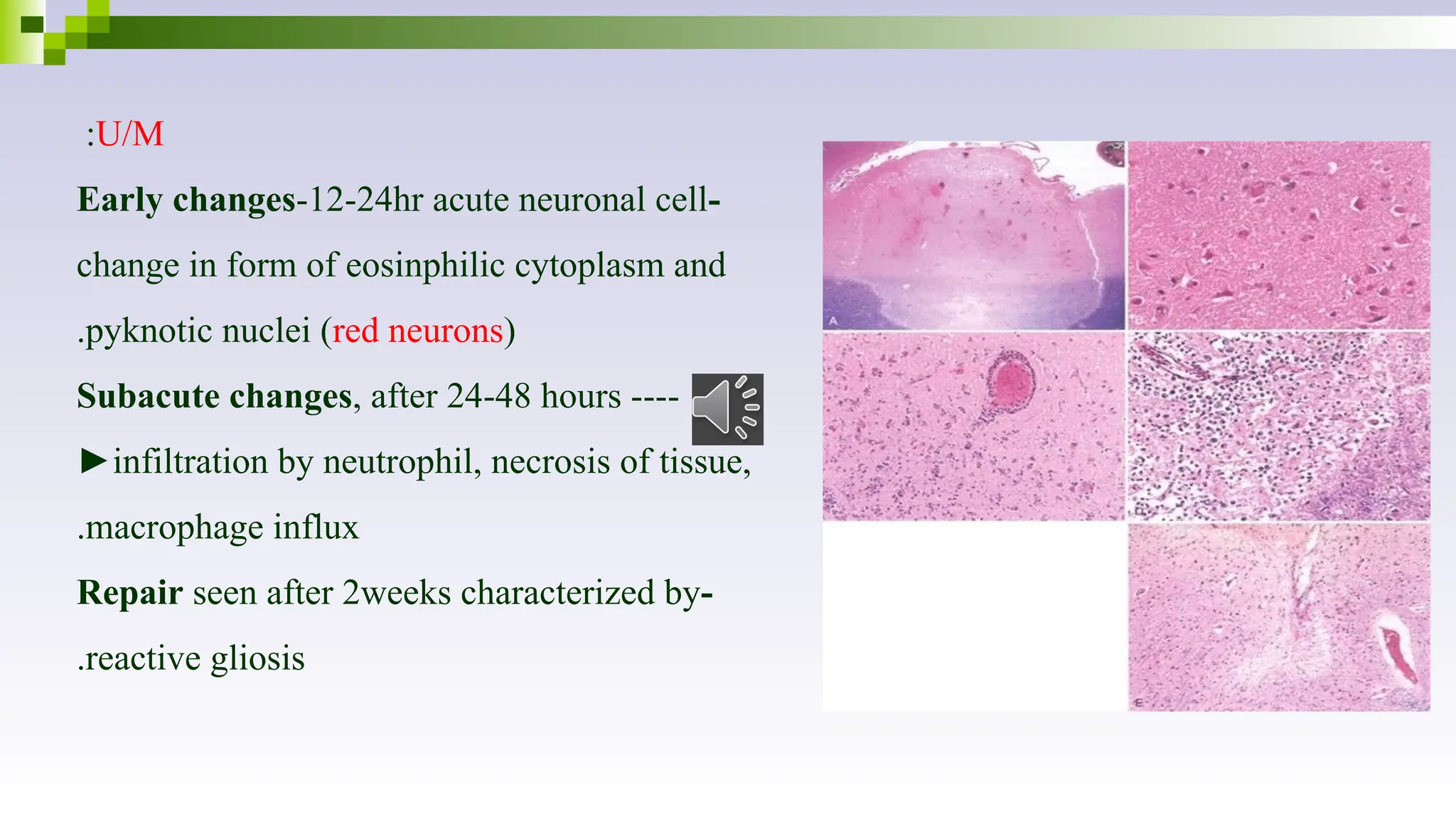
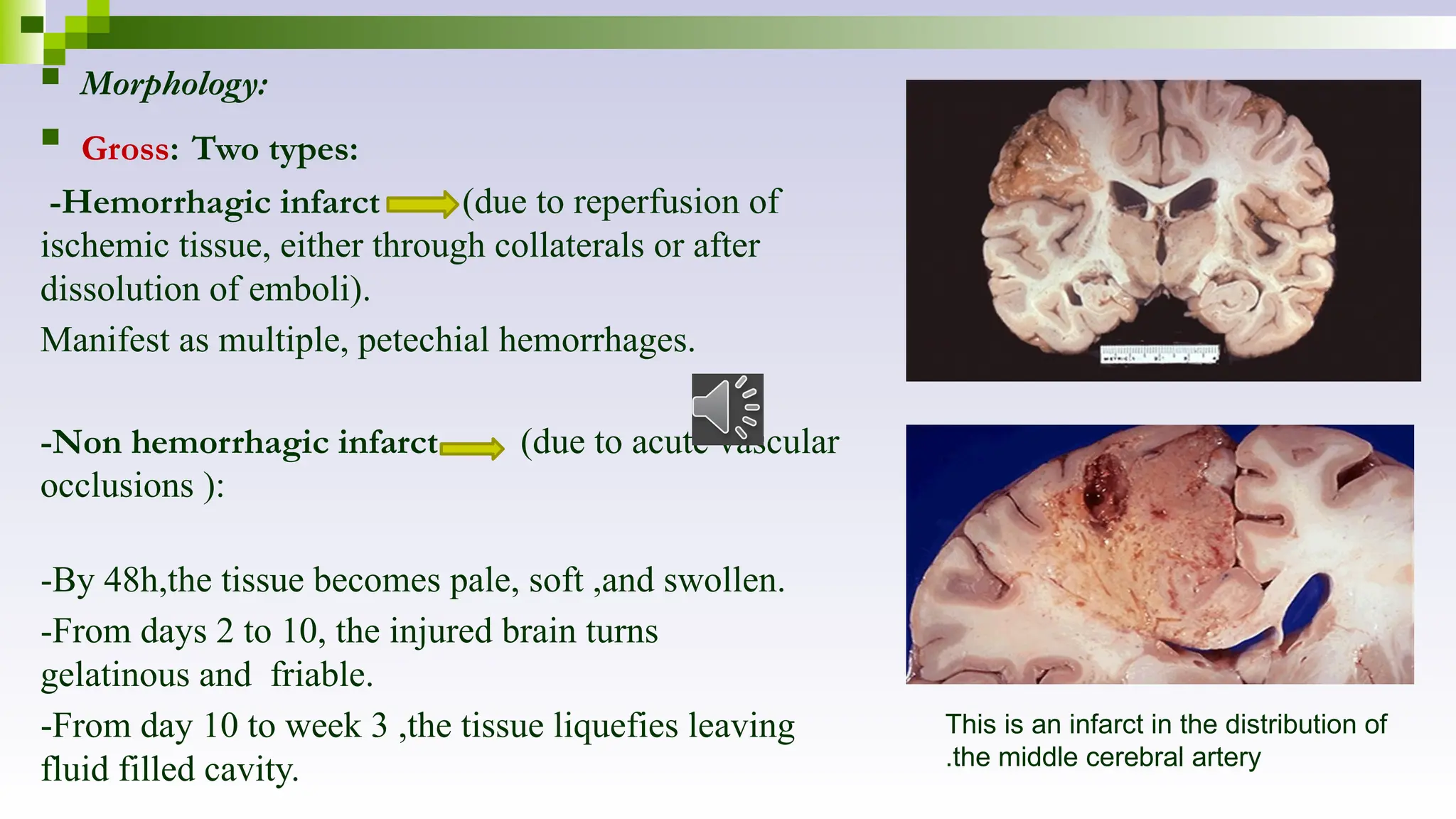
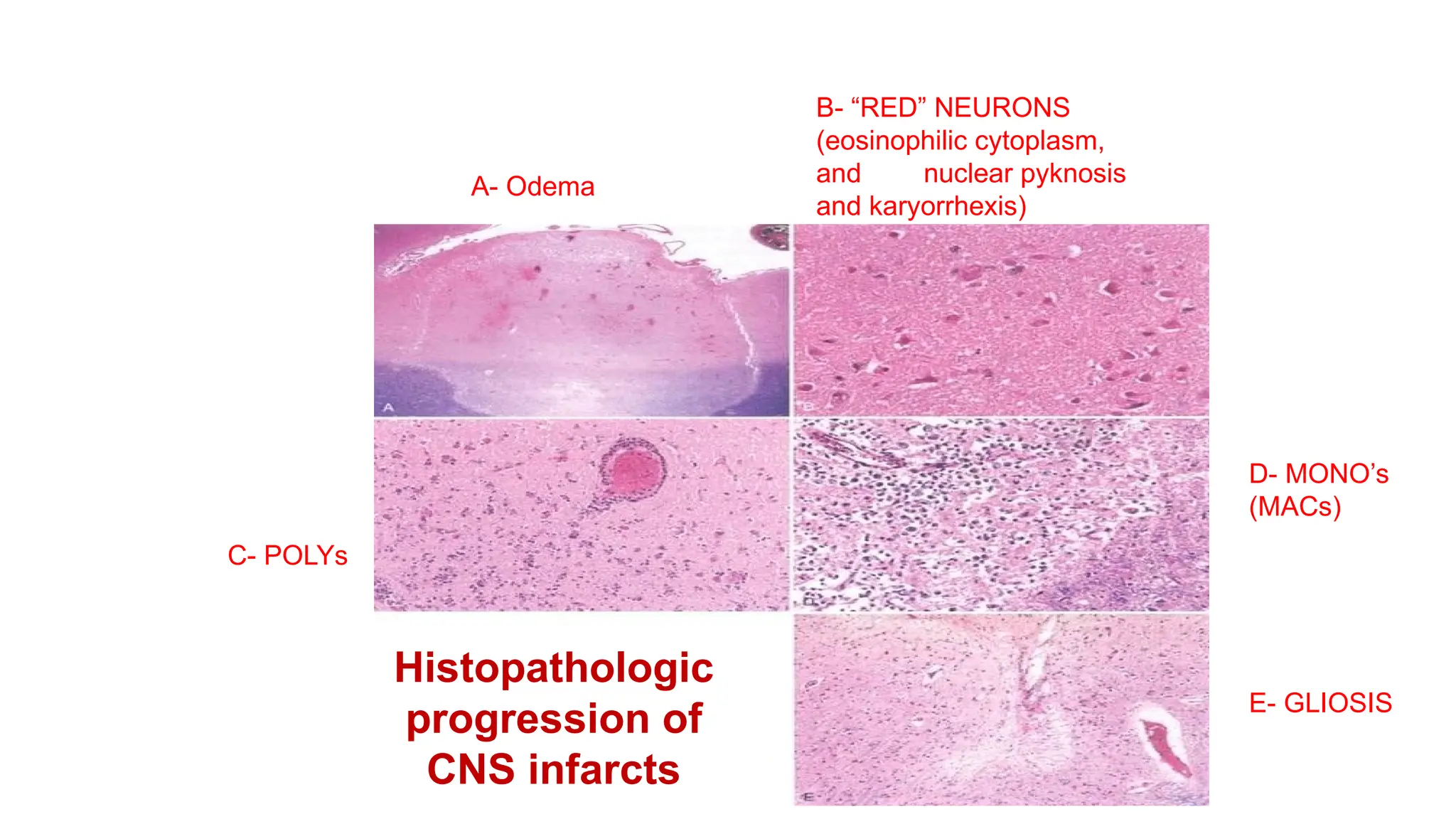
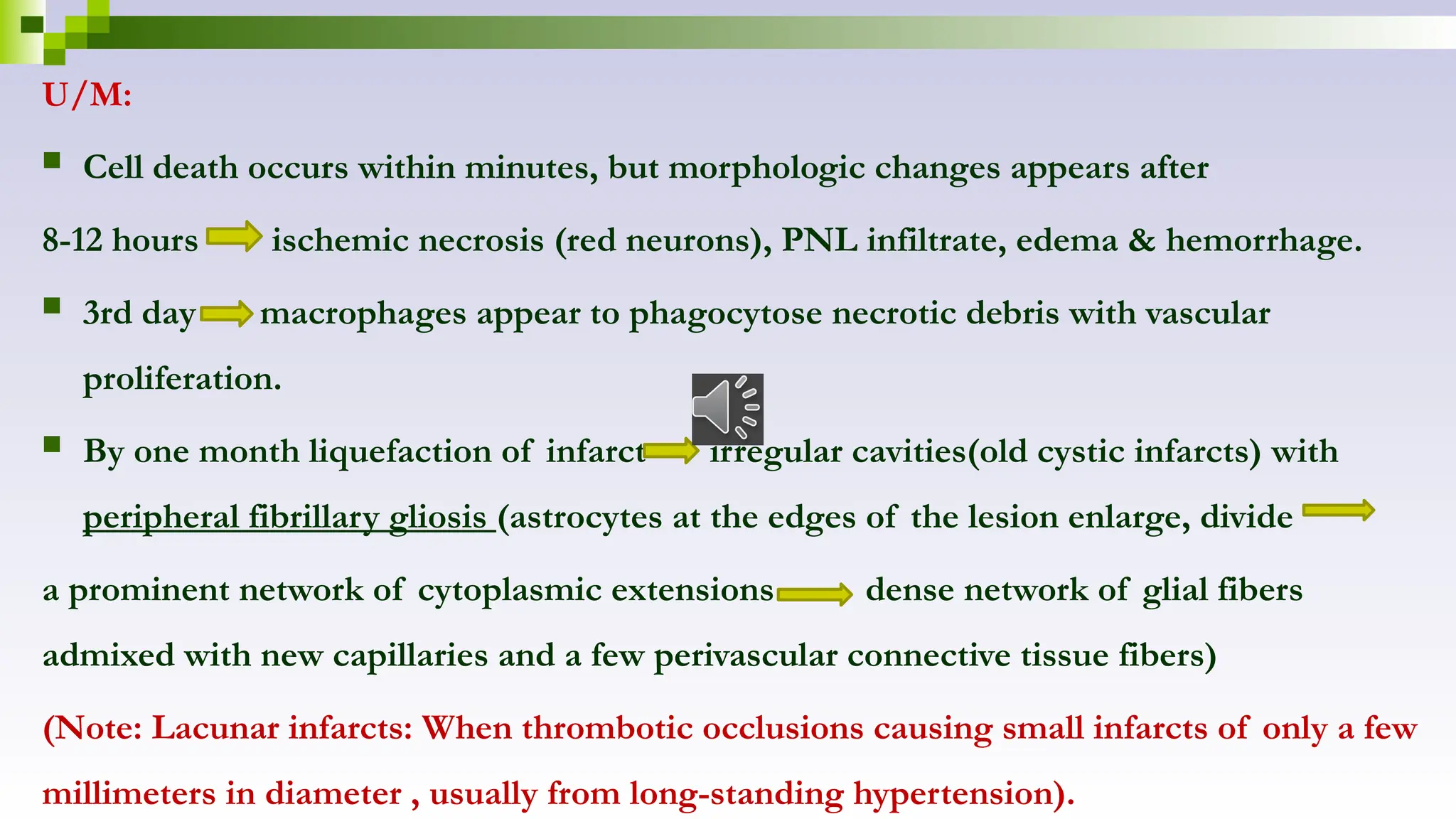
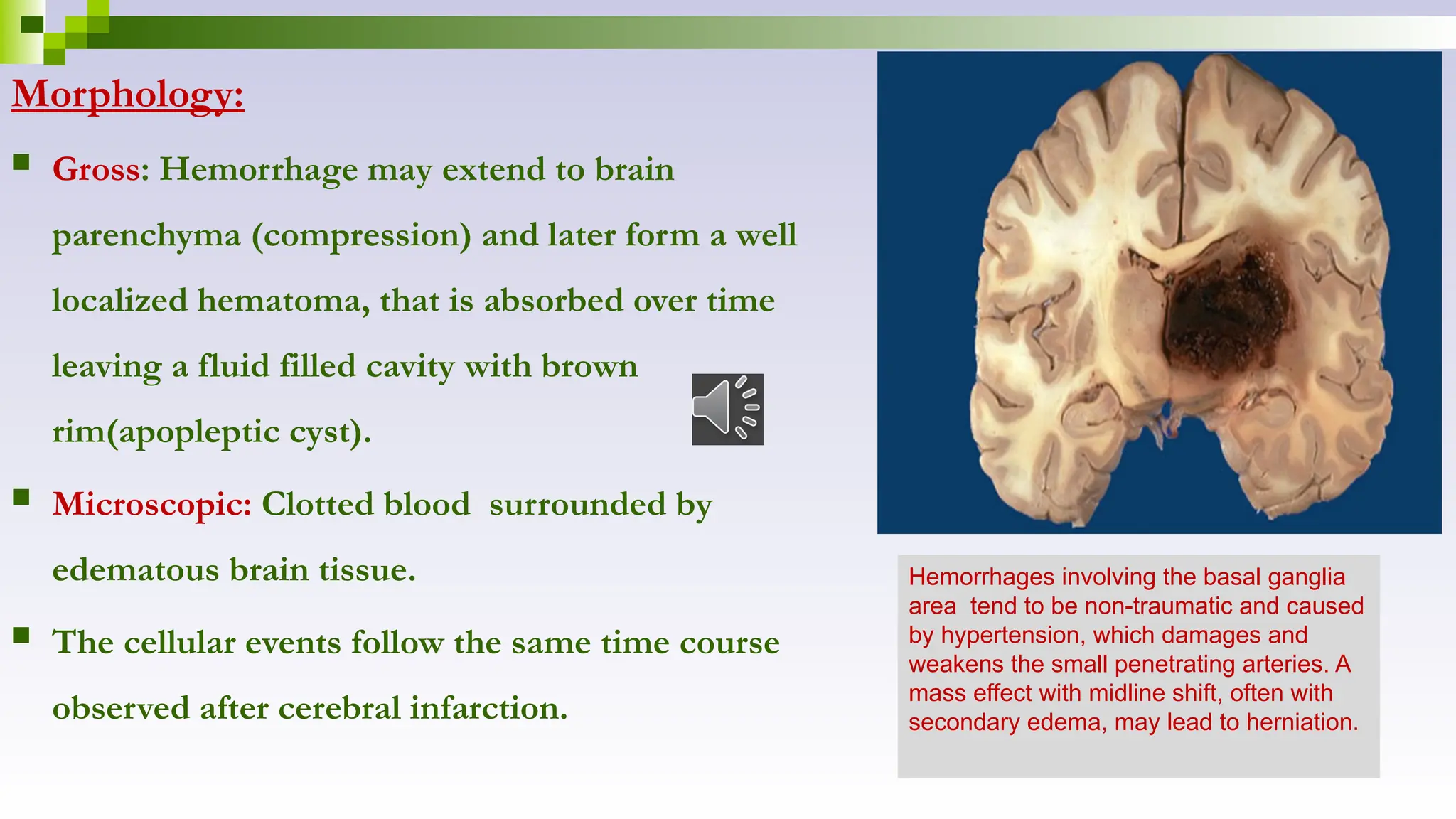
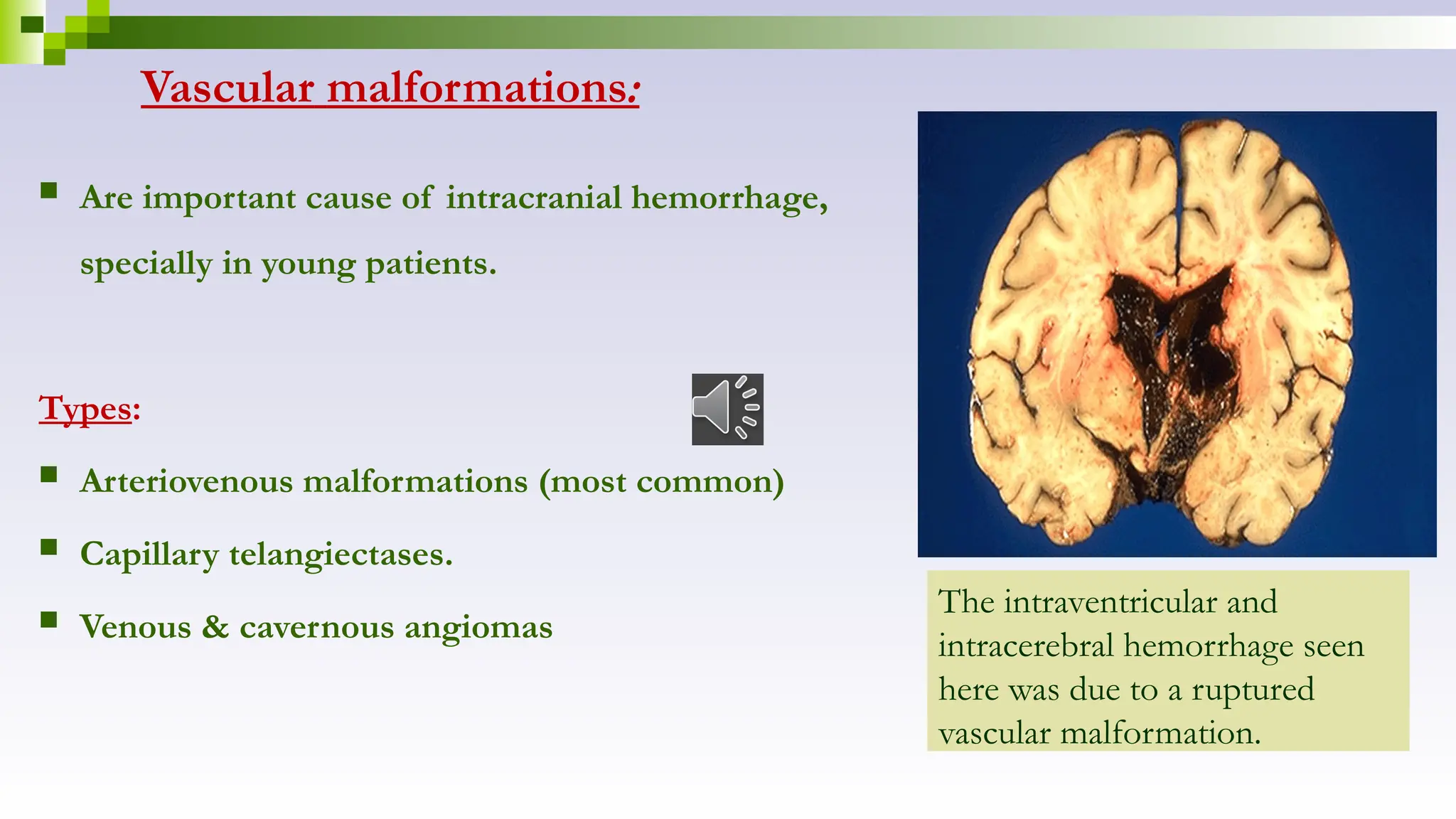
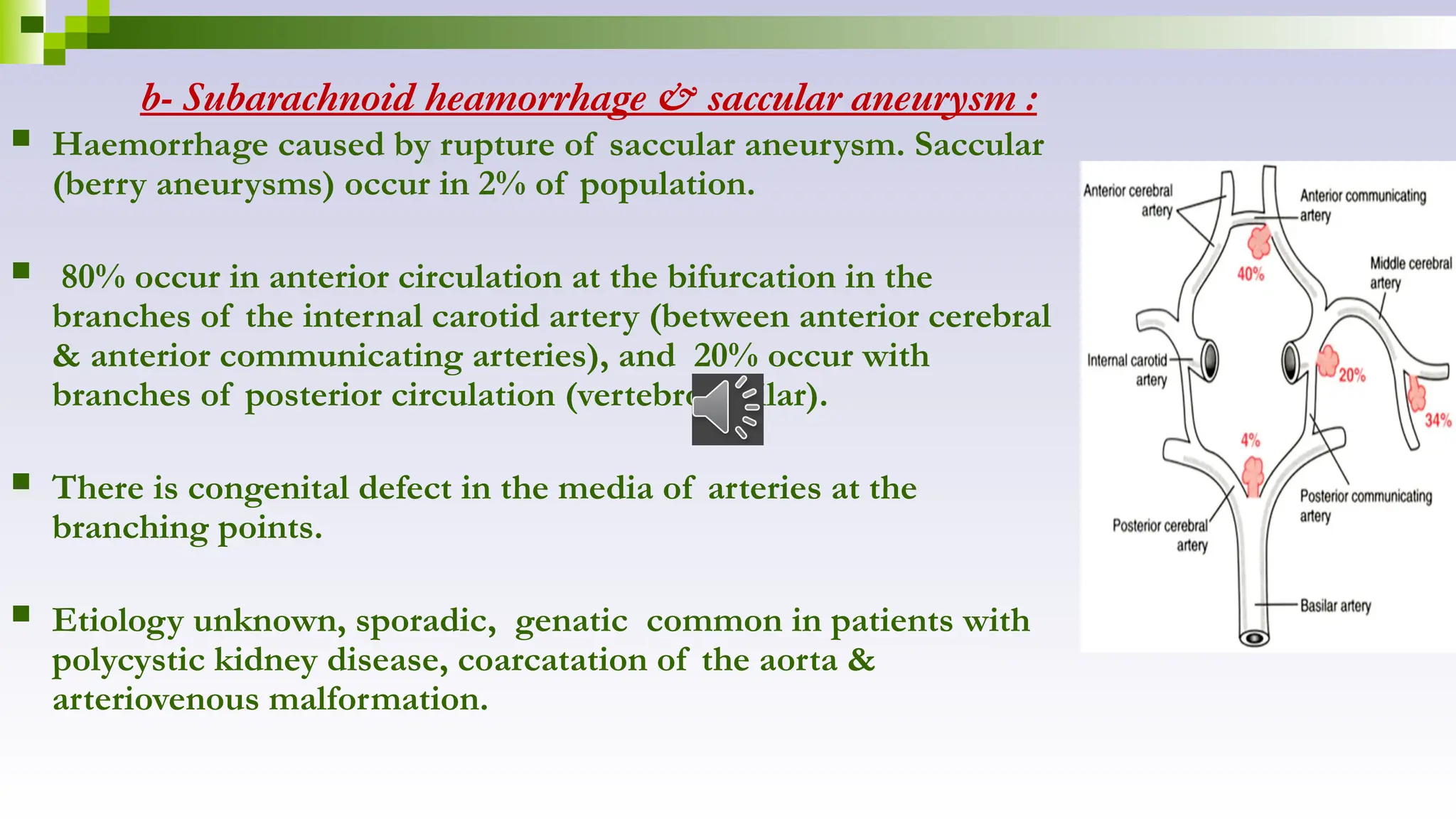
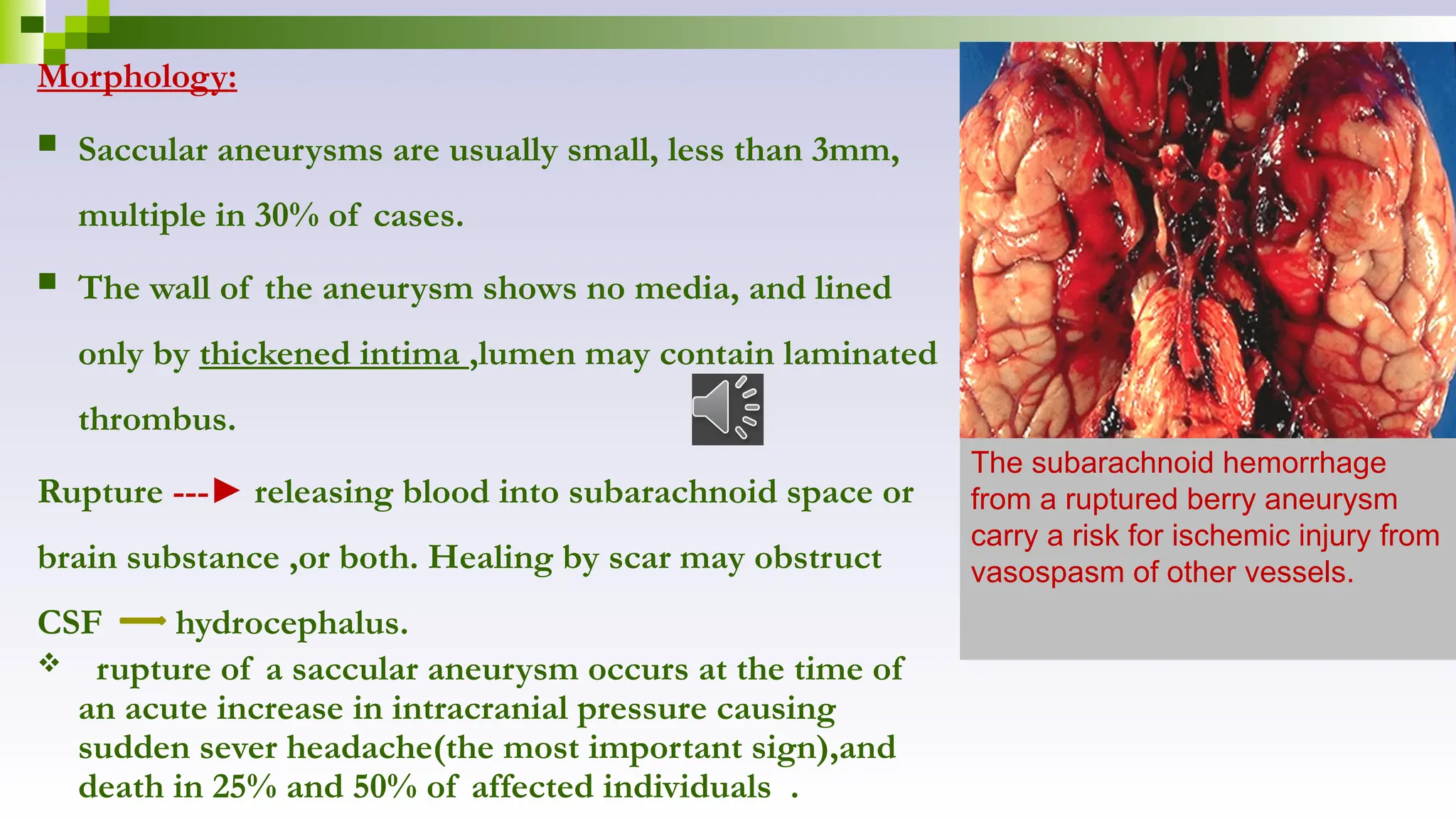
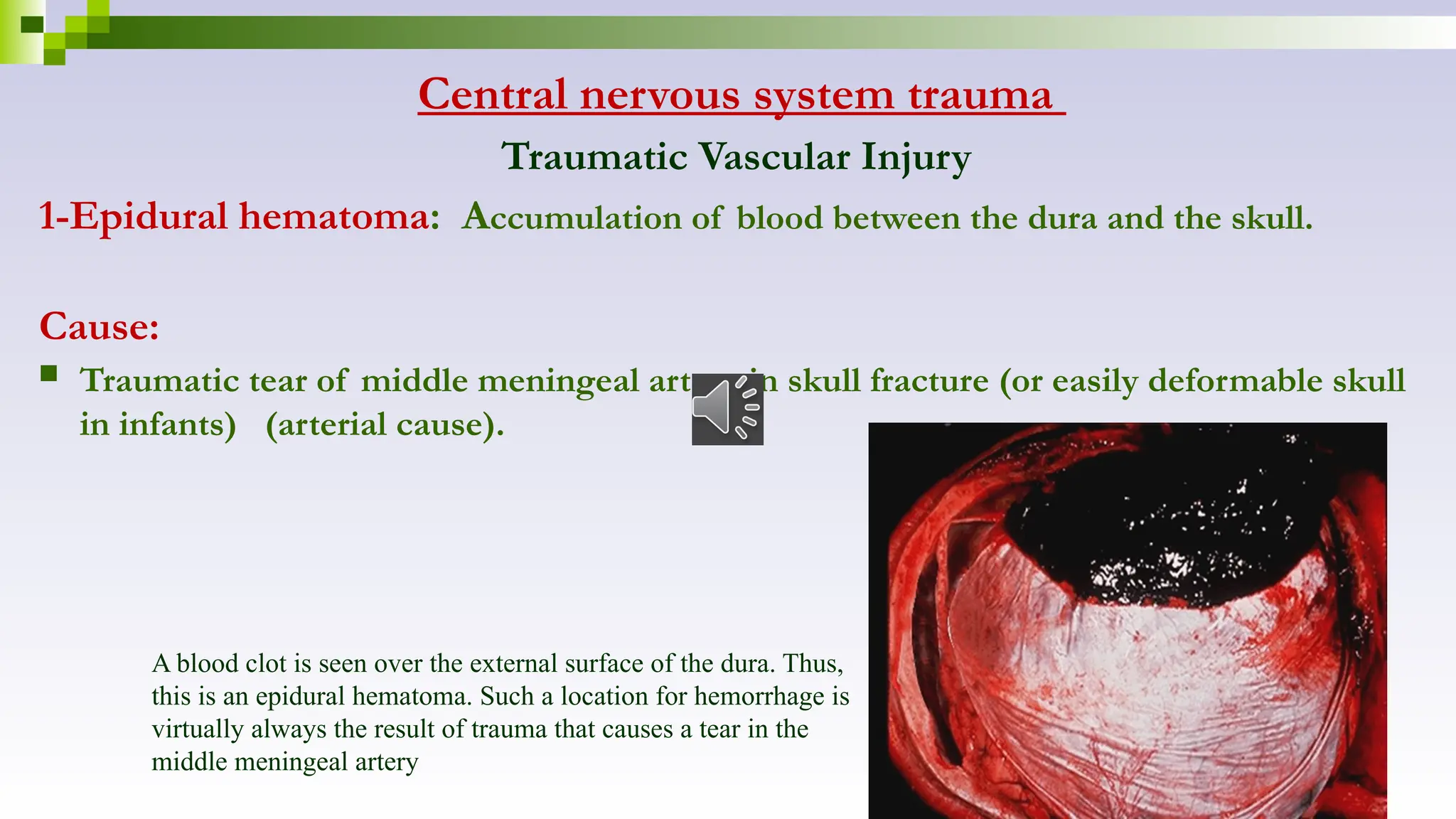
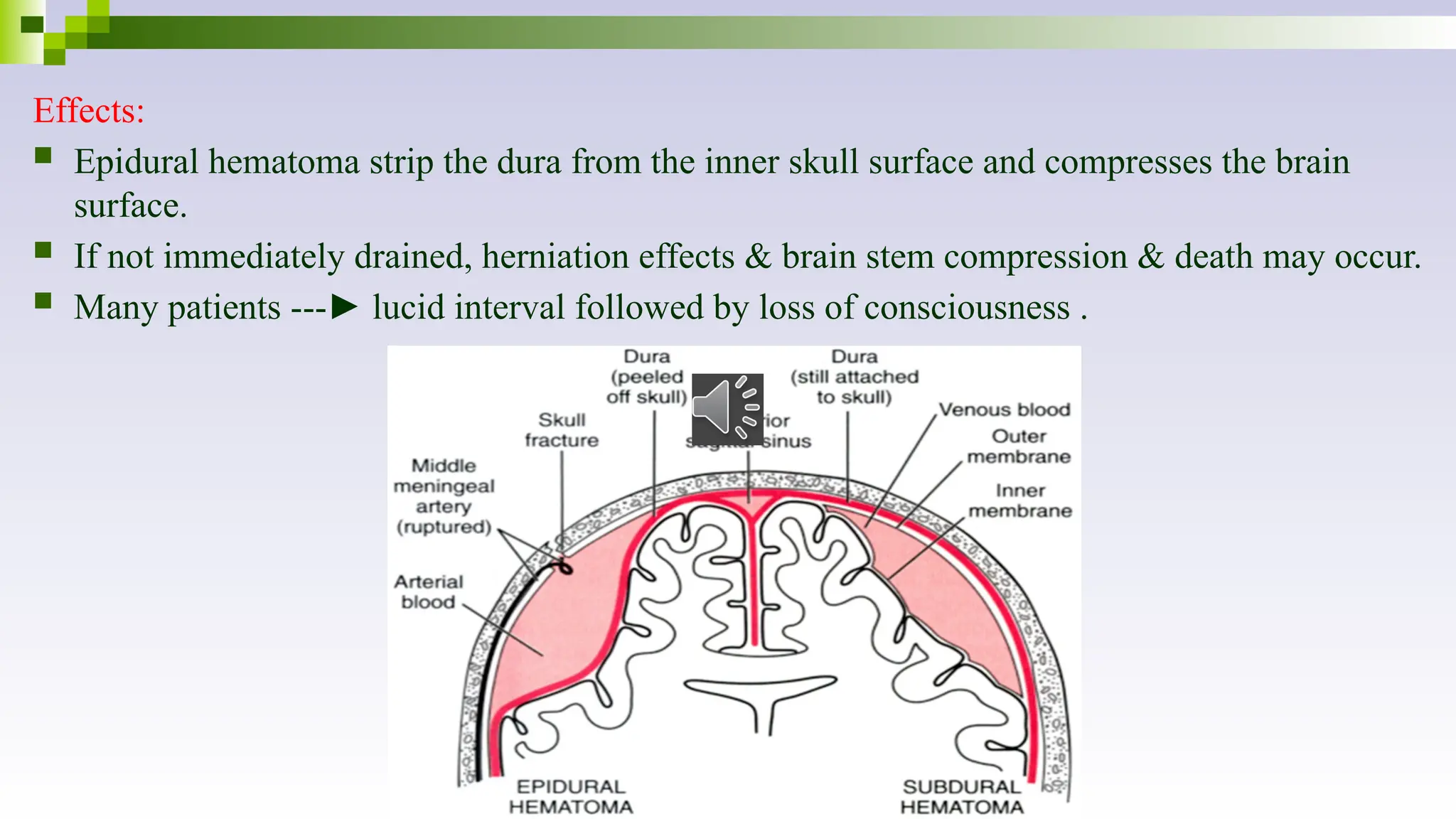
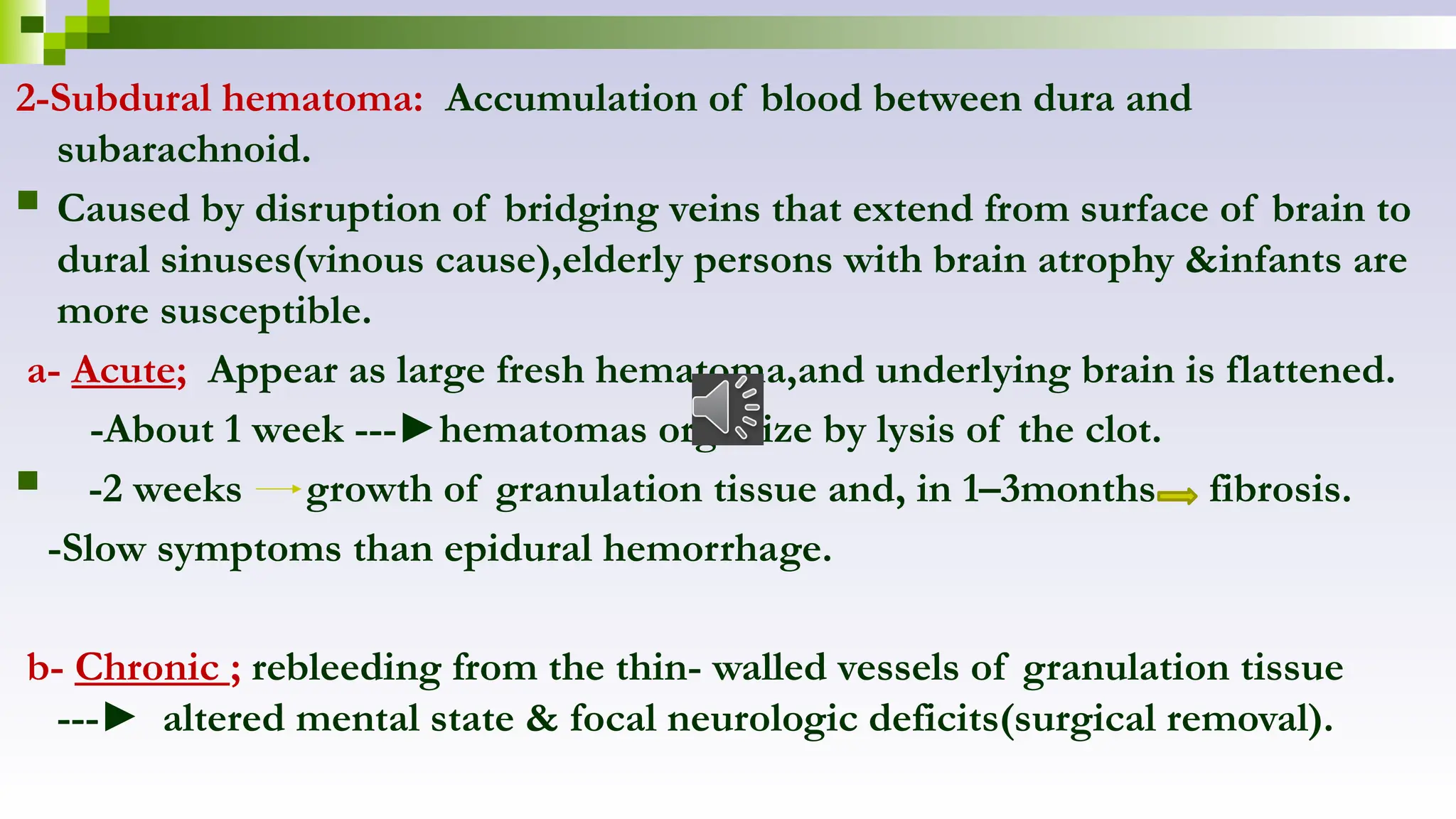
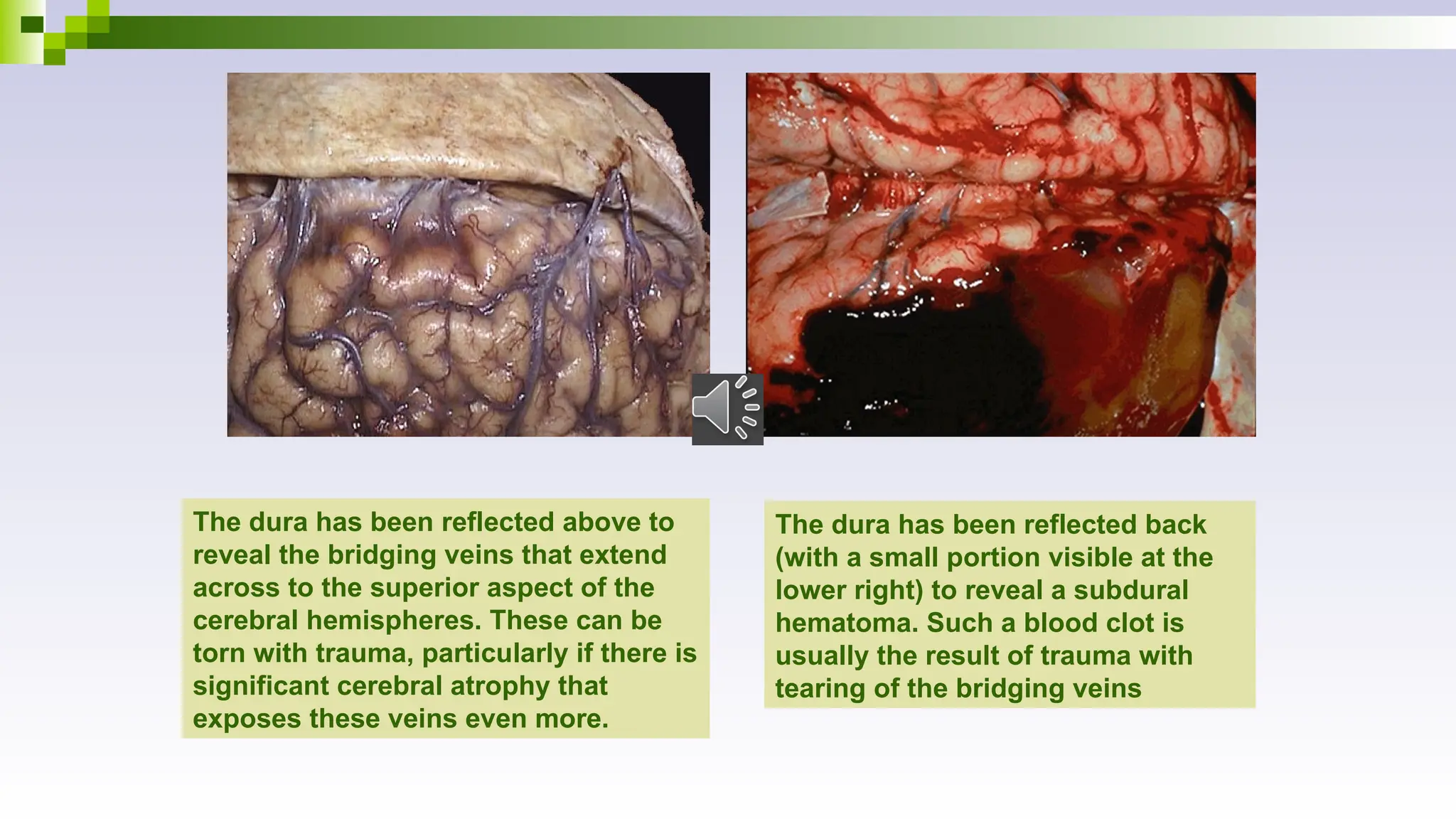
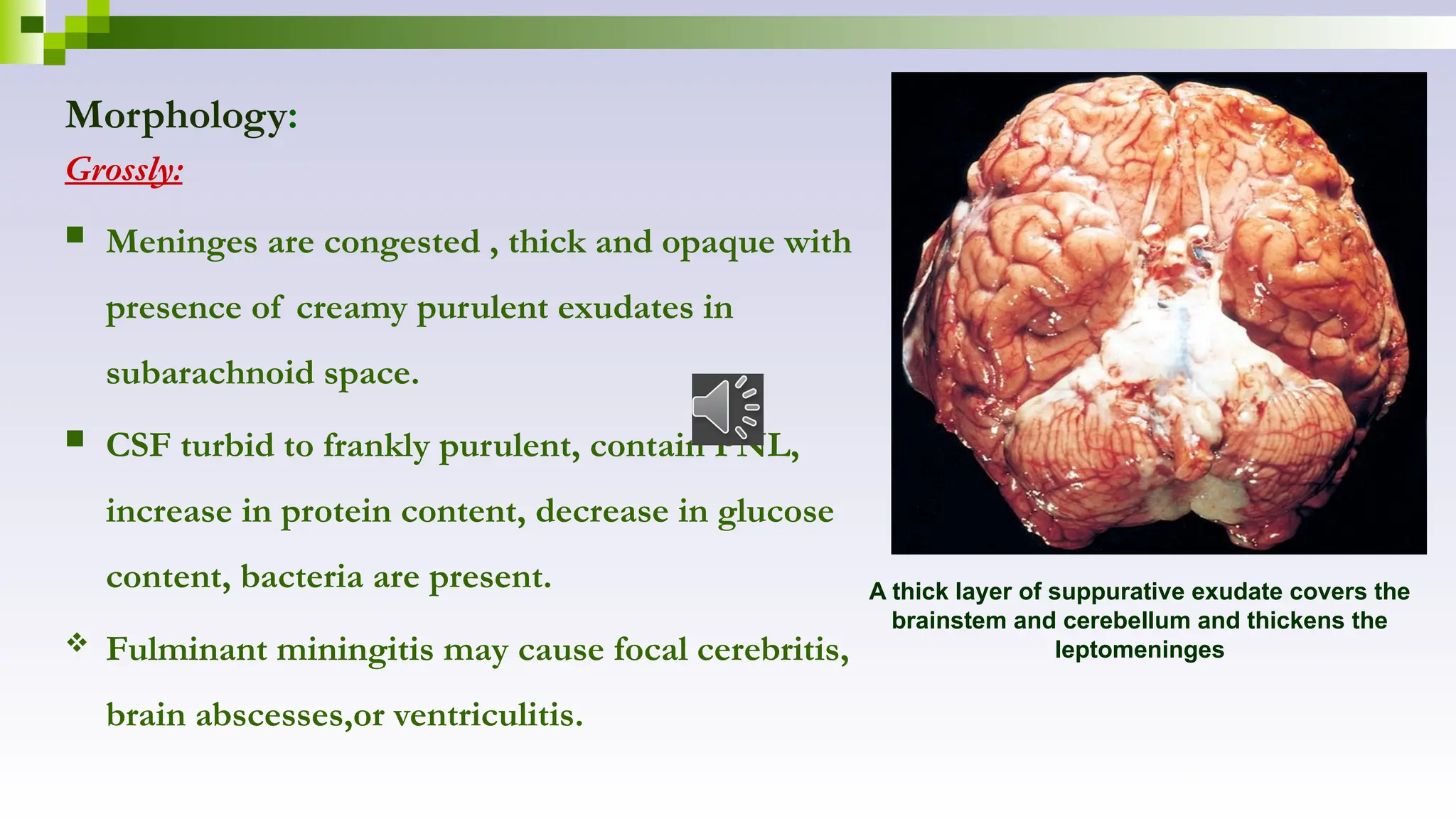
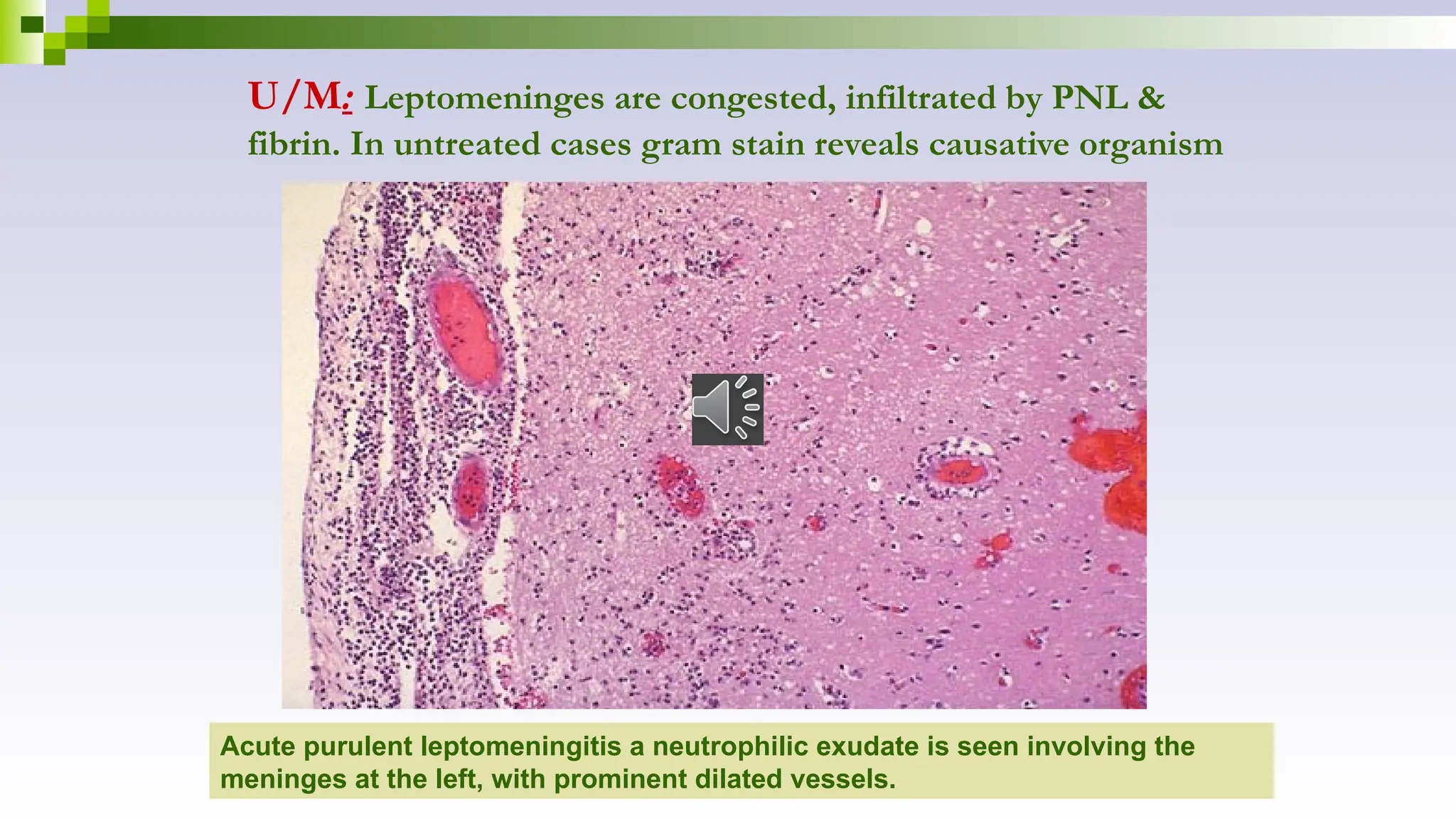
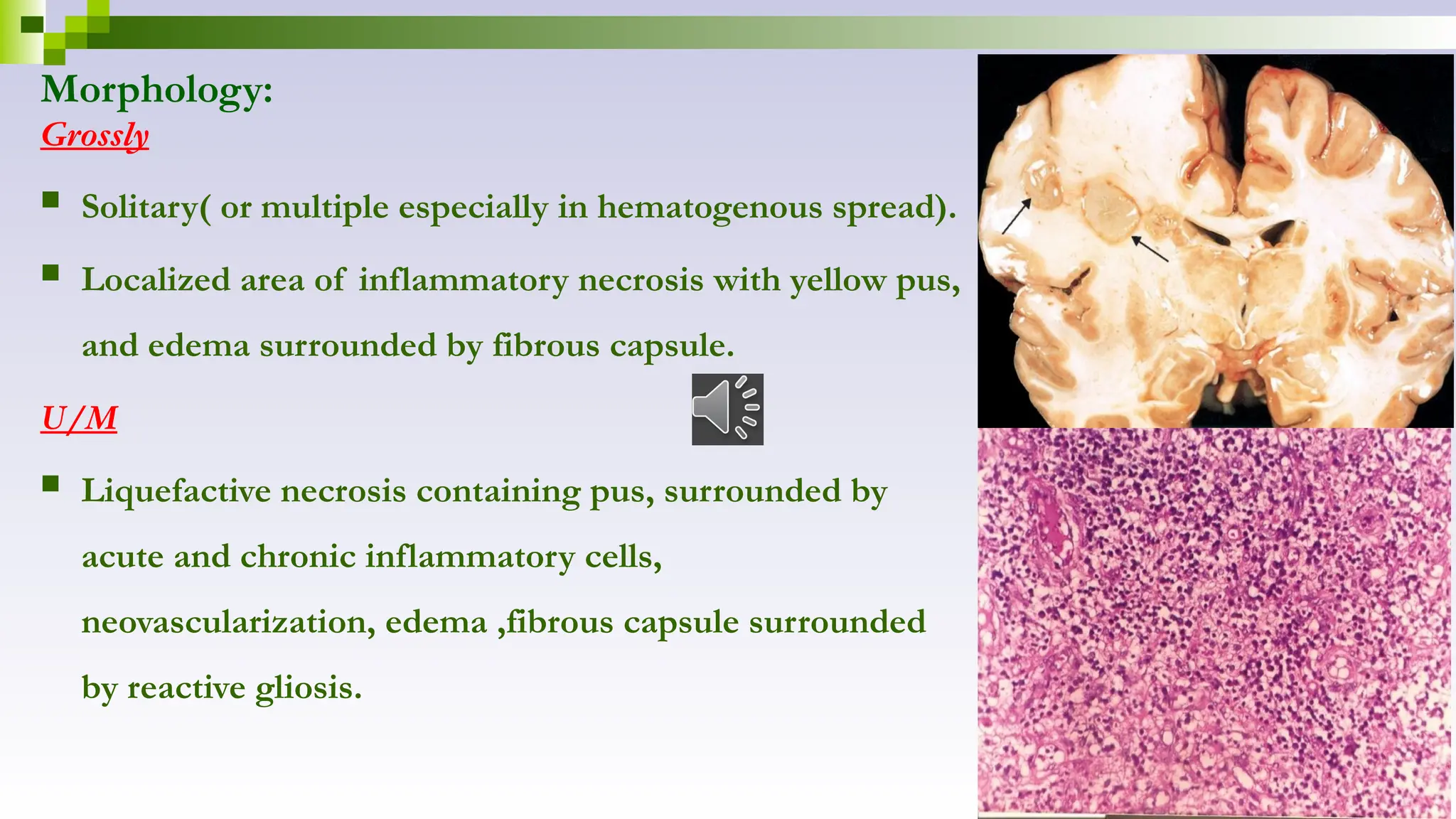
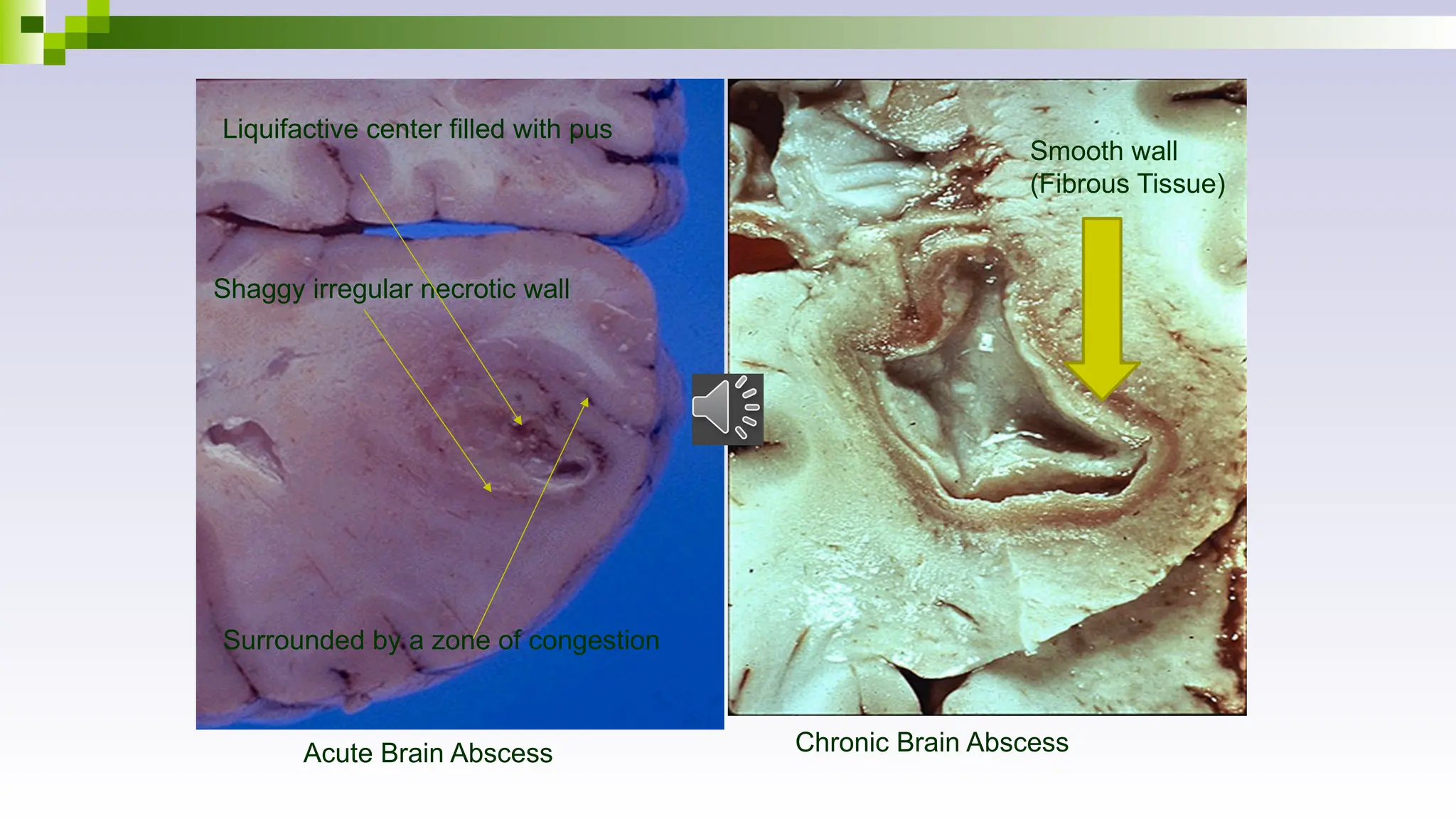
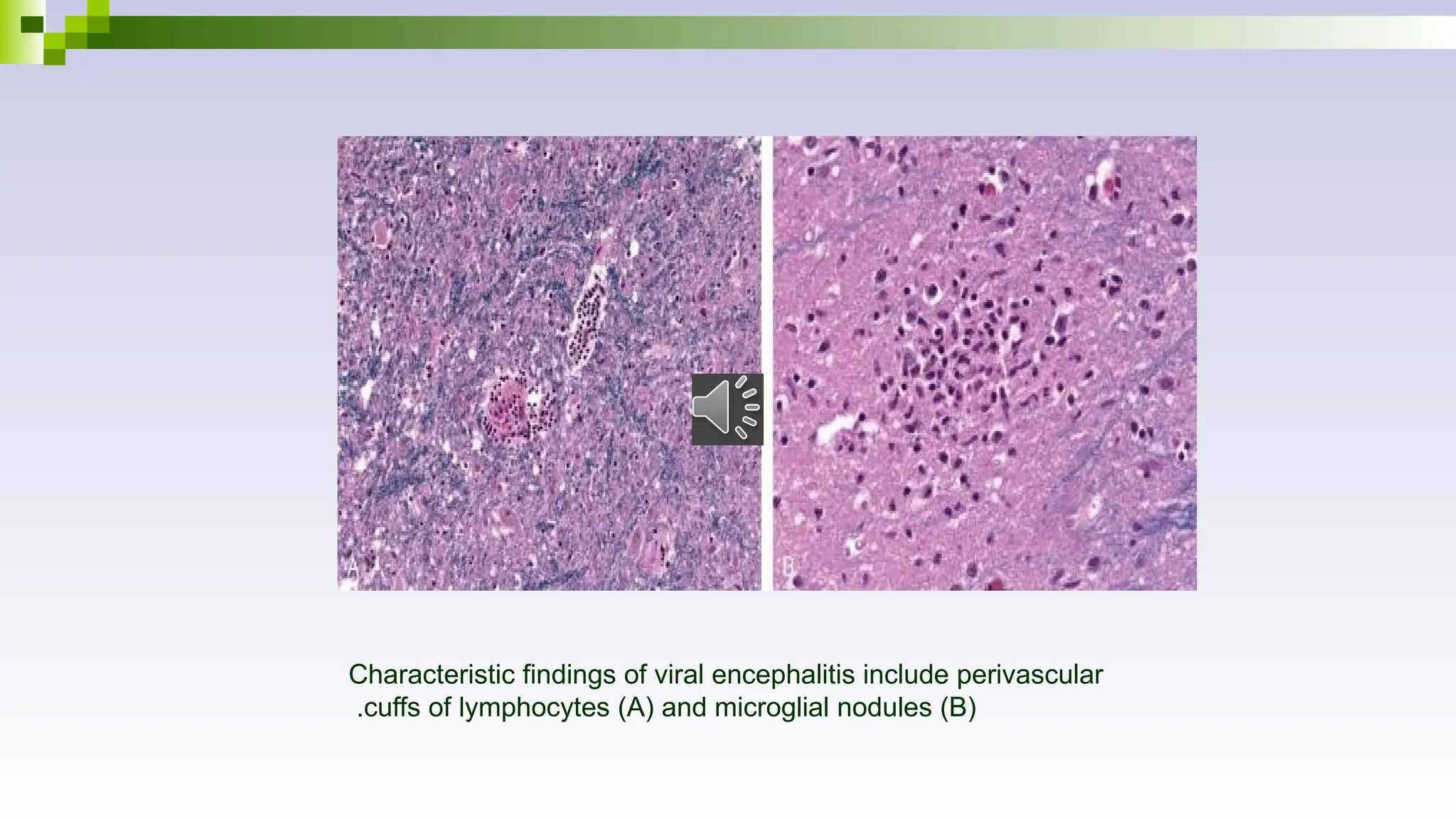
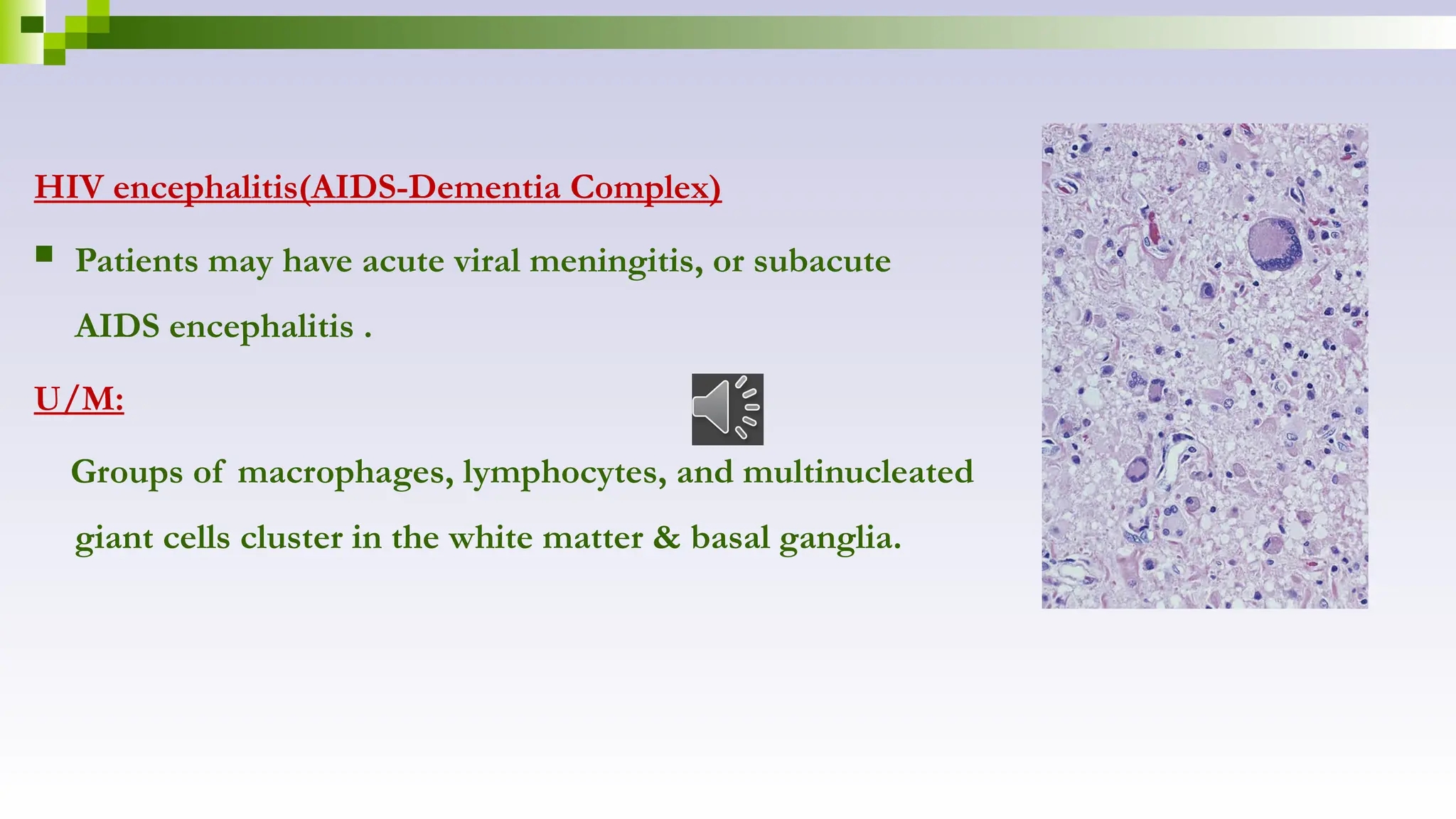
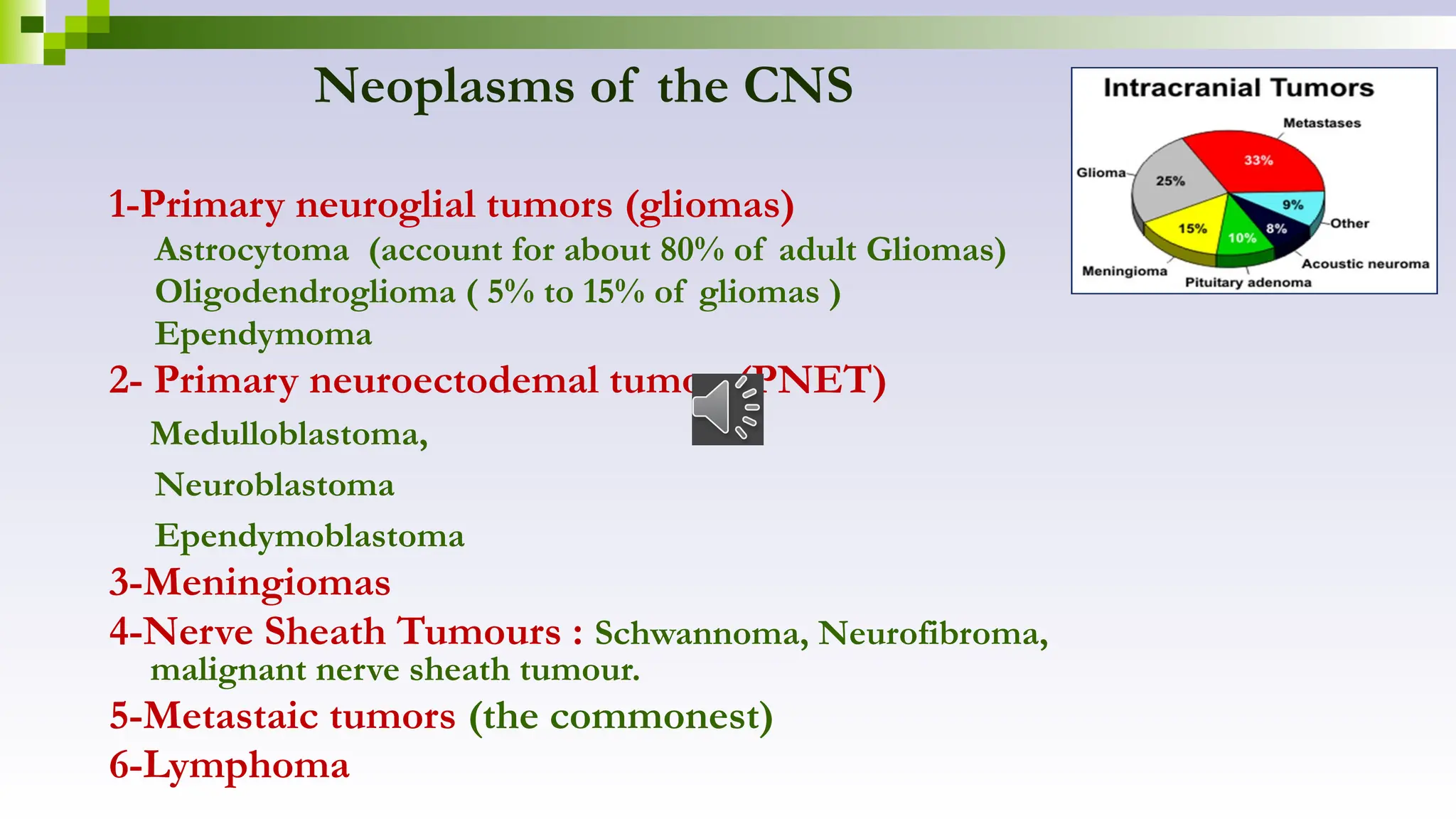
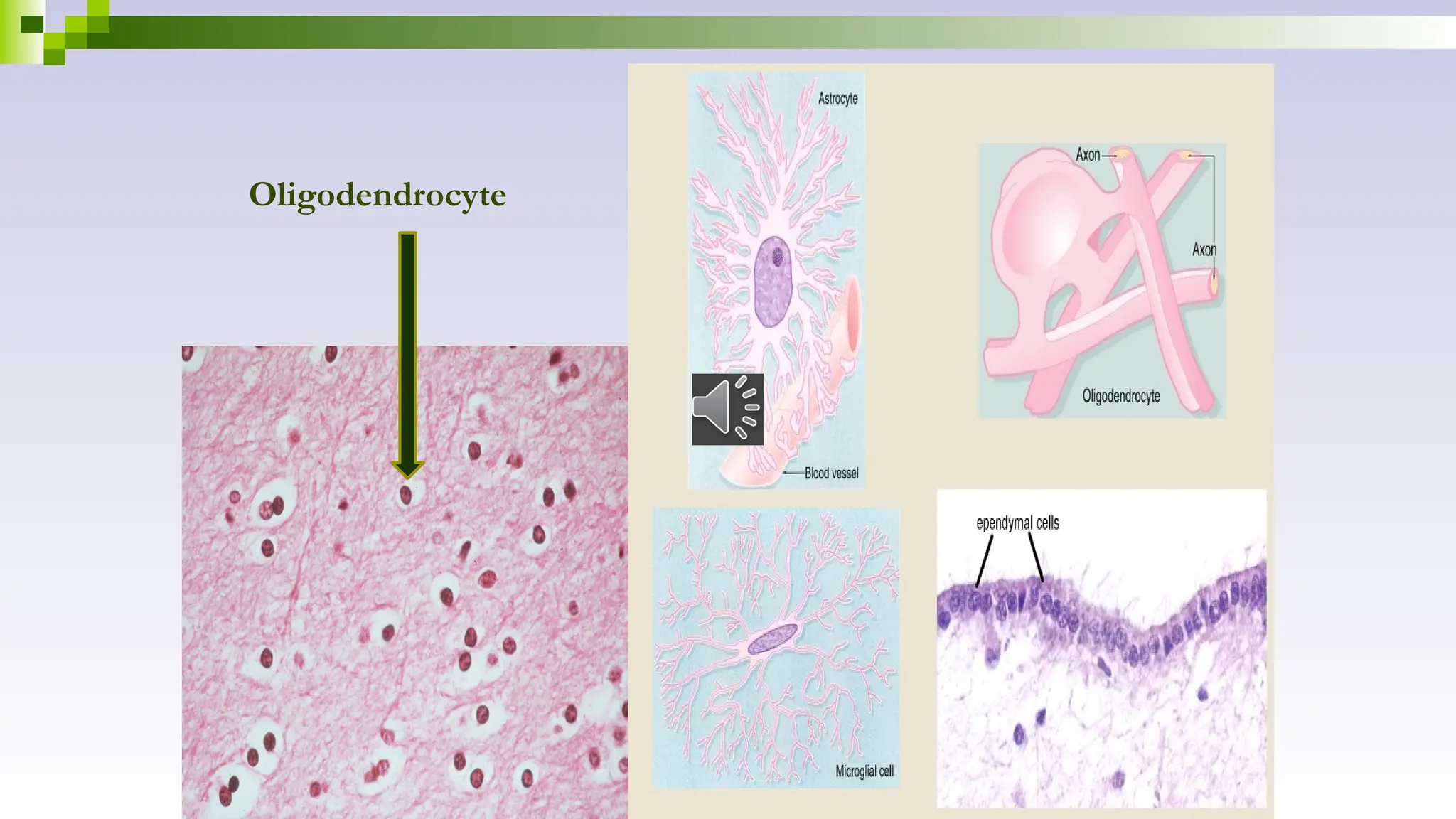
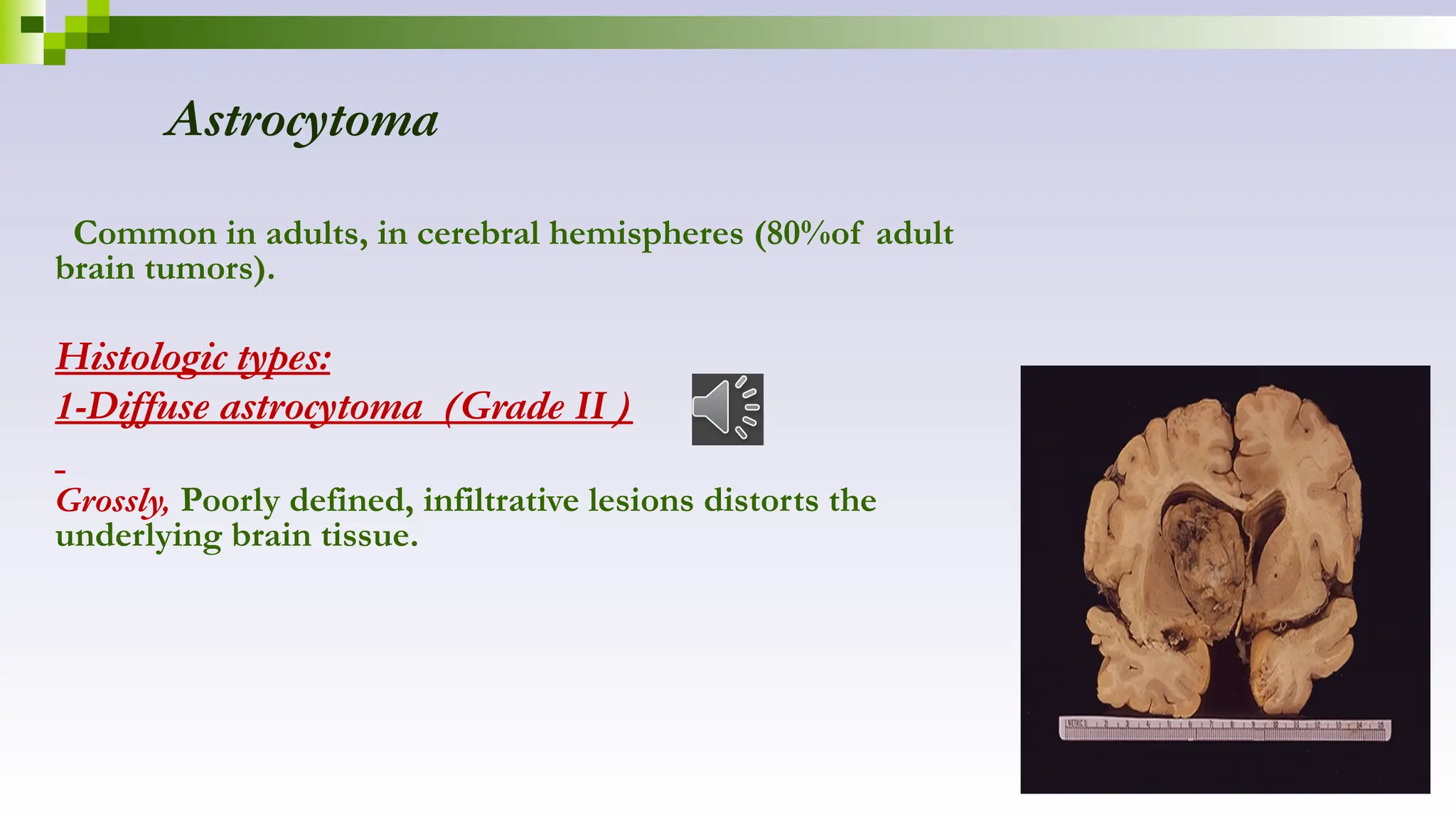
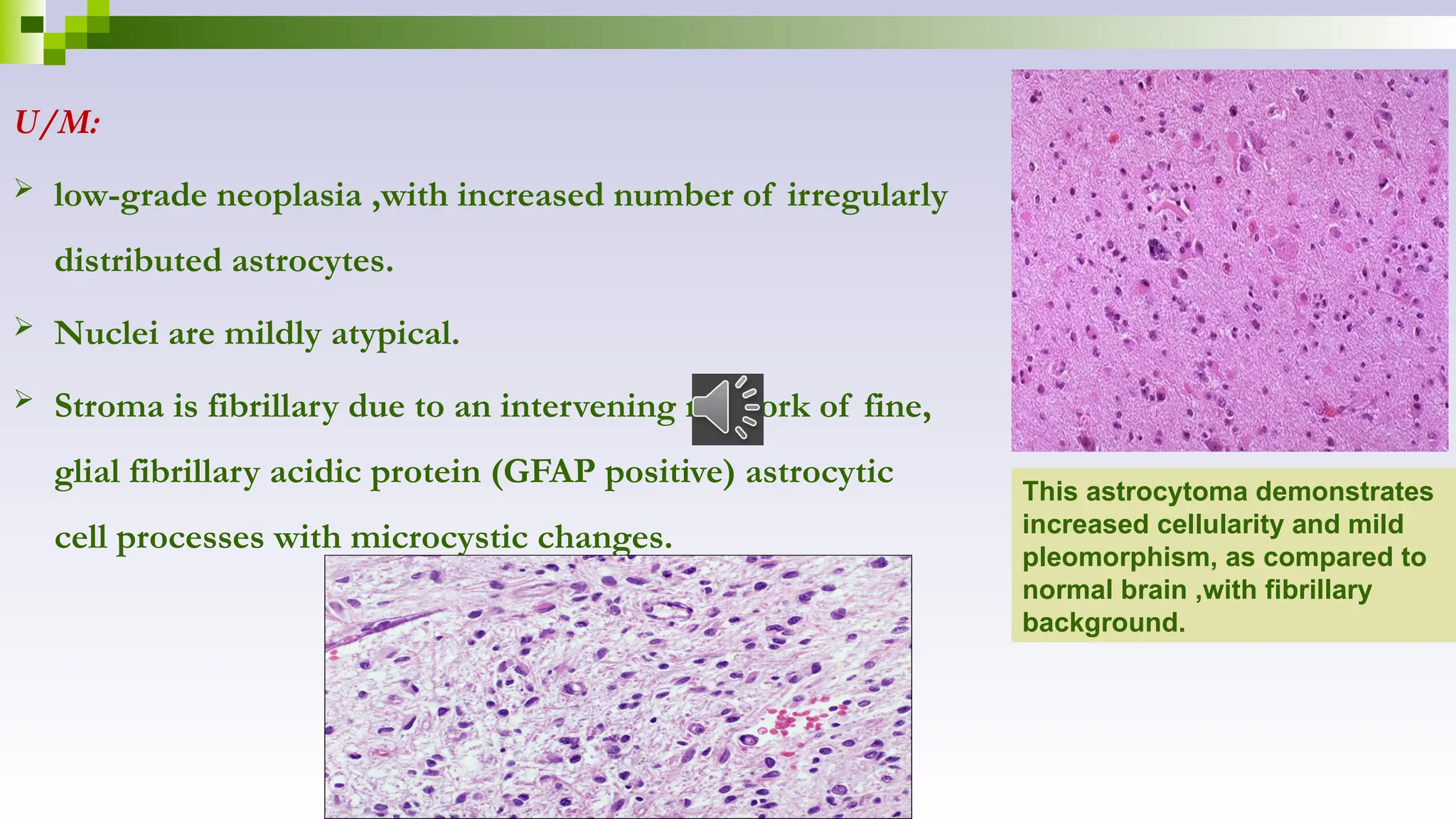
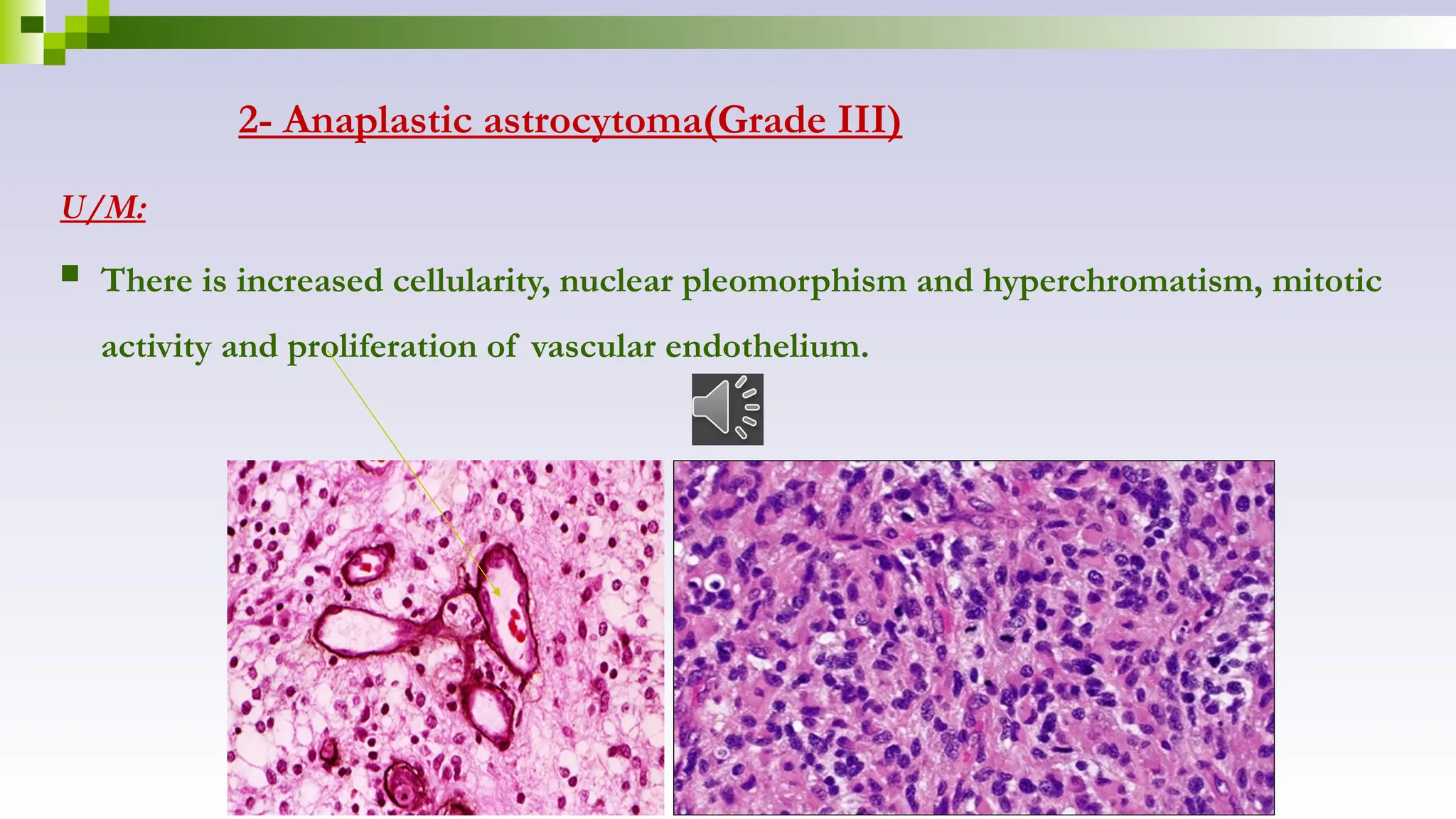
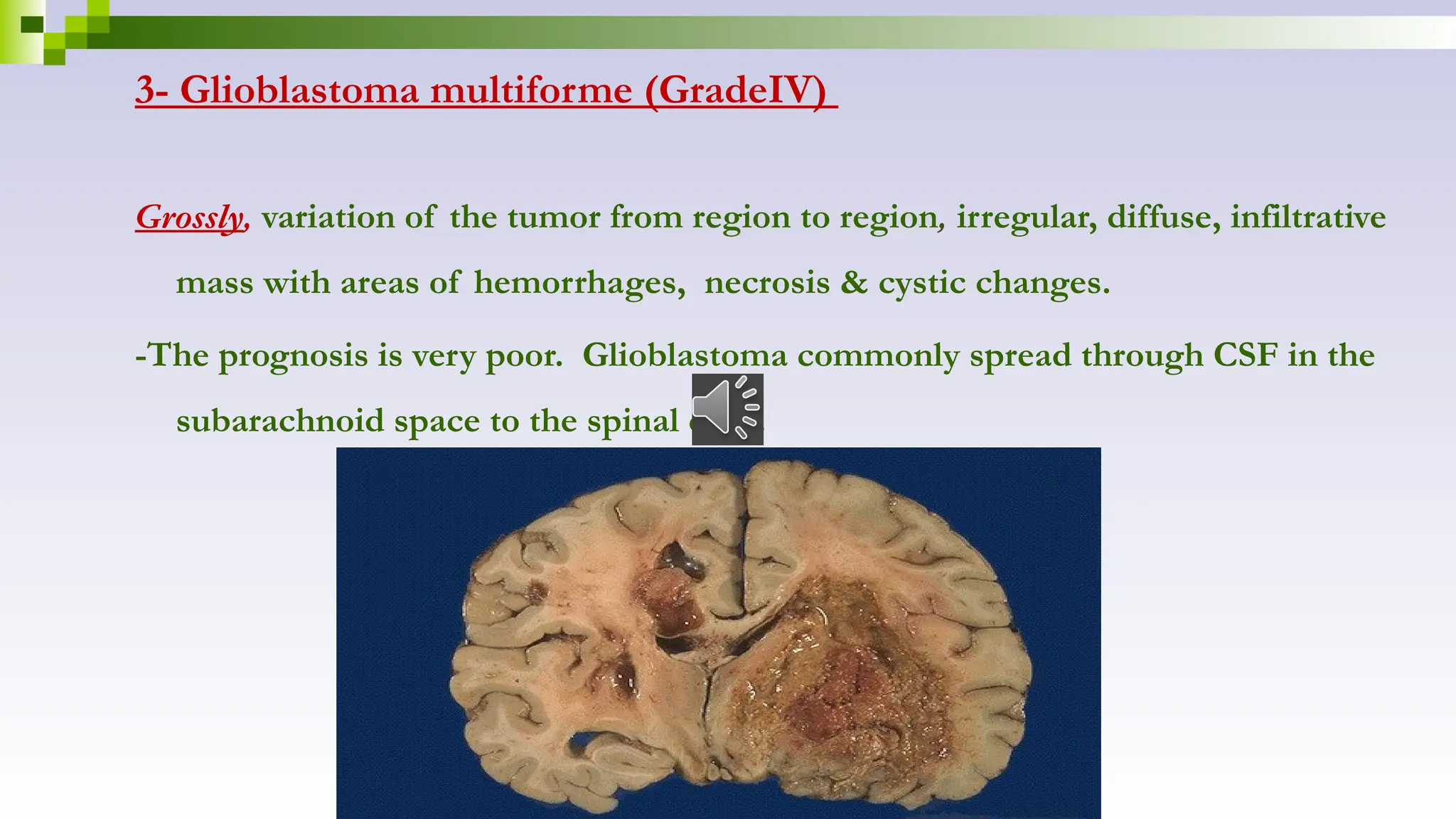
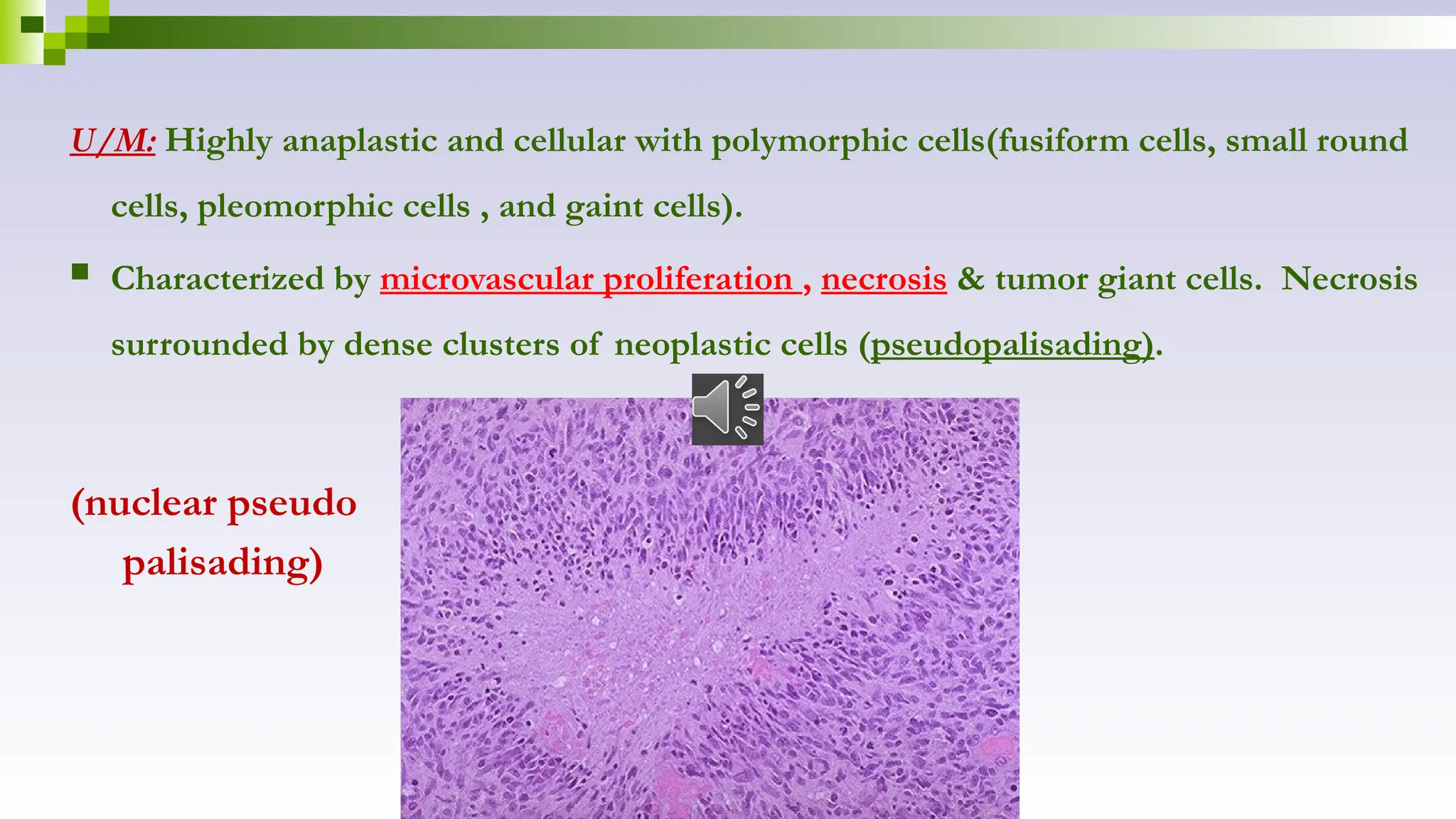
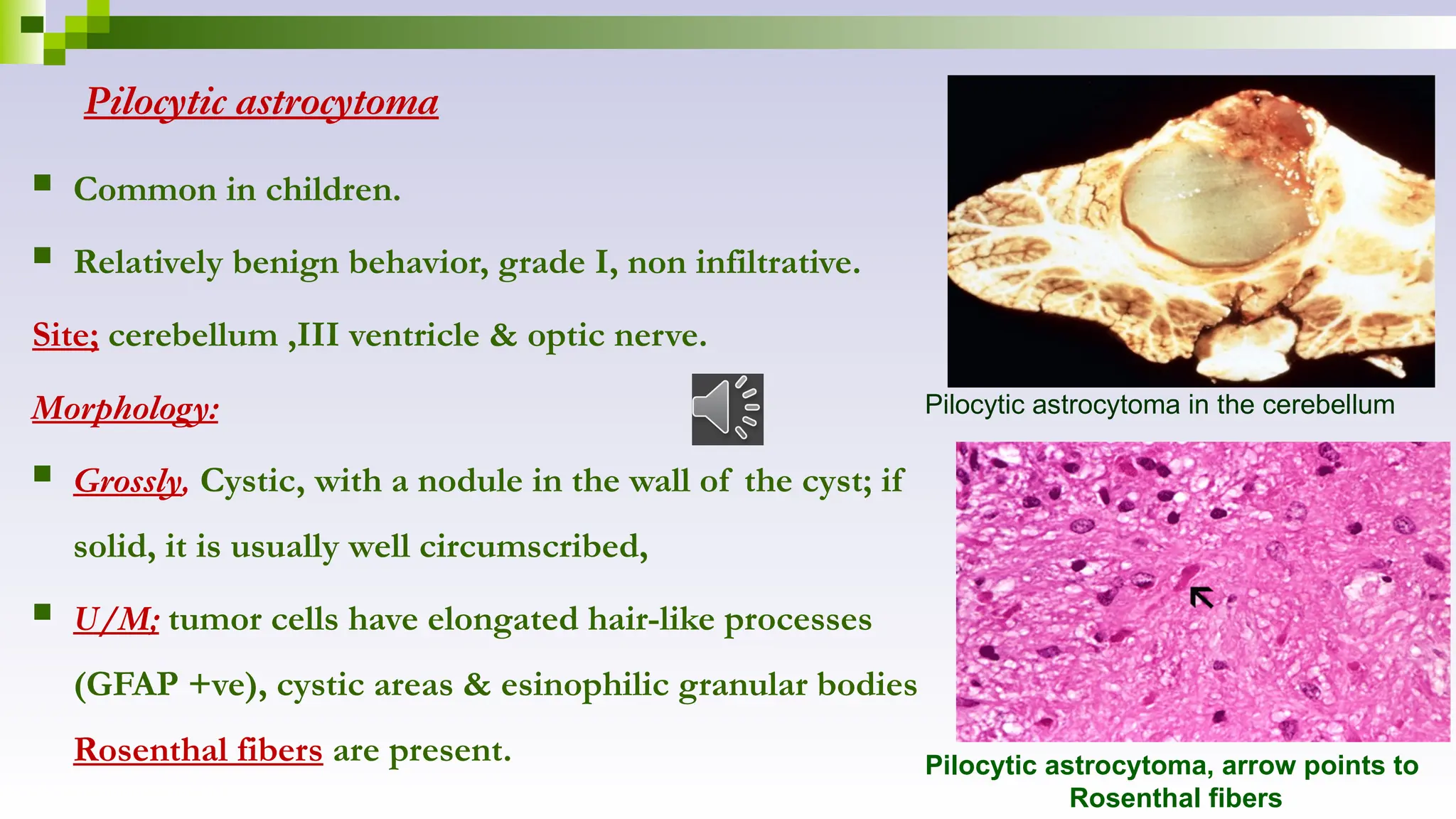
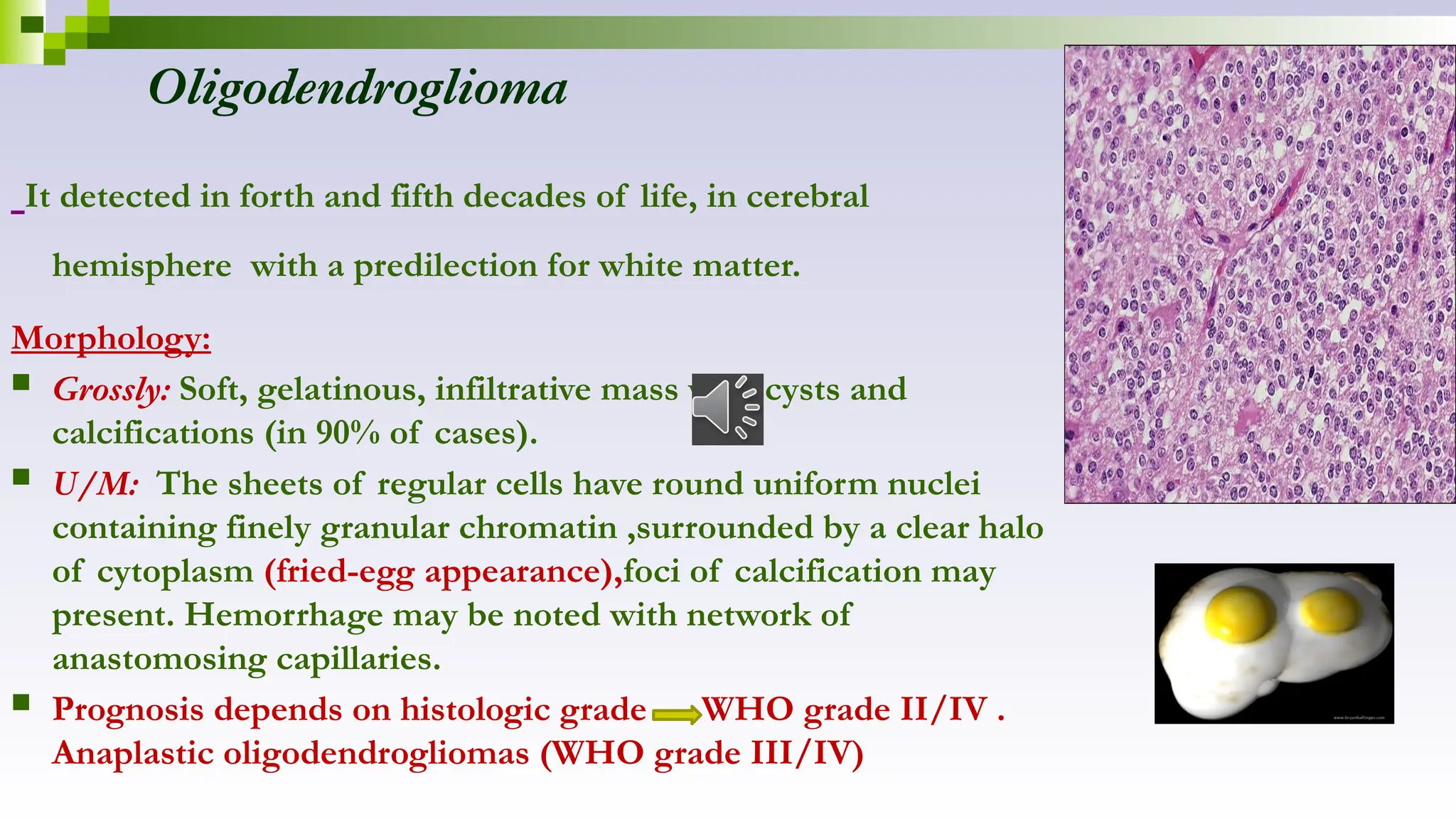
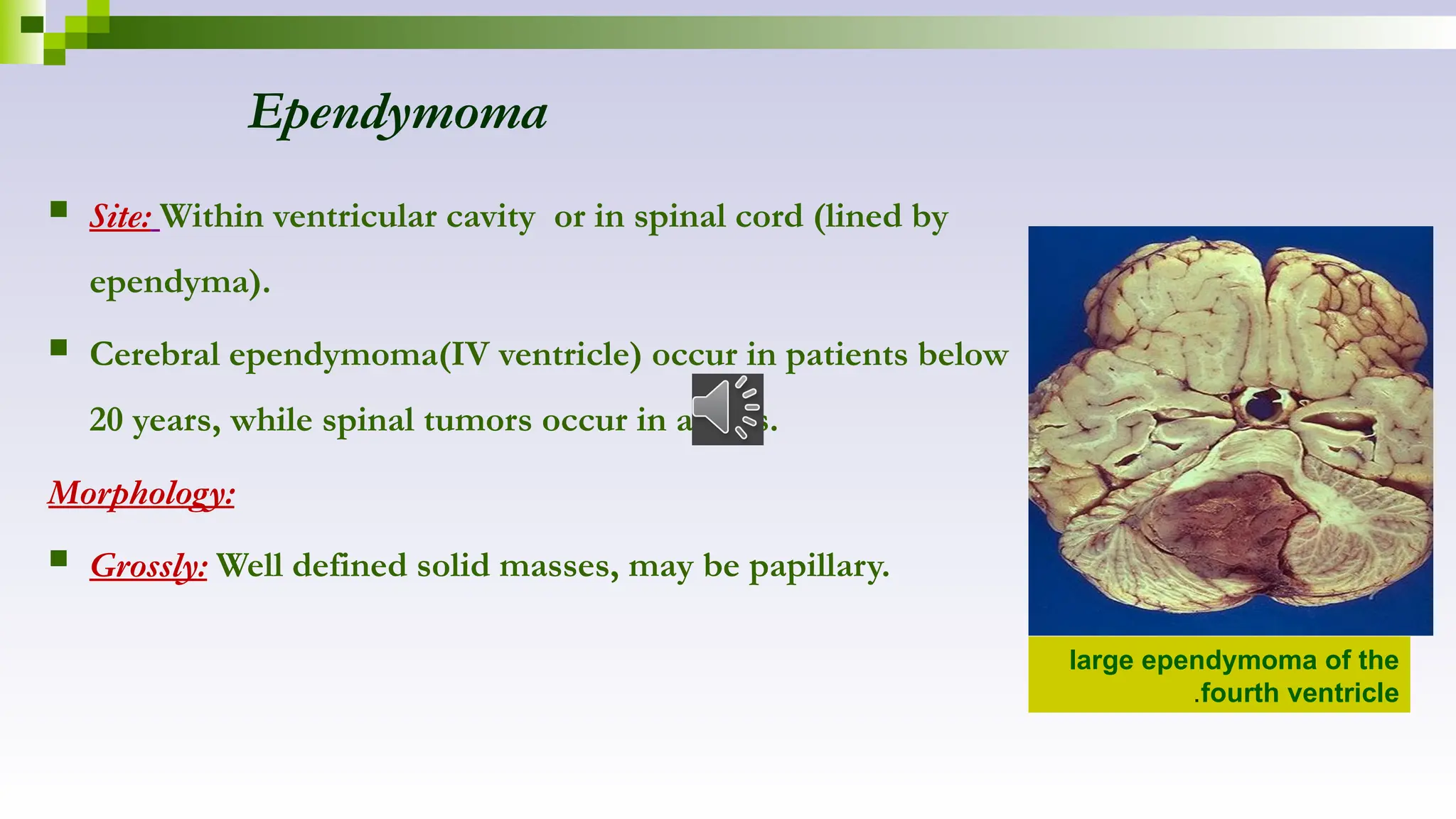
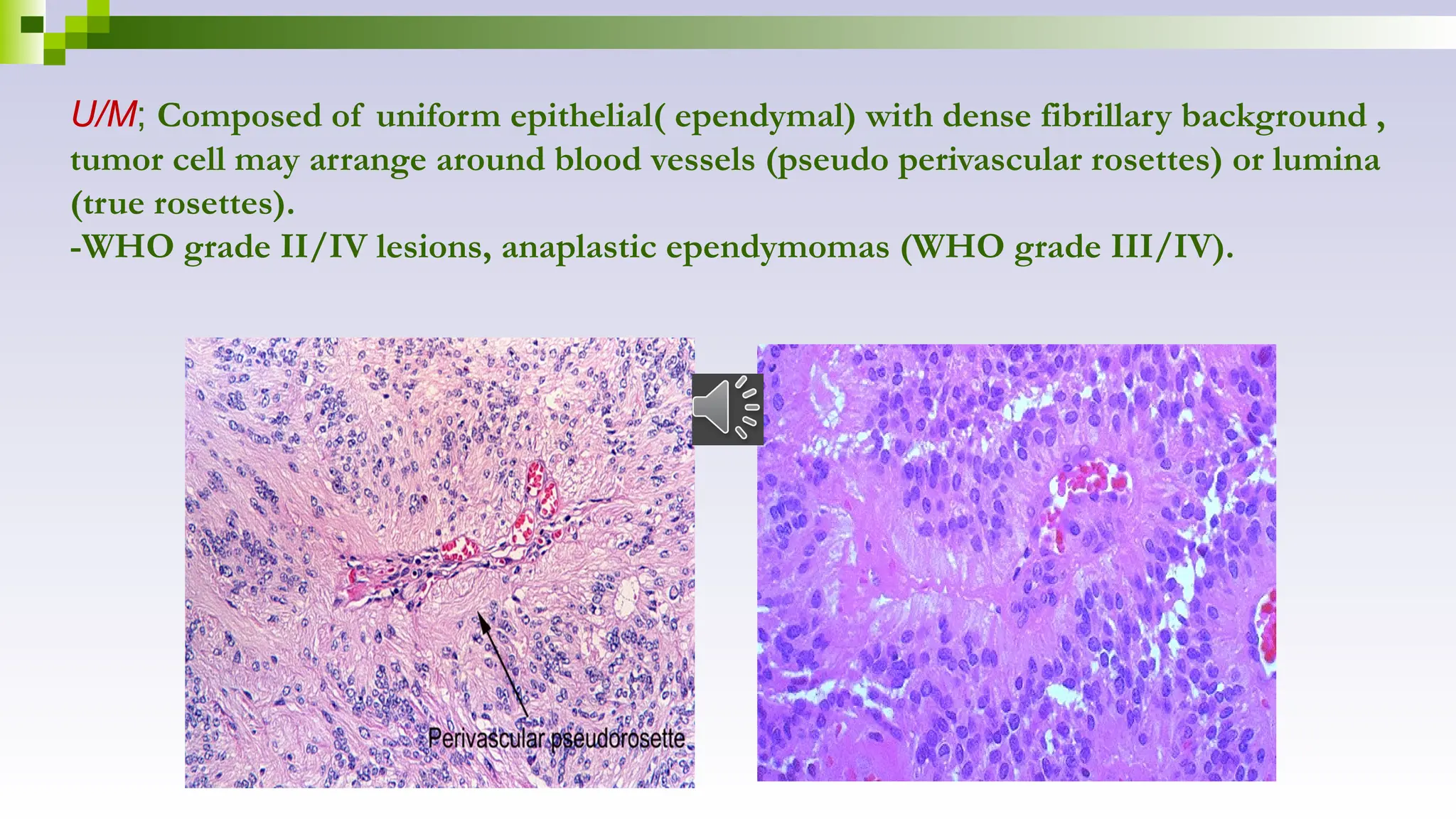
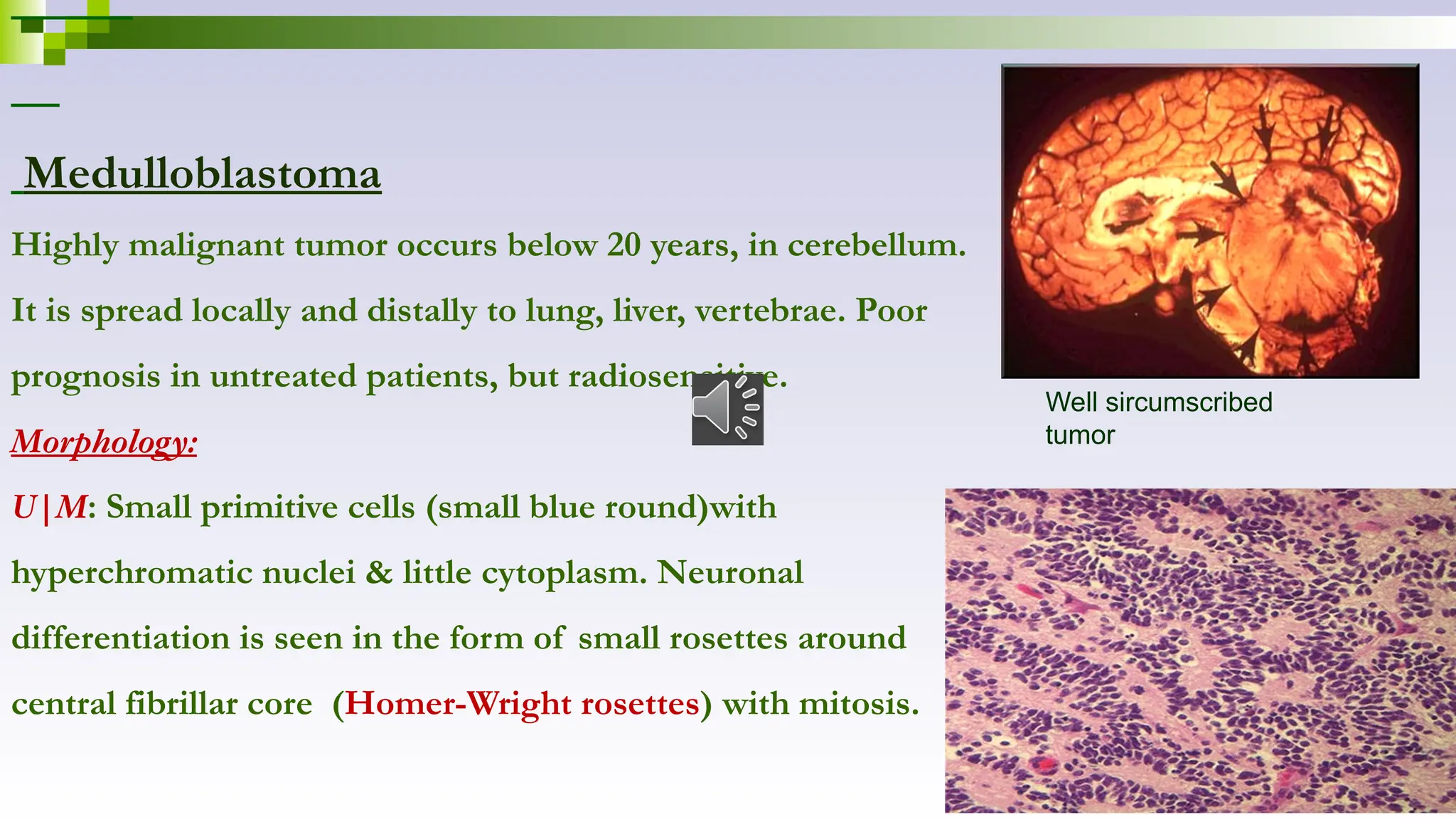
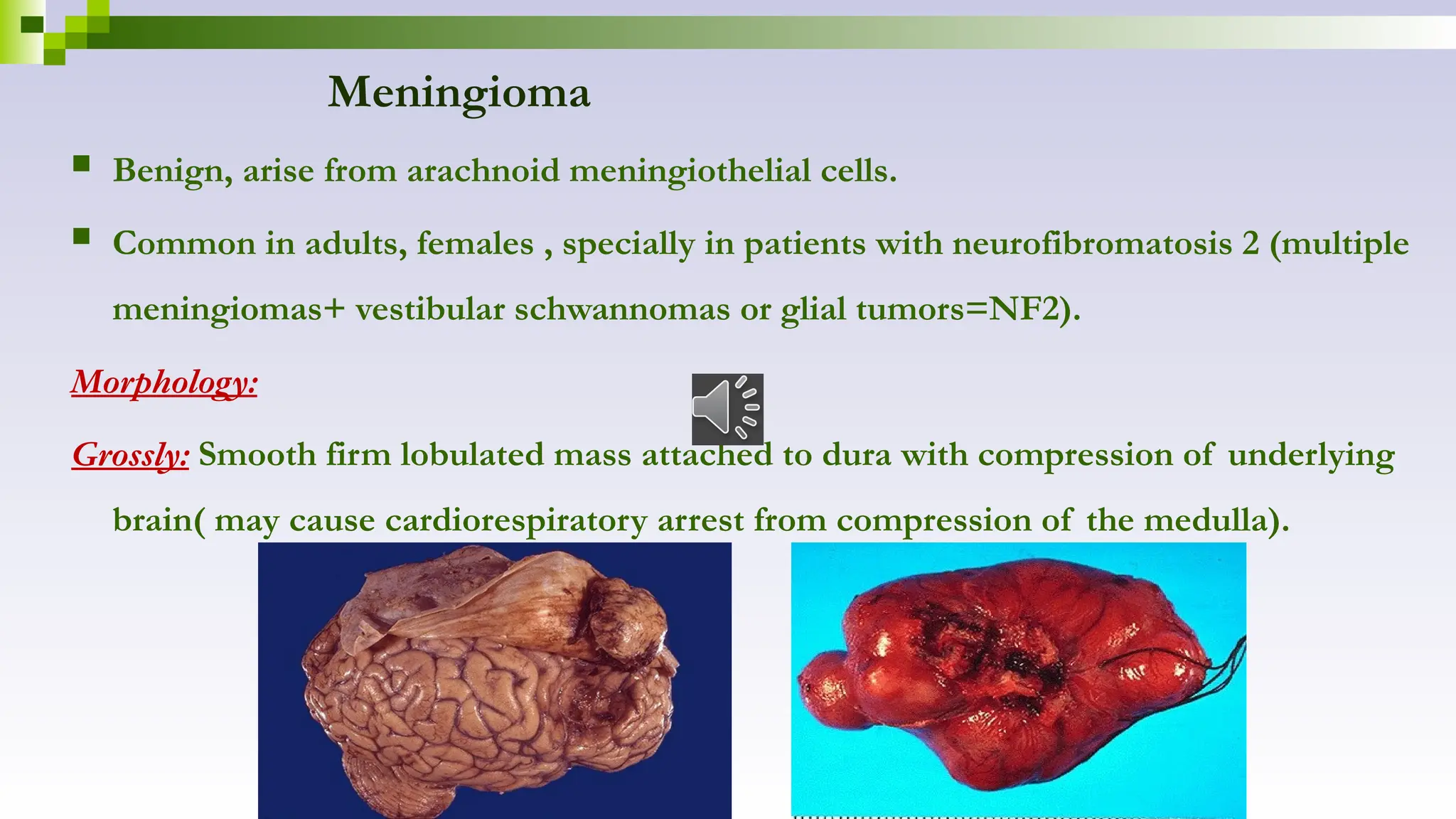
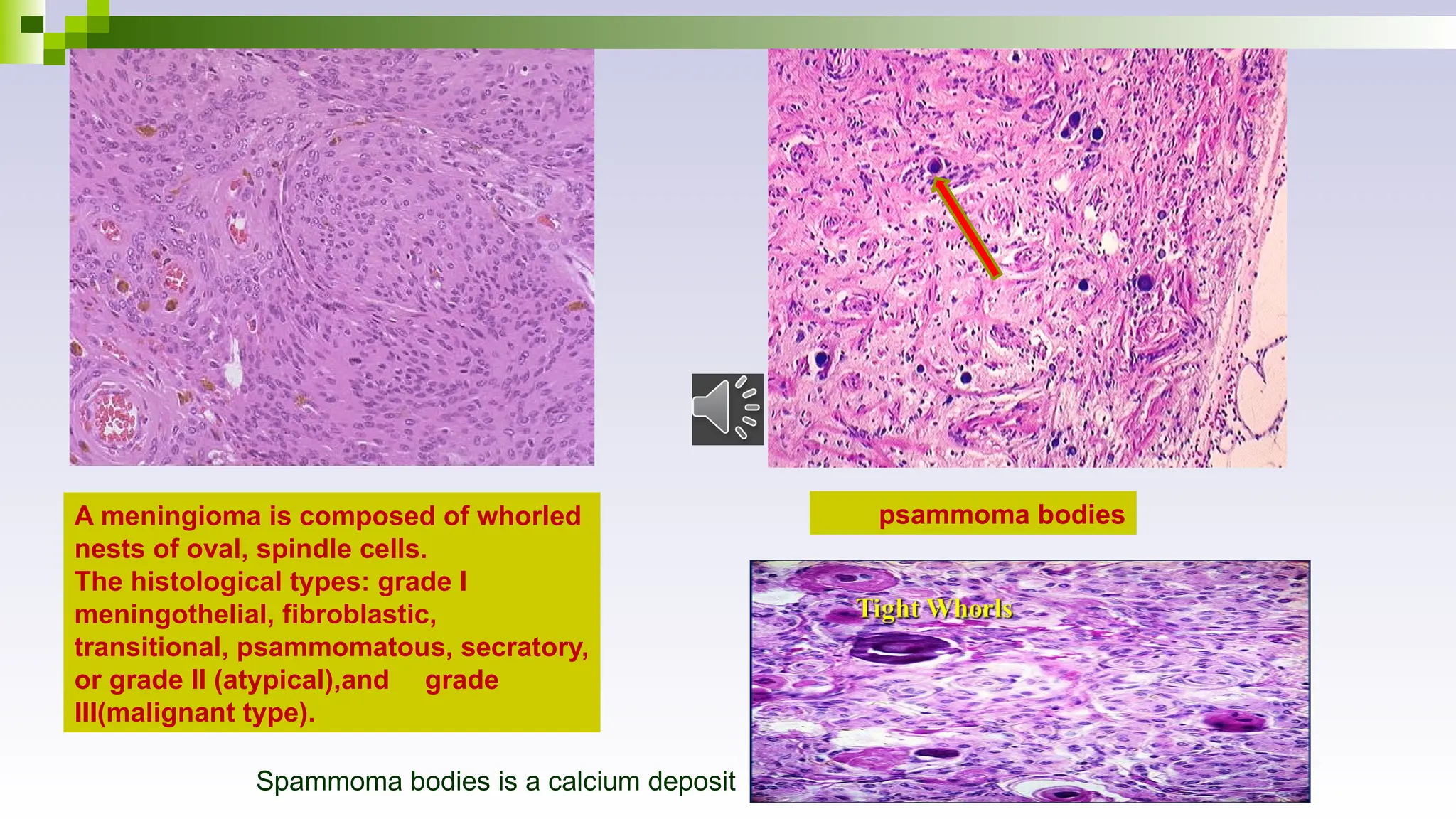
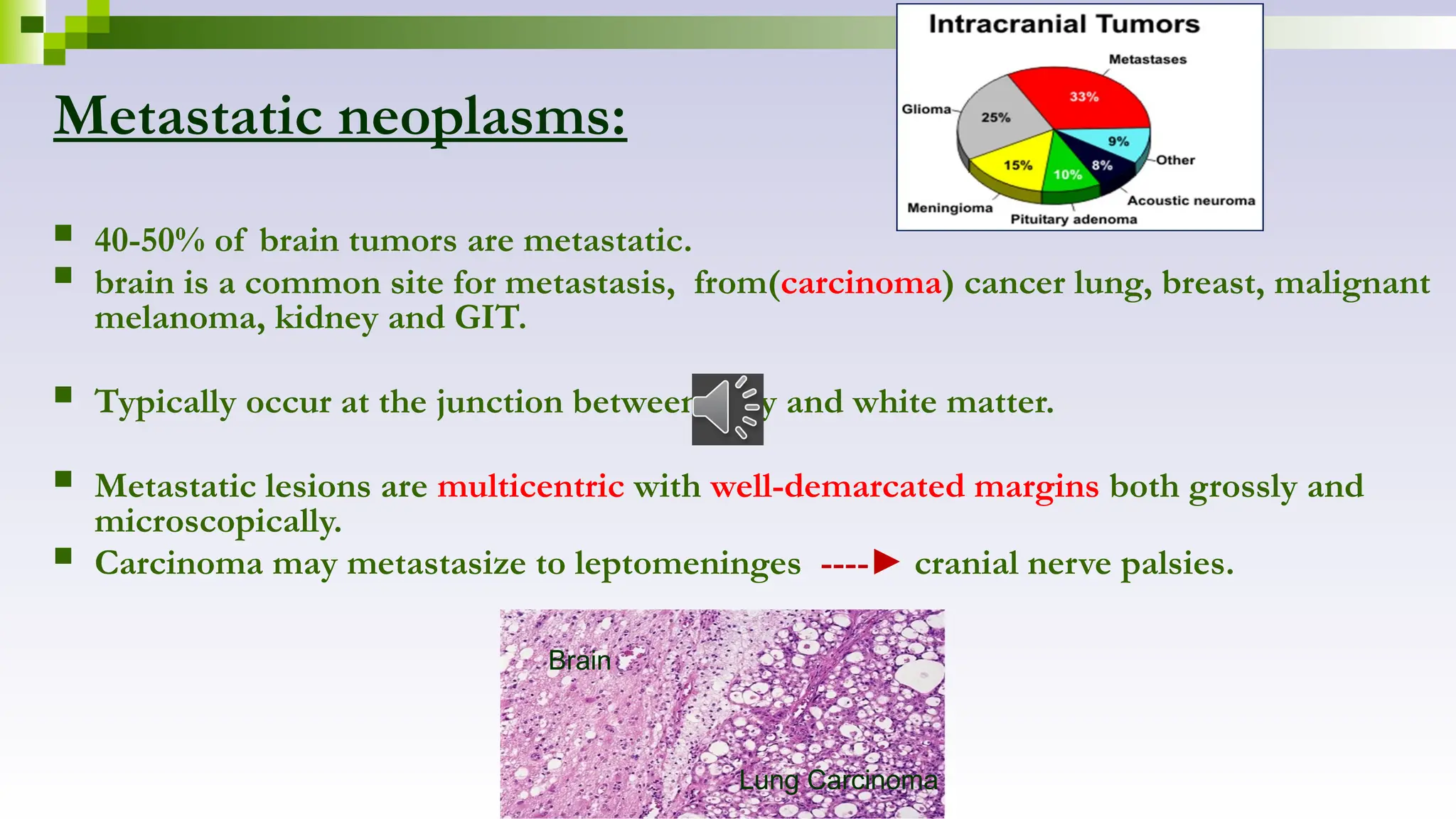
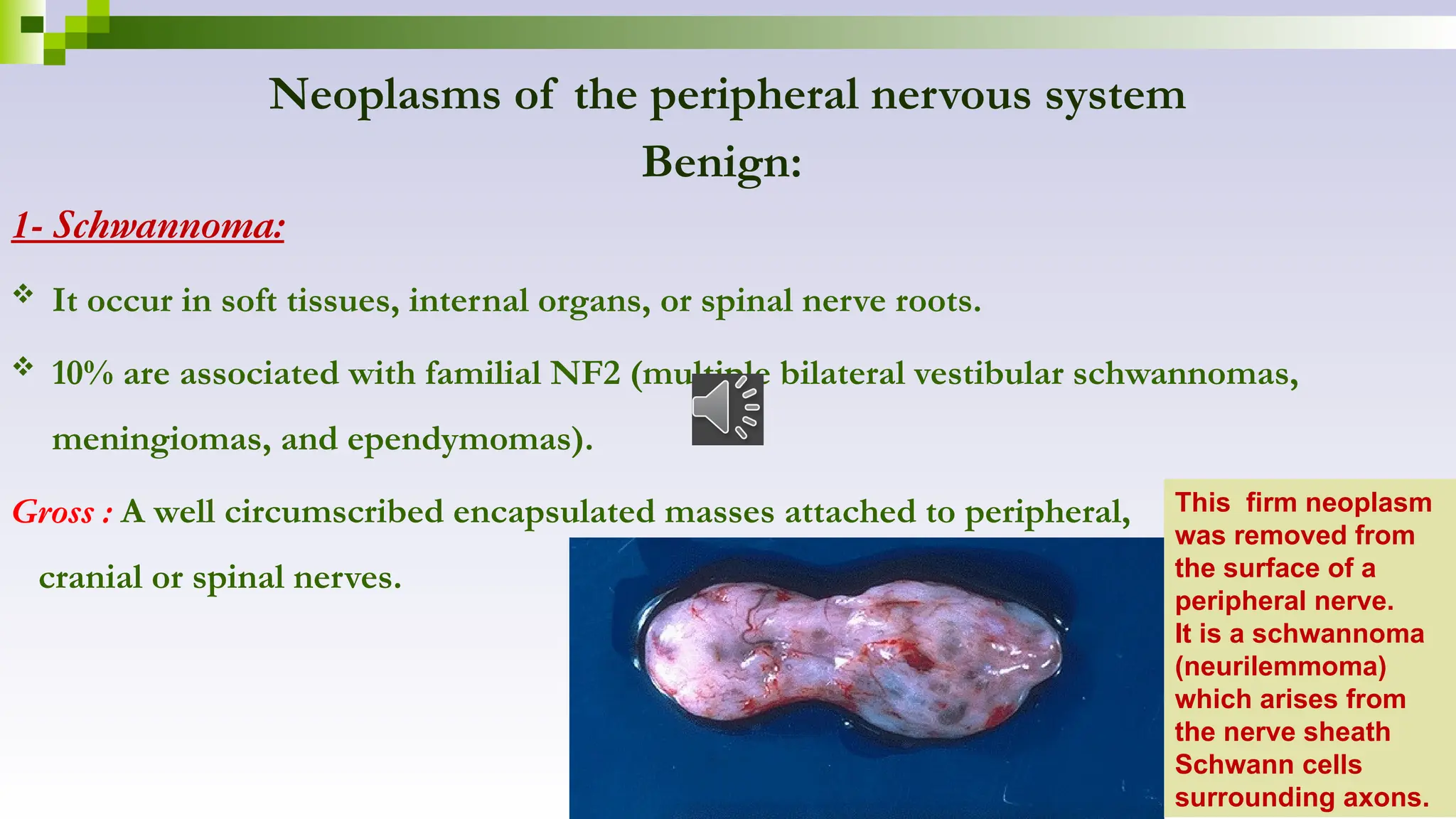
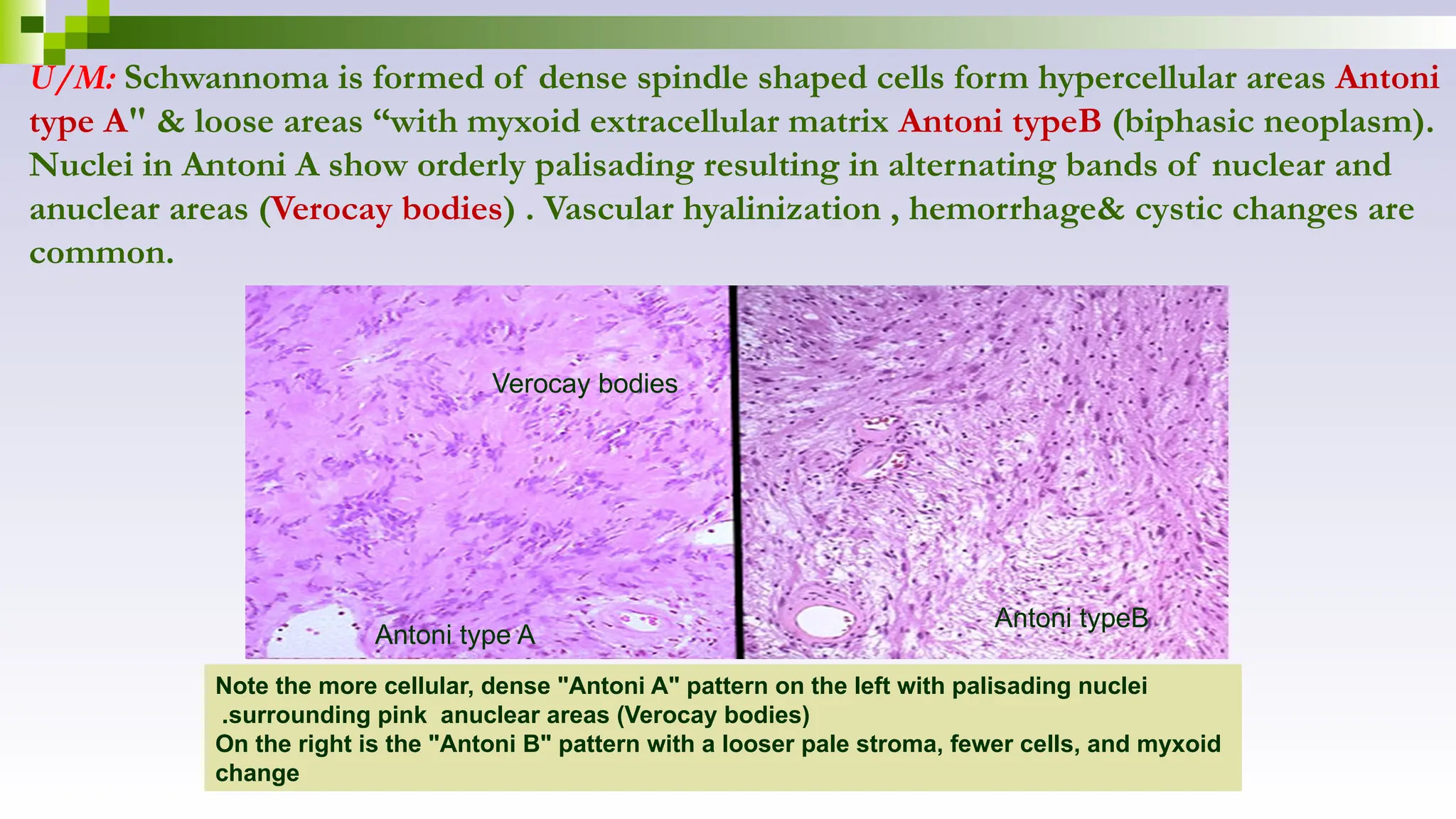
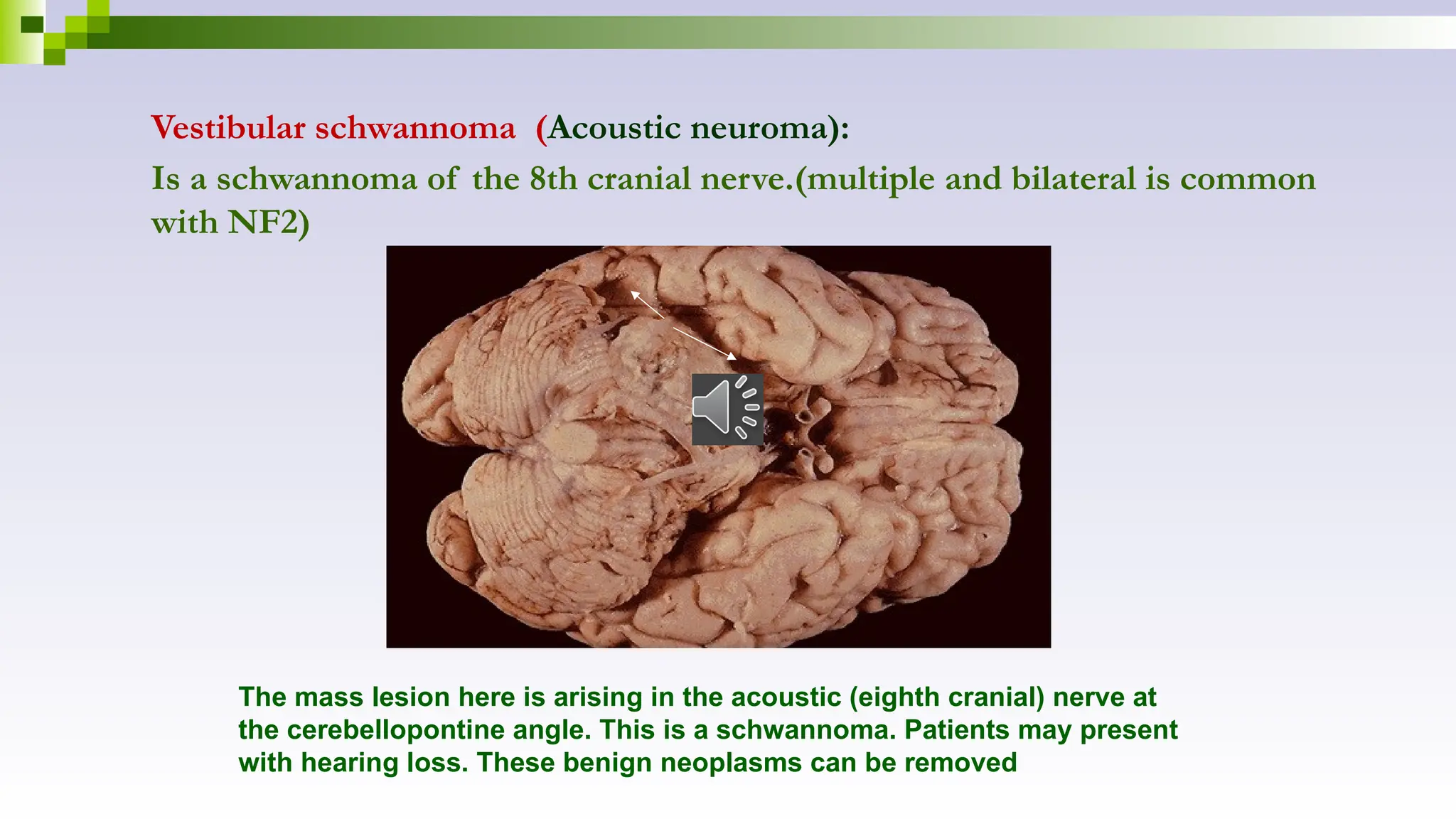
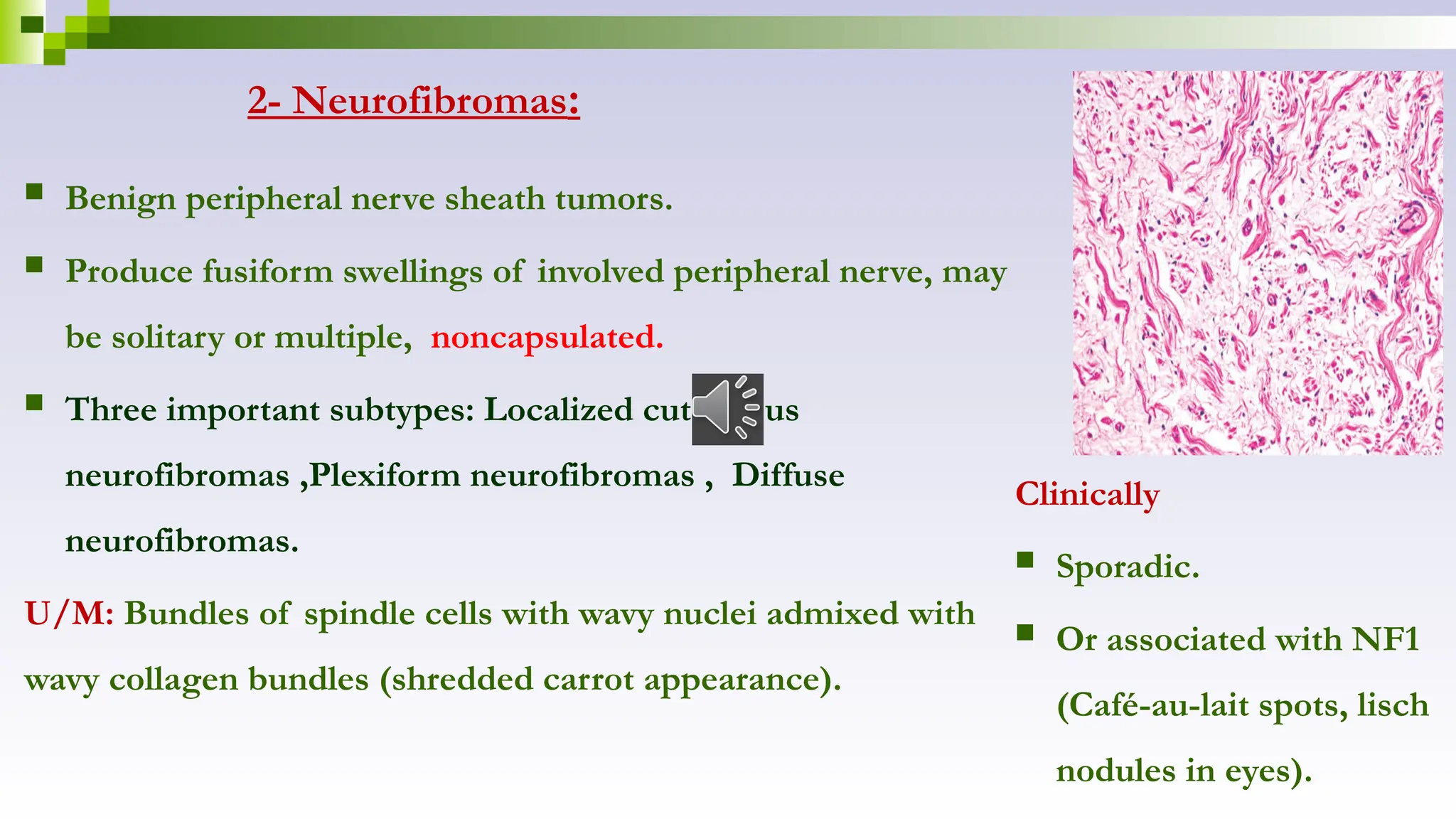
The document discusses various diseases affecting the central nervous system, including increased intracranial pressure, hydrocephalus, cerebral edema, vascular diseases, infections, and neoplasms. It highlights the causes, effects, and morphology related to these conditions, detailing the pathophysiology of ischemic brain damage and infections like meningitis and encephalitis. Additionally, the document covers types of CNS tumors, their classifications, and implications for treatment and prognosis.