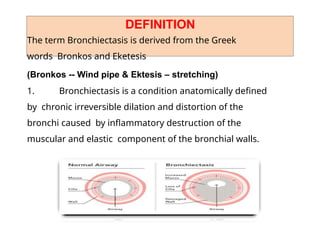
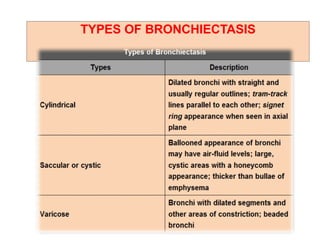
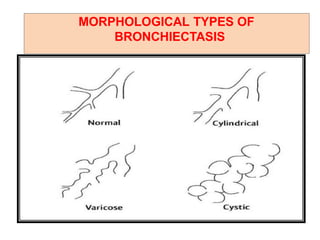
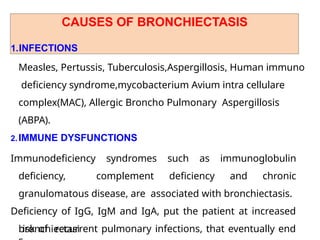
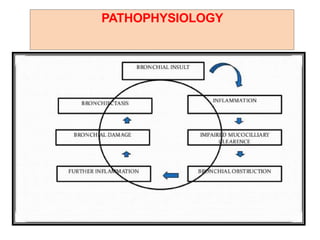
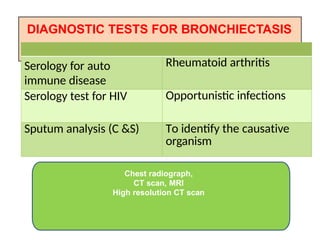
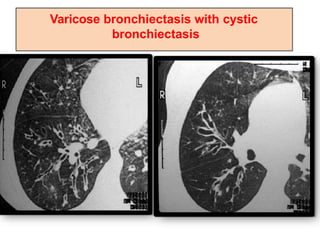
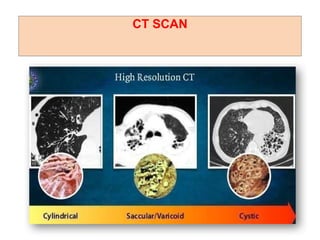
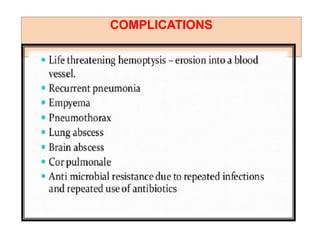
Bronchiectasis is a chronic lung disease marked by the irreversible dilation and distortion of the bronchi due to inflammation. Common causes include infections, immune disorders, cystic fibrosis, and broncholithiasis, leading to symptoms like increased sputum production and respiratory distress. Management includes antibiotics, bronchodilators, physiotherapy, and potentially surgical interventions for severe cases.