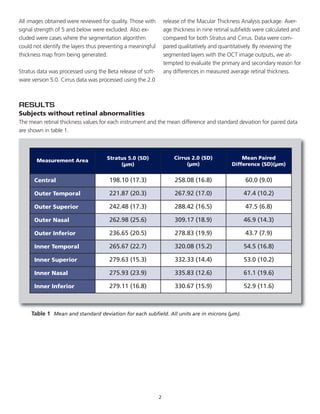
Differences between retinal thickness measurements from Cirrus HD-OCT and Stratus OCT range from 43-61 microns. This is primarily due to Cirrus measuring thickness from the RPE to ILM, while Stratus measures from IS/OS to ILM. For subjects without abnormalities, Cirrus typically measures 60 microns thicker in the central subfield. Differences are reduced for subjects with pathologies that disrupt the IS/OS or RPE boundaries. When comparing devices, it is important to examine the OCT images and morphology, not just quantitative values.