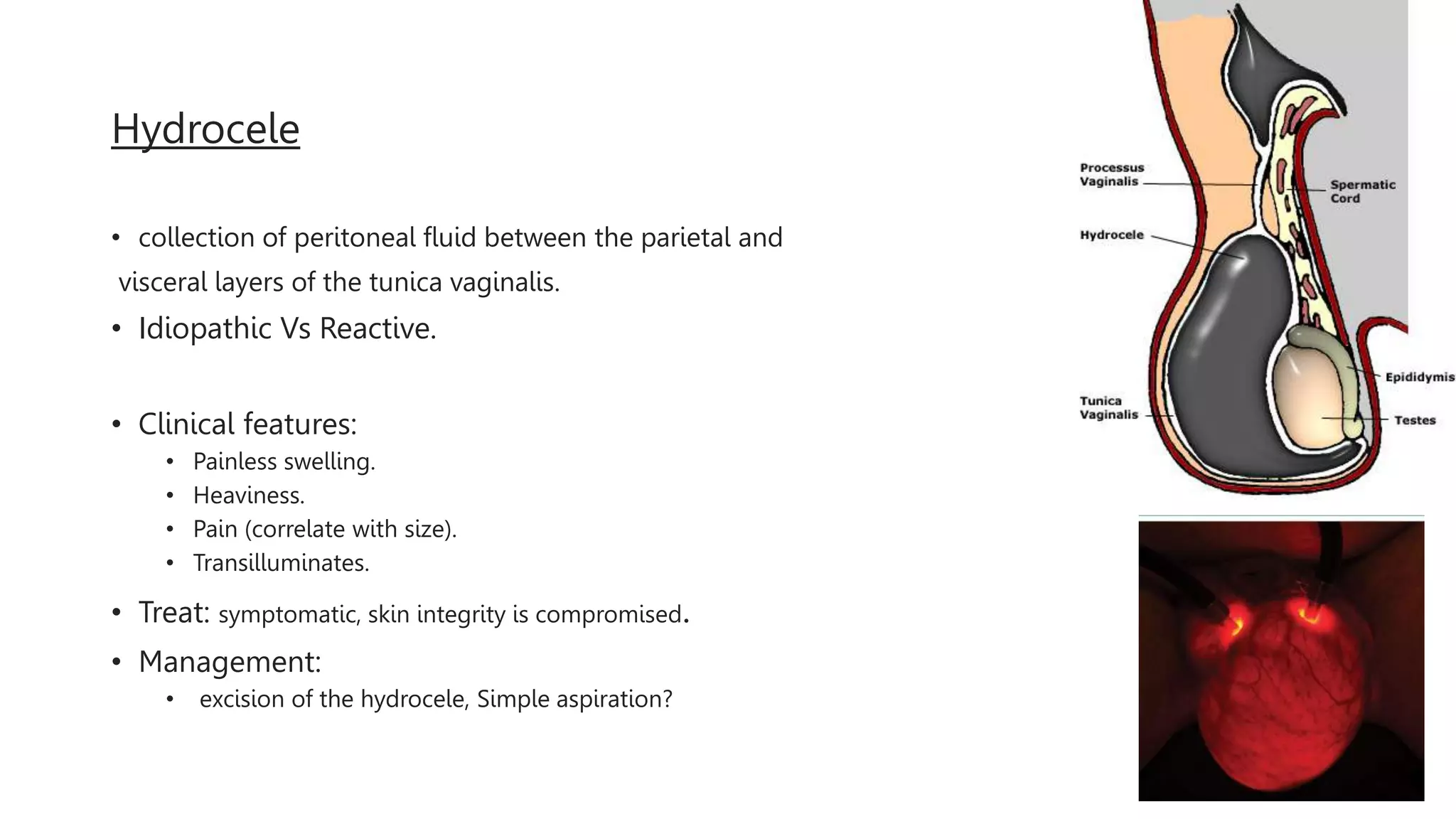
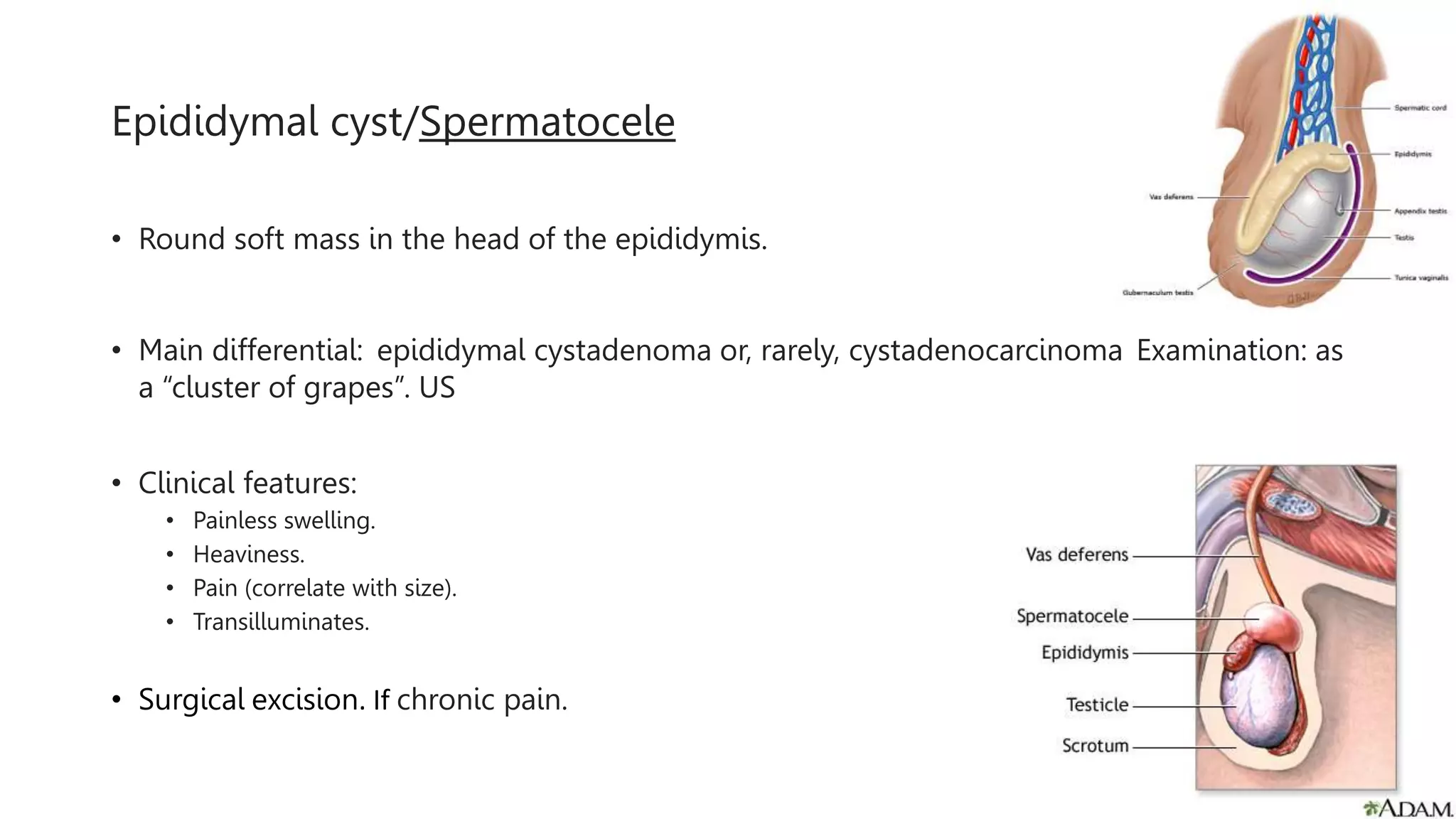
This document provides an overview of chronic scrotal pain. It defines chronic scrotal pain as intermittent or constant pain localized to the scrotal structures that lasts for 3 months or longer and significantly interferes with daily activities. Approximately 50% of cases will not have an identifiable cause. Common etiologies discussed include varicocele, hydrocele, epididymal cyst/spermatocele, and testicular cancer. Diagnosis involves a thorough history, physical exam, and imaging or lab tests when indicated based on exam findings. Treatment options discussed include conservative therapies like scrotal support, heat/cold, avoidance of aggravating activities, and psychological therapies. Medical management with NSAIDs, antibiotics, antidepressants,