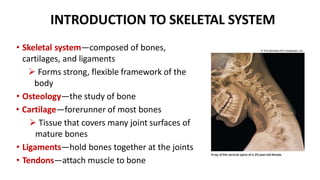
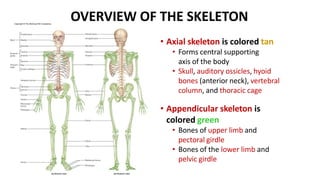
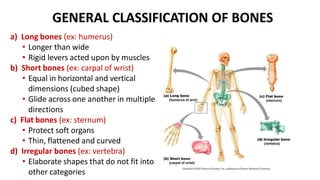
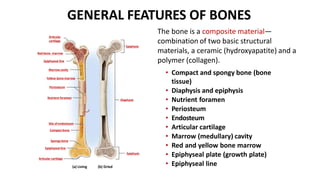
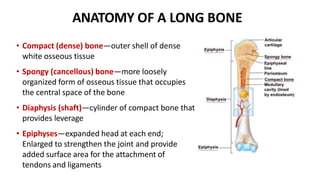
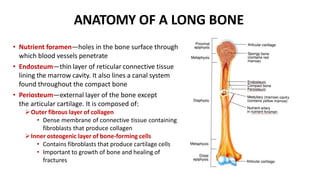
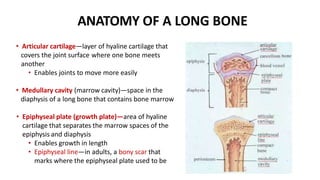
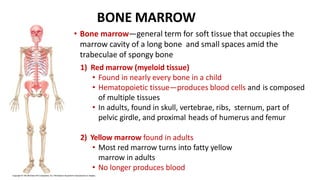
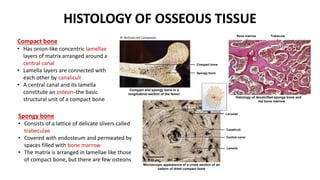
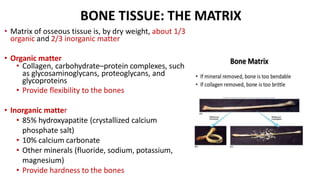
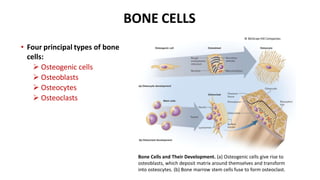
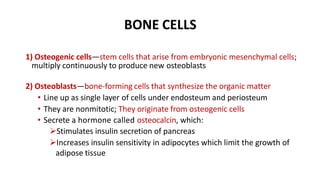
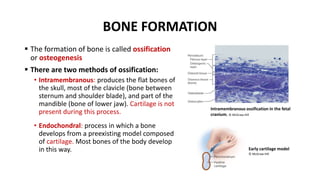
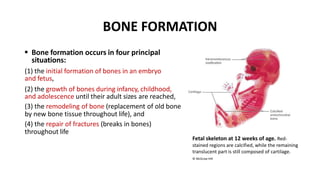
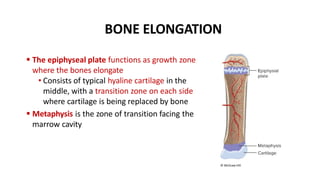
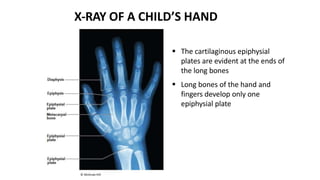
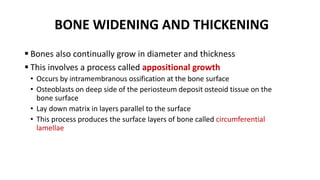
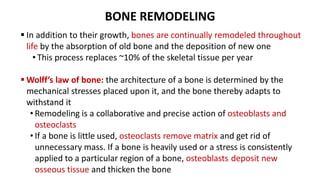
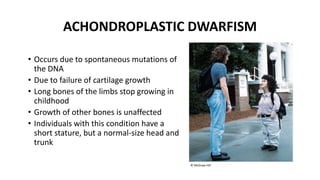
The document provides an overview of the skeletal system, including its components, functions, and the anatomy of bones. It discusses the classification of bones, types of bone tissue, and the various cell types involved in bone development and remodeling. Additionally, it details the processes of bone formation, growth, and related conditions such as achondroplastic dwarfism.