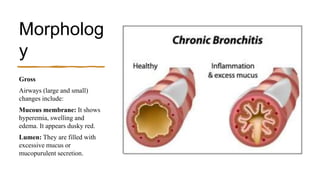
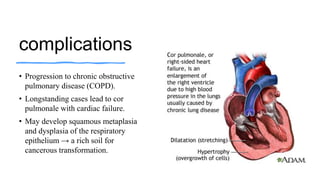
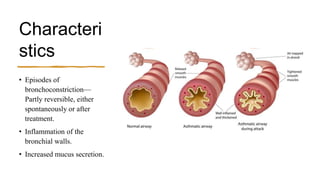
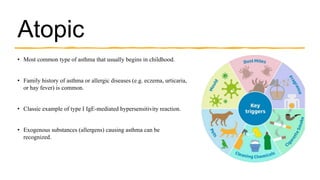
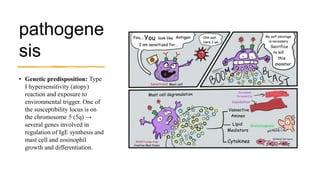
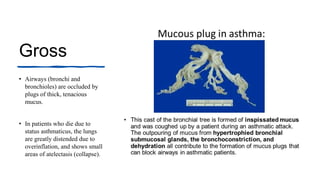
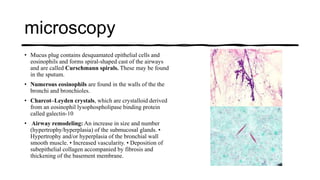
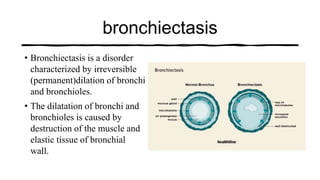
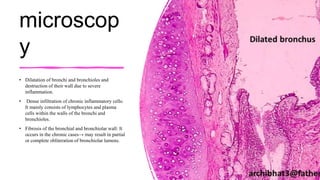
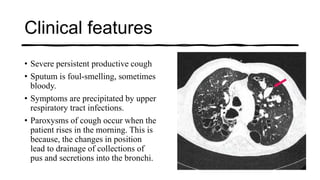
Chronic obstructive pulmonary disease (COPD) encompasses four main conditions, including chronic bronchitis, which is characterized by a persistent productive cough and mucus hypersecretion primarily caused by smoking and air pollution. Asthma is a chronic inflammatory disorder resulting in bronchoconstriction and increased mucus production, with two main types: atopic and non-atopic. Bronchiectasis involves irreversible dilation of bronchi due to destruction of muscle and elastic tissue, often resulting from chronic infections or genetic disorders like cystic fibrosis.