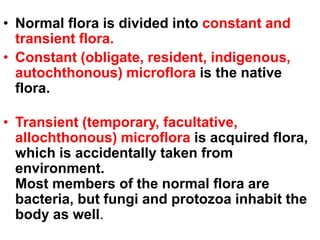
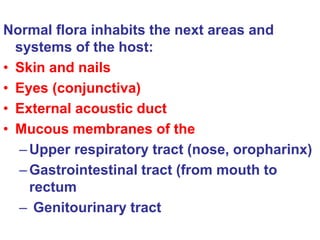
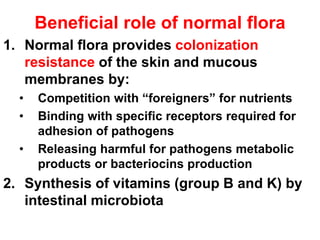
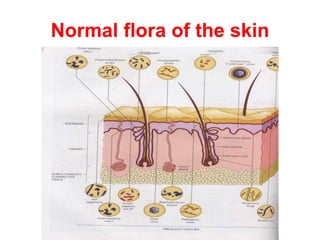
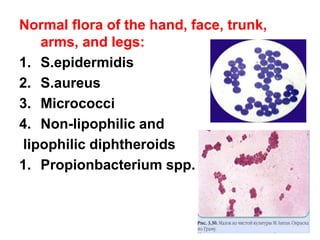
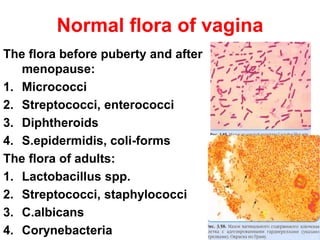
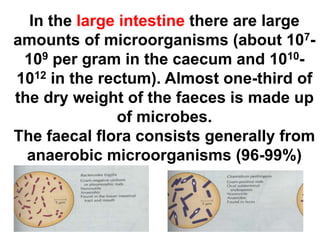
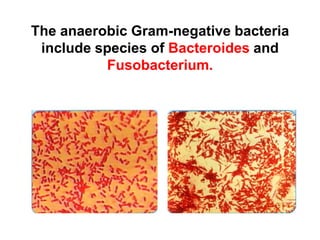
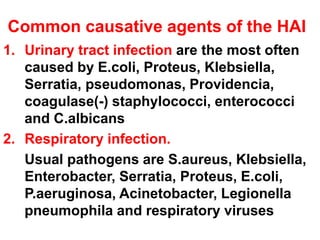
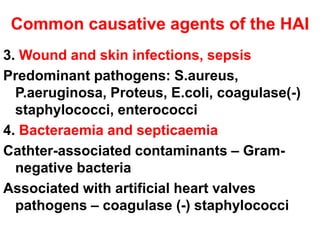
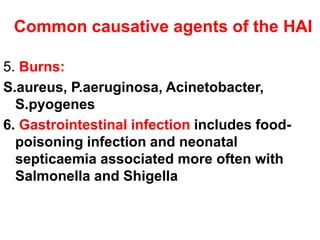
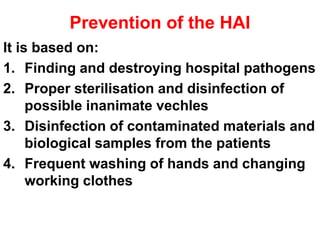
This document discusses clinical microbiology and normal human microbiota. It describes the major tasks of clinical microbiology as investigating opportunistic microorganisms that can cause hospital-acquired infections and developing rapid diagnostic tests. It then characterizes the normal microbiota found in different areas of the human body like the skin, respiratory tract, and gastrointestinal tract. Finally, it discusses hospital-acquired infections, identifying common pathogens and emphasizing prevention through proper sterilization, hand washing, and rational antibiotic use.