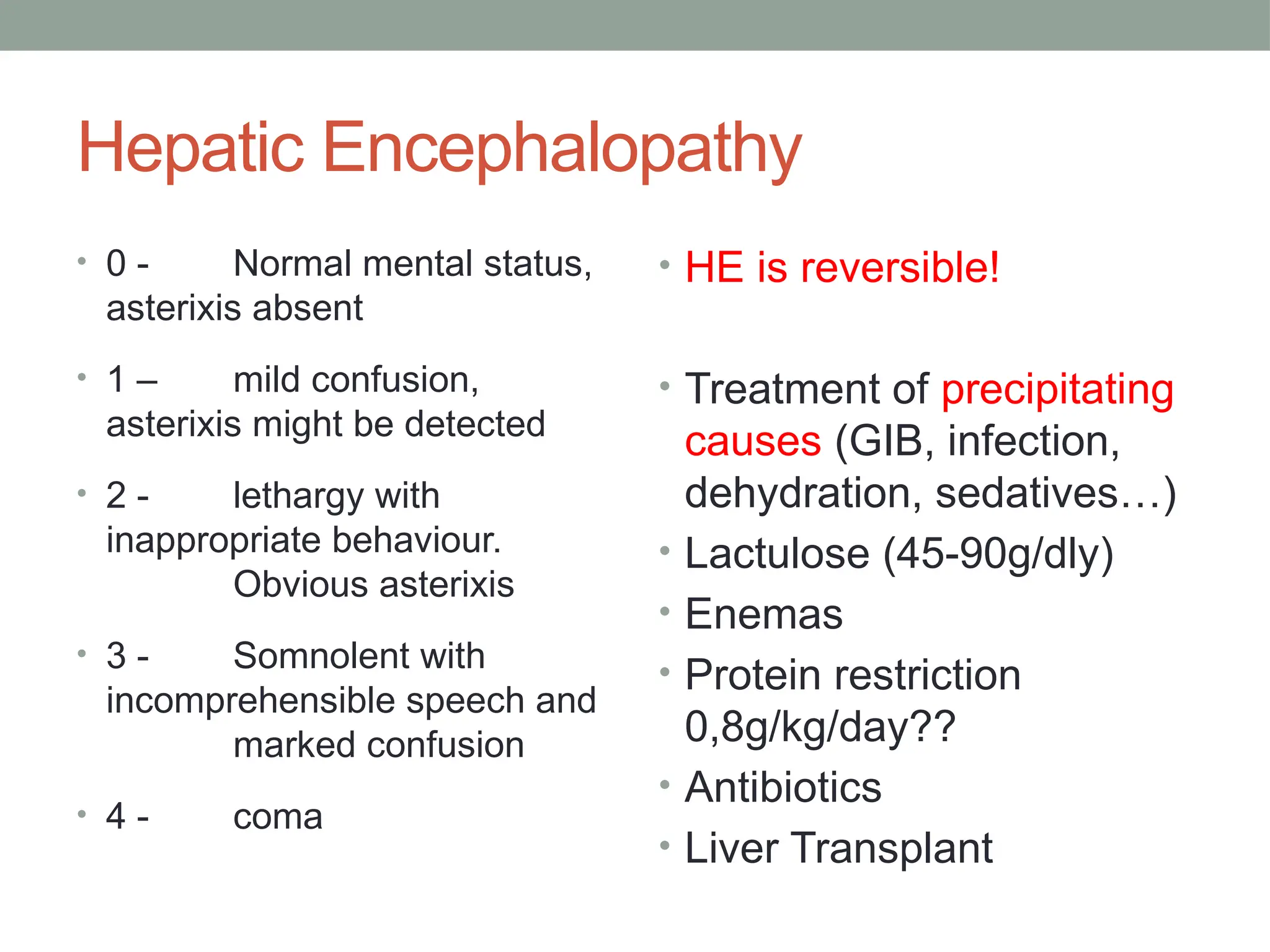
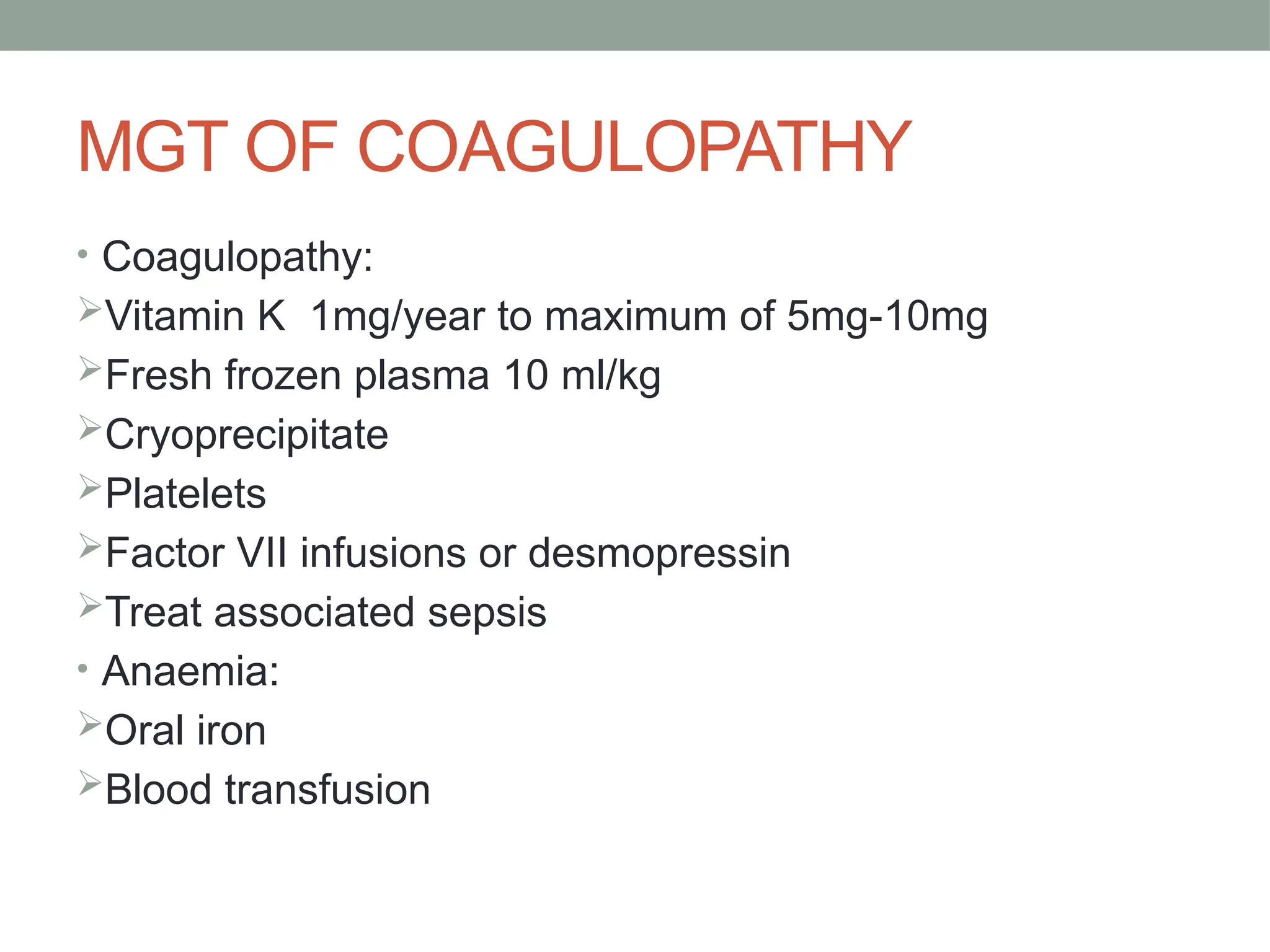
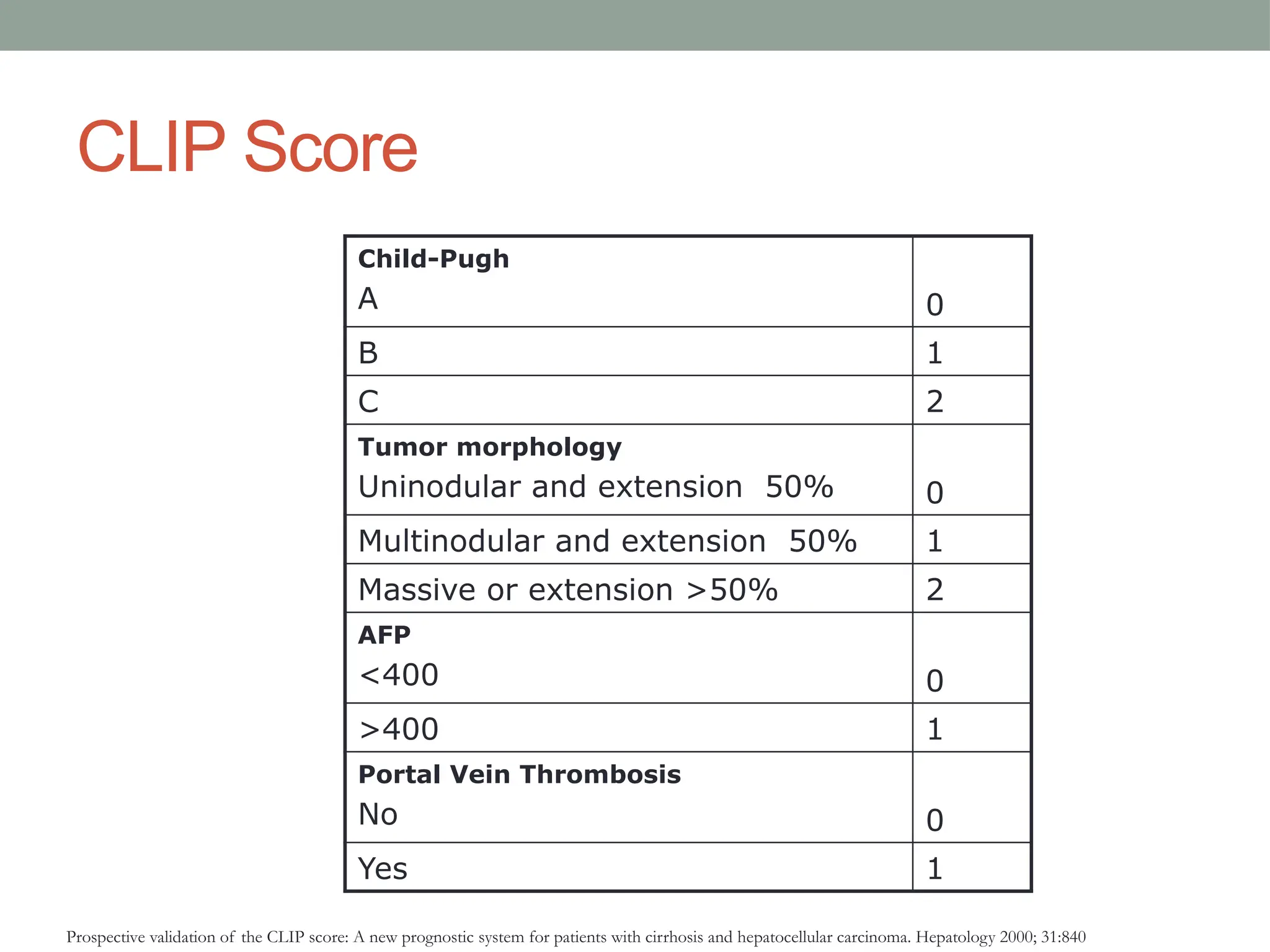
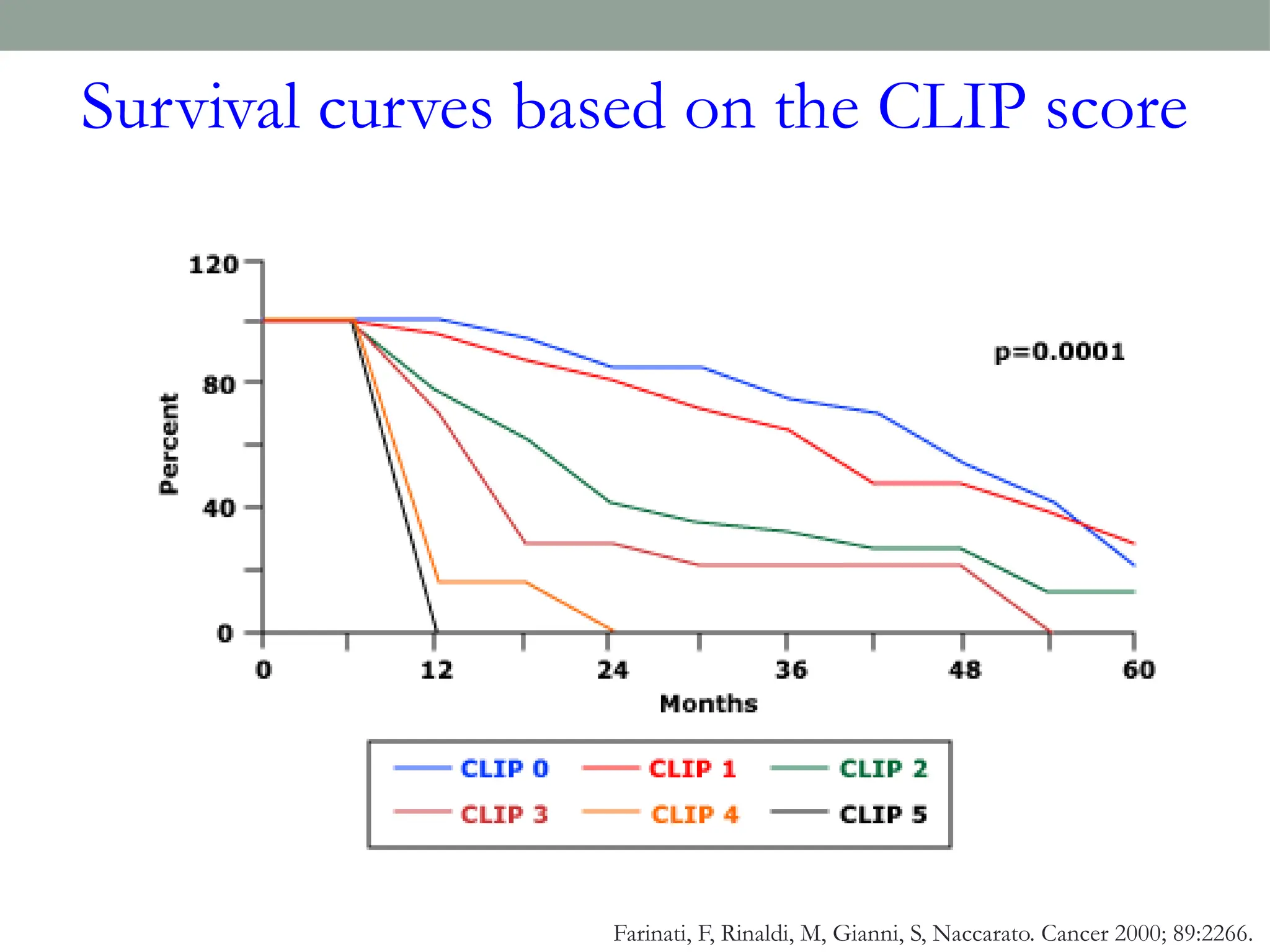
The document outlines chronic liver disease (CLD), detailing its definition, causes, symptoms, investigations, management, complications, and prognosis. It highlights the significance of liver function tests, imaging, and specific laboratory tests for diagnosis, while emphasizing the management strategies for conditions such as cirrhosis and portal hypertension. The prognosis for CLD depends on factors such as etiology, severity, and potential for liver transplantation.