Case Study Analysis RubricNeeds DevelopmentFairGoodExcel.docx
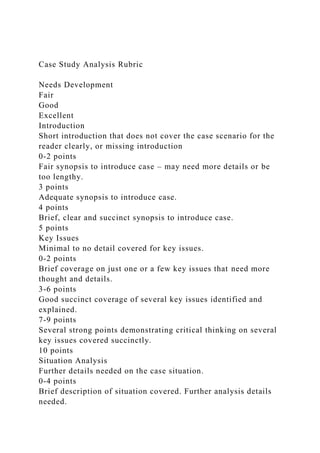
- 1. Case Study Analysis Rubric Needs Development Fair Good Excellent Introduction Short introduction that does not cover the case scenario for the reader clearly, or missing introduction 0-2 points Fair synopsis to introduce case – may need more details or be too lengthy. 3 points Adequate synopsis to introduce case. 4 points Brief, clear and succinct synopsis to introduce case. 5 points Key Issues Minimal to no detail covered for key issues. 0-2 points Brief coverage on just one or a few key issues that need more thought and details. 3-6 points Good succinct coverage of several key issues identified and explained. 7-9 points Several strong points demonstrating critical thinking on several key issues covered succinctly. 10 points Situation Analysis Further details needed on the case situation. 0-4 points Brief description of situation covered. Further analysis details needed.
- 2. 5-9 points Adequate case situation explained that also incorporates several areas of significance. 10-14 points Detailed description summarizes the situation and covers probable causes and/or significant areas. Critical thinking is evident. 15 points Organizational Strategy Brief suggestion or two with impact of ideas on organizational strategy attempted. 0-4 points Two short suggestions addressed to consider and some elements of organizational strategy impact covered. More details needed. 5-9 points Elements of applicable organizational strategy covered for two suggestions that include pros/cons to consider and possible impact. 10-14 points Elements of applicable organizational strategy to consider for three alternatives along with pros/cons and any possible ramifications of suggestions. 15 points Implementation Plan Further specifics and details needed on how to put suggestion(s) into place. Information may be brief or missing. 0-5 points At least one feasible and realistic suggestion explained. 6-13 points Several implementation suggestions covered in depth that incorporate some time elements to put ideas into place. 14-19 points Detailed suggestions on how to implement recommendations that include time frames and possible contingency plan. Critical thinking demonstrated. 20 points
- 3. Benchmarks to Measure Success Further details needed. Benchmark suggestions may be brief or missing. 0-4 points Brief monitoring points are addressed to measure progress and success. 5-9 points Some realistic monitoring plan suggestions are covered. 10-14 points Monitoring and measure action plan suggestions show insight and are realistic to demonstrate critical thinking. 15 points Scholarly Research of Literature Required scholarly research of literature was not met. Some research attempt evident,and/or only text is referred to. 0-5 points Credible outside research evident. Two scholarly research sources may not have been met. 6-13 points Scholarly research for two recent peer-reviewed journal articles was met. Other credible outside research may be evident. 14-19 points Scholarly research for three recent peer-reviewed journal articles was met and applied in various elements of analysis. There may be additional credible outside research support applied. 20 points Writing Mechanics More than 11 writing errors including grammar, punctuation, and spelling. Writing may be unfocused and contain serious errors, lacks detail and information, and may be poorly organized. 0-4 points 5-10 writing errors including grammar, punctuation, and spelling. Writing may not be clear or concise, contains numerous errors, lacks information and/or organization.
- 4. 5-9 points 1-4 writing errors including grammar, punctuation, and spelling. Writing is accomplished and contains only a few errors. Includes sufficient details and well organized. 10-14 points Free of writing errors including grammar, punctuation, and spelling. Writing is organized, clear and concise with thorough details. 15 points APA Have over 12 APA issues. 0-4 points 6-11 APA issues 5-9 points 2-5 APA issues 10-14 points Zero to 1 APA issues – Proper APA format used, and APA reference sources and in-text cites requirements met. Headings applied for rubric areas. 15 points 5 8 9 C A S E Dr. Louis Mickael: The Physician as Strategic Manager Industry Background
- 5. In the early 1900s, hospitals were perceived by the majority of the population in the United States as places where very sick people went to die. However, in the past five decades, rapid progress in medical technology, knowledge base, and expertise enhanced professional capability, and the public then demanded high levels of health care services. In 50 years, many demographic changes occurred. The popu- lation, longevity, and standard of living continued to increase. To address the needs of this changing population, government health care insurance programs for the older and needy segments of society were instituted. Private insurance companies prolifer- ated, and although workers had begun to expect employers to share with them the financial responsibility for their health serv- ice needs, employers were searching for less expensive ways to provide such care. The government was also attempting to reduce costs associated with the insurance programs it sponsored. This case was written by C. Louise Sellaro, Youngstown State University. It is intended as a basis for classroom discussion rather than to illustrate either effec- tive or ineffective handling of an administrative situation. The names of firms, individuals, locations, and financial information have been disguised to preserve the organization’s desire for anonymity. Presented and accepted for the Refereed Society for Case Research. All rights reserved to the author and SCR. Copyright © 1992 by C. Louise Sellaro. Used with permission of Louise
- 6. Sellaro. 8 both08.indd 589both08.indd 589 11/11/08 11:46:24 AM11/11/08 11:46:24 AM C A S E 8 : D R . L O U I S M I C K A E L5 9 0 By the early 1980s, costs to provide these health care services reached epic proportions; and the financial ability of employers to cover these costs was being stretched to breaking point. In addition, new government health care regula- tions had been enacted that have had far-reaching effects on this US industry. The most dramatic change came with the inauguration of a prospective pay- ment system. By 1984, reimbursement shifted to a prospective system under which health care providers were paid preset fees for services rendered to patients. The procedural terminology codes that were initiated at that time designated the maximum number of billed minutes allowable for the type of procedure (ser- vice) rendered for each diagnosis. A diagnosis was identified by the International Classification of Diseases, Ninth Revision, Clinical Modification, otherwise known as ICD-9-CM. The two types of codes, procedural and diagnosis, had to logically
- 7. correlate or reimbursement was rejected. Put simply, regardless of which third-party payor insured a patient for health care, the bill for an office visit was determined by the number of minutes that the regulation allowed for the visit. This was dictated by the diagnosis of the primary problem that brought the patient into the office and the justifiable procedures used to treat it. These cost-cutting measures initiated through the government- mandated pro- spective payment regulation added to physicians’ overhead costs because more paperwork was needed to submit claims and collect fees. In addition, the length of time increased between billing and actual reimbursement, causing cash flow problems for medical practices unable to make the procedural changes needed to adjust. This new system had the effect of reducing income for most physicians, because the fees set by the regulation were usually lower than those physicians had previously charged. Almost all other operating costs of office practice increased. These included utilities, maintenance, and insurance premiums for office liability coverage, workers’ compen- sation, and malpractice coverage (for which costs tripled in the late 1980s and early 1990s). This changed the method by which government insurance reimbursement was provided for health care disbursed to individuals covered
- 8. under the Medicare and Medicaid programs. Private insurors quickly adopted the system, and health care as an industry moved into a more competitive mode of doing business. The industry profile differed markedly from that of only a decade earlier. Hos- pitals became complex blends of for-profit and not-for-profit divisions, joint ven- tures, and partnerships. In addition, health care provided by individual physician practitioners had undergone change. These professionals were forced to take a new look at just who their patients were and what was the most feasible, competitively justifiable, and ethical mode of providing and dispensing care to them. For the first time in his life, Dr. Mickael read about physicians who were bank- rupt. In actuality, Dr. Charles, who shared office space with him, was having a financial struggle and was close to declaring bankruptcy. January 6, 1994 The last patient had just left, and Dr. Lou Mickael (“Dr. Lou”) sat in his office thinking about the day’s events. He had been delayed getting into work because both08.indd 590both08.indd 590 11/11/08 11:46:25 AM11/11/08 11:46:25 AM
- 9. 5 9 1 a patient telephoned him at home to talk about a problem with his son. When he arrived at the office and before there was time to see any of the patients waiting for him, the hospital called to tell him that an elderly patient, Mr. Spence, admitted through the emergency room last night had taken a turn for the worse. “My days in the office usually start with some sort of crisis,” he thought. “In addition to that, the national regulations for physician and hospital care reim- bursement are forcing me to spend more and more time dealing with regulatory issues. The result of all this is that I’m not spending enough time with my patients. Although I could retire tomorrow and not have to worry financially, that’s not an alternative for me right now. Is it possible to change the way this practice is organized, or should I change the type of practice I’m in?” Practice Background When Dr. Lou began medical practice the northeastern city’s population was approx- imately 130,000 people, most of whom were blue-collar workers with diverse ethnic backgrounds. By 1994, suburban development surrounded the city, more than doubling the population base. A large representation of service industries
- 10. were added, along with an extensive number of upper and middle managers and administrators typically employed by such industries. Location Dr. Lou kept the same office over the years. It was less than one-half mile from the main thoroughfare and located in a neighborhood of single- family dwell- ings. The building, constructed specifically for the purpose of providing space for physicians’ offices, was situated across the street from City General, the hospital where Dr. Lou continued to maintain staff privileges. Three physicians (including Dr. Lou) formed a corporation to purchase the building, and each doctor paid that corporation a monthly rental fee, which was based primarily on square footage occupied, with an adjustment for shared facilities such as a waiting room and rest rooms. Office Layout One of the physicians, Dr. Salis, was an orthopedic surgeon who occupied the entire top floor of the building. Dr. Lou and the other physician, Dr. Charles, were housed on the first floor. Total office space for each (a small reception area, two examining rooms, and private office) encompassed a 15' × 75' area (see Exhibit 8/1). The basement was reserved for storage and maintenance equipment.
- 11. The reception area and each of the other rooms that made up the office space opened on to a hallway that Dr. Lou shared with Dr. Charles. The two physicians and their respective staff members had a good rapport; and because the reception desks opened across from each other, each staff was able to provide support for the other by answering the phone or giving general informa- tion to patients when the need arose. P R A C T I C E B A C K G R O U N D both08.indd 591both08.indd 591 11/11/08 11:46:25 AM11/11/08 11:46:25 AM C A S E 8 : D R . L O U I S M I C K A E L5 9 2 The large, common waiting room was used by both physicians. After report- ing to their own doctor’s reception area, patients were seated in this room, then paged for their appointment via loudspeaker. Dr. Charles was in his mid-forties and in general practice as well. His patients ranged in age from 18 to their mid-eighties, and his office was open from 10:00 A.M. until 7:30 P.M. on Mondays and Thursdays, and from 9:30 A.M. until 4:30 P.M. on Tuesdays and Fridays; no office hours were scheduled on Wednesday. He and Dr. Lou were familiar with each other’s patient base, and
- 12. each covered the other’s practice when necessary. Staff and Organizational Structure Dr. Lou’s staff included one part-time bookkeeper (who doubled as office manager) and two part-time assistants. The assistants’ and bookkeeper’s time during office hours was organized in such a way that one individual was always at the recep- tion desk and another was “floating,” taking care of records, helping as needed in the examining rooms, and providing office support functions. There were never more than two staff people on duty at one time, and the assistants’ job descrip- tions overlapped considerably (see Exhibit 8/2 for job descriptions). Each staff member could handle phone calls, schedule appointments, and usher patients to the examining rooms for their appointments. Although Dr. Lou was “only a phone call away” from patients on a 24-hour basis, patient visits were scheduled only four days a week. On two of these days (Monday and Thursday) hours were from 9:00 A.M. to 5:00 P.M. The other two were “long days” (Tuesday and Friday), when office hours officially were extended to 7:00 P.M. in the evening, but often ran much later. Front Desk Treatment
- 13. Room 1 Treatment Room 2 Private Office Dr. Charles’ Office Space Front Door Common Waiting Room 75' 15' Exhibit 8/1: Shared Office Space of Dr. Mickael and Dr. Charles both08.indd 592both08.indd 592 11/11/08 11:46:26 AM11/11/08 11:46:26 AM 5 9 3 The fifth weekday (Wednesday) was reserved for meetings, which were an important part of Dr. Lou’s professional responsibilities because he was a mem- ber of several hospital committees. He was one of two
- 14. physicians residing on the ten-member board of the hospital, and this, along with other committee responsibilities, often demanded attendance at a variety of scheduled sessions from 7:00 A.M. until late afternoon on “meetings” day. Wednesday was used by the staff to process patient insurance forms, enter patient data into their charts and accounts receivables, and prepare bills for processing. When paperwork began to build after the PPS regulations came into effect in the 1980s, patients had many problems dealing with the forms that were required for reimbursement of services received in a physician’s office. It was the option of physicians whether to “accept assignment” (the standard fee designated by an insurance payor for a particular health care service provided in a medical office). A physician who chose to not accept assignment must bill patients for health care services according to a fee schedule (“a usual charge” industry profile) that was preset by Medicare for Medicare patients. Most other insur- ances followed the same profile. Dr. Lou agreed to accept the standard fee, but the patient had to pay 20 percent of that fee, so the billing process became quite complicated. In 1988, Dr. Lou decided that he needed to computerize his patient informa- tion base to provide support for the billing function. He
- 15. investigated the possib- ility of using an off-site billing service, but it lacked the flexibility needed to deal with regulatory changes in patient insurance reporting that occurred with greater Exhibit 8/2: Job Descriptions for Dr. Mickael’s Office Staff Job Description: Bookkeeper/Office Manager In addition to responsibility for bookkeeping functions, ordering supplies, and reconciling the orders with supplies received, this person knows how to run the reception area, pull the file charts, and usher patients to treatment rooms. In addition, she can handle phone calls, schedule appointments, and enter office charges into patient accounts using the computer. Job Description: Assistant 1 The main responsibility of this position is insurance billing. Additional duties include running the reception area, pulling and filing charts, ushering patients to treatment rooms, answering the phone, scheduling appointments, entering office charges into patient accounts, and placing supplies received into appropriate storage areas. Job Description: Assistant 2 This is primarily a receptionist position. The duties include running the reception area, pulling and filing charts, ushering patients to treatment rooms, answering the phone, scheduling appointments, entering office charges into patient accounts, and placing
- 16. supplies received into appropriate storage areas. S T A F F A N D O R G A N I Z AT I O N A L S T R U C T U R E both08.indd 593both08.indd 593 11/11/08 11:46:29 AM11/11/08 11:46:29 AM C A S E 8 : D R . L O U I S M I C K A E L5 9 4 and greater frequency. Dr. Charles was asked if he wished to share expenses and develop a networked computer system. But the offer was declined; he preferred to take care of his own billing manually. An information systems consultant was hired to investigate the computer hardware and software systems available at that time, make recommendations for programs specifically developed for a practice of this type, and oversee installation of the final choice. After initial setup and staff training, the con- sultant came to the office only on an “as needed” basis, mostly to update the diagnostic and procedure codes for insurance billing. Computerization was an important addition to the record- keeping process, and the system helped increase the account collection rate. However, at times prob-
- 17. lems would arise when the regulations changed and third-party payors (insurance companies) consequently adjusted procedure or diagnosis codes. For example, there was often some lag time between such decisions and receipt of the informa- tion needed to update the computer program. Fortunately, the software chosen remained technologically sound, codes were easily adjusted, and vendor support was very good. Although the new system helped to adjust the account collection rate, fitting this equipment into the cramped quarters of current office space was a problem. To keep the computer paper and other supplies out of the way, Dr. Lou and his staff had to constantly move the heavy boxes containing this stock to and from the basement storage area. January 8, 1994 (Morning) On Dr. Lou’s way in that day, the bookkeeper told him that something needed to be done about accounts receivable. Lag time between billing and reimburse- ment was again getting out of hand, and cash flow was becoming a problem (see Exhibits 8/3 through 8/6 for financial information concerning the practice). Cash flow had not been a problem prior to PPS, when billing for the health care provided by Dr. Lou was simpler, and payment was usually
- 18. retrospectively reimbursed through third-party payors. However, as the regulatory agencies continued to refine the codes for reporting procedures, more and more pressure was being placed on physicians to use additional or extended codes in reporting the condition of a patient. Speed of reimbursement was a function of the accur- acy with which codes were recorded and subsequently reported to Medicare and other insurance companies. In part, that was determined by a physician’s ability to keep current with code changes required to report illness diagnoses and office procedures. Cathy, the receptionist, had a list of patients who wanted Dr. Lou to call as soon as he came in. She also wanted to know if he could squeeze in time around lunch hour to look at her husband’s arm; she believed he had a serious infec- tion resulting from a work-related accident. The wound looked pretty nasty this morning, and Cathy thought maybe it should not wait until the first available appointment at 7:00 P.M. both08.indd 594both08.indd 594 11/11/08 11:46:29 AM11/11/08 11:46:29 AM 5 9 5
- 19. Exhibit 8/3: Trial Balance at December 31 1991 1992 1993 Debits Cash $15,994 $9,564 $8,666 Petty cash 50 100 100 Accounts receivable 19,081 25,054 28,509 Medical equipment 11,722 11,722 11,722 Furniture and fixtures 3,925 3,925 3,361 Salaries 117,455 124,608 132,325 Professional dues and licenses 1,925 1,873 1,816 Miscellaneous professional expenses 1,228 2,246 3,232 Drugs and medical supplies 2,550 1,631 2,176 Laboratory fees 2,629 524 1,801 Meetings and seminars 2,543 838 3,880 Legal and professional fees 5,525 2,057 5,400 Rent 16,026 16,151 18,932 Office supplies 4,475 3,262 4,989 Publications 1,390 406 401 Telephone 1,531 1,451 2,400 Insurance 8,876 9,629 11,760 Repairs and maintenance 3,547 4,240 5,352 Auto expense 1,009 1,487 3,932 Payroll taxes 3,107 2,998 3,780 Computer expenses 846 938 1,905 Bank charges 438 455 479 $225,872 $225,159 $256,918 Credits Professional fees $172,281 $172,472 $204,700 Interest income 992 456 210 Capital 46,122 43,137 40,117 Accumulated depreciation (furniture and fixtures) 1,692 2,151 2,796
- 20. Accumulated depreciation (medical equipment) 4,785 6,943 9,095 $225,872 $225,159 $256,918 Exhibit 8/4: Gross Revenue and Accounts Receivable December 31 1979 1986 Gross revenue $116,951 $137,126 Accounts receivable 15,684 32,137 J A N U A R Y 8 , 1 9 9 4 ( M O R N I N G ) both08.indd 595both08.indd 595 11/11/08 11:46:29 AM11/11/08 11:46:29 AM C A S E 8 : D R . L O U I S M I C K A E L5 9 6 “I’m just starting to see my patients, and I’ve already done a half-day’s work,” Dr. Lou thought when he buzzed his assistant to bring in the first patient. He was 45 minutes late. Patient Profile When Dr. Lou walked into Treatment Room 1 to see the first patient of the day, Doris Cantell, he was thinking about how his practice had grown over the years. His practice maintained between 800 and 900 patients in active files. In com-
- 21. parison to other solo practitioners in the area, this would be considered a fairly large patient base. “Well, how are you feeling today?” he asked the matronly woman. Doris and her husband, like many of his patients, were personal friends. In the beginning years of practice, Dr. Lou’s patients had been primarily younger people with an average age in the mid-thirties; their average income was approximately $15,000. Their families and careers were just beginning, and it was not unusual to spend all night with a new mother waiting to deliver a Exhibit 8/5: Statements of Income for the Years Ended December 31 1991 1992 1993 Operating Revenues Professional fees $172,281 $172,472 $204,700 Interest income 992 456 210 Total revenues 173,273 172,928 204,910 Operating Expenses Salaries (Dr. Mickael, Staff) 117,455 124,608 132,325 Professional dues and licenses 1,925 1,873 1,816 Miscellaneous professional expenses 1,228 2,246 3,232 Drugs and medical supplies 2,550 1,631 2,176 Laboratory fees 2,629 524 1,801
- 22. Meetings and seminars 2,543 838 3,880 Legal and professional fees 5,525 2,057 5,400 Rent 16,026 16,151 18,932 Office supplies 4,475 3,262 4,989 Publications 1,390 406 401 Telephone 1,531 1,451 2,400 Insurance 8,876 9,629 11,760 Repairs and maintenance 3,547 4,240 5,352 Auto expense 1,009 1,487 3,932 Payroll taxes 3,107 2,998 3,780 Computer expenses 846 938 1,905 Bank charges 438 455 479 Total operating expenses 175,100 174,794 204,560 Net Income (Loss) ($1,827) ($1,866) $350 both08.indd 596both08.indd 596 11/11/08 11:46:30 AM11/11/08 11:46:30 AM 5 9 7 baby. Although often dead tired, he enjoyed the closeness of the professional rela- tionships he had with his patients. He believed that much of his success as a physician came from “going that extra mile” with them. Many things had changed. Today all pregnancies were referred to specialists in the obstetrics field. His patients ranged in age from 3 to 97, with an average of 58 years; their median income was $25,000. Most were blue- collar workers or
- 23. recently retired, and their health care needs were quite diverse. Approximately 60 percent of Dr. Lou’s patients were subsidized by Medicare insurance, and most of the retired patients carried supplemental insurance with other third-party payors. Three types of third-party payors were involved in Dr. Lou’s practice: (1) private insurance companies, such as Blue Cross and Blue Shield; (2) government insurance (Medicare and Medicaid); and (3) preferred provider organizations. Preferred provider organizations and health maintenance organizations were forms of group insurance that emerged in response to the need to cut the costs of providing health care to patients, which resulted in the prospective payment system. Both types of organizations developed a list of physicians who would Exhibit 8/6: Balance Sheets at December 31 1991 1992 1993 Assets Capital equipment Medical equipment $11,722 $11,722 $11,722 Furniture and fixtures 3,925 3,925 3,361 Less-accumulated depreciation (6,477) (9,094) (11,891) Total capital equipment 9,170 6,553 3,192 Current assets
- 24. Cash 15,994 9,564 8,666 Petty cash 50 100 100 Accounts receivable 19,081 25,054 28,509 Total current assets 35,125 34,718 37,277 Total assets $44,295 $41,271 $40,467 Liabilities Current liabilities Income taxes payable ($639) ($653) $122 Dividends payable 1,158 1,154 1,154 Total current liabilities 519 501 1,276 New income (1,188) (1,213) 228 Less dividends 1,158 1,154 1,154 Retained earnings (2,346) (2,367) (926) Capital 46,122 43,137 40,117 Total owner’s equity 43,776 40,770 39,191 Total liabilities and owner’s equity $44,295 $41,271 $40,467 PAT I E N T P R O F I L E both08.indd 597both08.indd 597 11/11/08 11:46:30 AM11/11/08 11:46:30 AM C A S E 8 : D R . L O U I S M I C K A E L5 9 8 accept their policies and fee schedules; using the list, subscribers chose the doctor from whom they preferred to obtain health care services.
- 25. Contrary to reimbursement policies of most other major medical third-party payors, PPOs and HMOs covered the cost of office visits, and the patient might not be responsible for any percentage of that cost. Although the physician had to accept a fee schedule determined by the outside organization, there was an advantage to working with these agencies. A physician might be on the list of more than one organization, and a practice could maintain or expand its patient base through the exposure gained from being listed as a health service provider for such organizations. Those patients who were working usually had coverage through work bene- fits. Some were now members of a PPO. Dr. Lou was on the provider list of the Northeast Health Care PPO; only a few of his patients were enrolled in the government welfare program. “How’s your daughter doing in college?” Dr. Lou asked. He had a strong rap- port with the majority of his patients, many of whom continued to travel to his office for medical needs even after they moved out of the immediate area. “Are you heading south again this winter, and are you maintaining your ‘snowbird’ relationship with Dr. Jackson?” It was not unusual for patients to call from as far away as
- 26. Florida and Arizona during the winter months to request his opinion about a medical problem, and Doris had called last year to ask him to recommend a physician near their winter home in the South. Because of this personal attention, once patients initiated health care with him, they tended to continue. Dr. Lou had lost very few patients to other physicians in the area since he began to practice medicine. The satisfac- tion experienced by his patients provided the only marketing function carried out for the practice. Any new patients (other than professional referrals) were drawn to the office through word-of-mouth advertising. Dr. Lou: Profile of the Physician Dr. Lou had grown older with many of his patients. His practice spanned more than three generations; a lot of families had been with him since he opened his doors in 1961. Caring for these people, many of whom had become personal friends, was very important to him. However, as the character of the health care industry was changing, Dr. Lou was beginning to feel that he now spent entirely too much time dealing with the “system” rather than taking care of patients. Eighty-year-old Mr. Spence was a good example. Three weeks before, he was discharged from the hospital after having a pacemaker implanted. He had been
- 27. living at home with his wife, and although she was wheelchair bound, they managed to maintain some semblance of independence with the assistance of part-time care. Lately, however, the man had become more and more confused. The other night he wandered into the yard, fell, and broke his hip. His reentry to the hospital so soon meant that a great deal of paperwork would be needed to justify this second hospital admission. In addition, Dr. Lou expected to receive both08.indd 598both08.indd 598 11/11/08 11:46:30 AM11/11/08 11:46:30 AM 5 9 9 calls from their children asking for information to help them determine the best alternatives for the care of both parents from now on. He had never charged a fee for such consultation, considering this to be an extension of the care he norm- ally provided. “Things are really different now,” he thought. “Under this new system I don’t have the flexibility I need to determine how much time I should spend with a patient. The regulations are forcing me to deal with business issues for which I have no background, and these concerns for costs and time efficiency are very
- 28. frustrating. Medical school trained me in the art and science of treating patients, and in that respect I really feel I do a good job, but no training was provided to prepare me to deal with the business part of a health care practice. I wonder if it’s possible to maintain my standards for quality care and still keep on practic- ing medicine.” Local Environment The actual number of city residents had not changed appreciably since the early 1960s, although suburban areas had grown considerably. In the mid-1970s, a four-lane expressway, originally targeted for construction only one mile from the center of the downtown area, was put in place about eight miles farther away. Within five years, most of the stores followed the direction of that main highway artery and moved to a large mall situated about five miles from the original center of the city. Many of the former downtown shops then became empty. Government offices, banking and investment firms, insurance and real estate offices, and a university occupied some of this vacated space; it was used for quite different (primarily service-oriented) business activities. Numerous residential apartments devoted to housing for the elderly and low- income families were built near the original, downtown shopping area. Several
- 29. large office buildings (where much space was available for rent) and offices for a number of human services agencies relocated nearby. As he headed across the street to lunch in the hospital dining room, Dr. Lou was again thinking about how things had changed. At first, he had been one of a few physicians in this area. Within the past ten years, however, many new physicians had moved in. Competition Two large (500-bed) hospitals within easy access of the downtown area had been in operation for over 40 years. One was located immediately within the city lim- its on the north side of the city; the other was also just inside city limits on the opposite (south) side. They were approximately three miles apart and competed for a market share with City General, a 100-bed facility. This smaller hospital was only two blocks from the old business district; it was the only area hospital where Dr. Lou maintained staff privileges. Exhibit 8/7 contains a map showing the loca- tion of the hospitals and Dr. Lou’s office. C O M P E T I T I O N both08.indd 599both08.indd 599 11/11/08 11:46:31 AM11/11/08 11:46:31 AM
- 30. C A S E 8 : D R . L O U I S M I C K A E L6 0 0 The two large hospitals had begun to actively compete for staff physicians (physicians in private practice who paid fees to a hospital for the privilege of bringing their patients there for treatment). In addition, these two health care institutions offered start-up help for newly certified physicians by providing low-cost office space and ensuring financial support for a certain period of time while they worked through the first months of practice. City General recently began subsidizing physicians coming into the area by providing them with offices inside the hospital. Most of these physicians worked in specialty fields that had a strong market demand, and the hospital gave them a salary and special considerations, such as low rent for the first months of practice, to entice them to stay in the area. These doctors served as consultants to hospital patients admitted by other staff physicians and could influence the length of time a patient remained in the hos- pital. This was an extremely important issue for the hospital, because under the new regulations a long length of stay could be costly to the facility. All third-party insurors reimbursed only a fixed amount to the hospital for patient care; the pay- ment received was based on the diagnosis under which a patient
- 31. was admitted. Should a patient develop complications, a specialist could validate the extension of reimbursable time to be added to the length of stay for that patient. In the past few years, many services to patients provided by all these hospitals changed to care provided on an outpatient basis. Advancements in technology made it possible to complete in one day a number of services, including tests and some surgical procedures, which formerly required admission into the hospital and an overnight stay. Many such procedures could also be done by physicians in their offices, but insurance reimbursement was faster and easier if a patient had them done in a hospital. As an example of the degree of change involved, W. P ost R d. Airport W. Ridge Rd. W 31 St ar r R d.
- 32. Be ac h PE N N R R Hospital NYC RR E. P ost Rd. E. Ridge Rd. W ar re n R d . HospitalTownhall Rd.
- 33. Dr. Mickael Pe nt ar R d. City General E 31 Exhibit 8/ 7: Map of the Hospitals and Dr. Mickael’s Medical Office both08.indd 600both08.indd 600 11/11/08 11:46:31 AM11/11/08 11:46:31 AM 6 0 1 in the mid-1980s, outpatient gross revenue was only 18 percent of total gross revenue for City General. In 1992 this figure was projected to be approximately 30 percent. January 8, 1994 (Lunchtime) “May I join you?” Dr. Lou looked up from his lunch to see Jane Duncan, City
- 34. General’s hos- pital administrator, standing across the table. “I’d like to talk with you about something.” Dr. Lou thought he knew what this was about. The hospital had been recruit- ing additional staff physicians (doctors who owned private practices in and around the city). A number of these individuals held family practice certification, a prerequisite for staff privileges in many hospitals. The recruitment program offered financial assistance to physicians who were family practice specialists wish- ing to move into the area, and also subsidized placement of younger physicians who had recently completed their residencies. In contrast to physicians designated as general practitioners, who had not received training beyond that received through medical school and a residency, “family practitioners” received additional training and passed state board exams written to specifically certify a physician in that field. Last week after a hospital staff meeting, Duncan had caught him in the hall and wanted to know if Dr. Lou had thought about his retirement plans. “It’s really not too soon,” she had said. Dr. Lou knew that one of the methods used to bring in “new blood” was to provide financial backing to a physician wishing to ease out
- 35. of practice, helping pay the salary of a partner (usually one with family practice certification) until the older physician retired. “She wants to talk to me again about retirement and taking on a partner,” he thought. “But I’m only in my late fifties. And I’m not ready to go to pasture yet! Besides, there’s really no room to install a partner in my office.” January 8, 1994 (Afternoon) After lunch Dr. Lou ran back to the office to take a look at Cathy’s husband’s arm before regular office hours started. This was a work-related case. As he treated the patient, he began thinking about industrial medicine as an alternative to full-time office practice. Right then the prospect seemed quite appealing. He had invest- igated the idea enough to know that there were only a few schools that provided this kind of training but one was within driving distance (Exhibit 8/8 contains information on industrial medicine). As health costs rose over the past decade, manufacturing organizations began to feel the cost pinch of providing health care insurance to employees. Some larger companies in the area began to recognize the cost benefit of maintaining a pri- vate physician on staff who was trained in the treatment of health care needs for
- 36. J A N U A R Y 8 , 1 9 9 4 ( A F T E R N O O N ) both08.indd 601both08.indd 601 11/11/08 11:46:32 AM11/11/08 11:46:32 AM C A S E 8 : D R . L O U I S M I C K A E L6 0 2 industrial workers. Dr. Lou had been considering going back for postgraduate training in industrial medicine, and while wrapping the man’s arm, he began to think about working for a large corporation. “Work like that could have a lot of benefits; it would give me a chance to do something a little different, at least part time for now,” he thought. “The income was almost comparable to what I net for the same time in the office, and some days I might even get home before 9:00 P.M.!” End of the Day As he was putting on his coat and getting ready to leave, Dr. Charles, the physi- cian from across the hall, phoned to ask if Dr. Lou might be interested in buying him out. “I think you could use the space,” he said, “and my practice is going down the tubes. I can’t seem to get an upper hand with the finances. I’ve had to borrow every month to maintain the cash flow needed to pay my bills because patients can’t keep up with theirs. City General has offered me
- 37. a staff position, and I’m seriously considering it. I thought I’d give you first chance.” After some minutes of other “office talk,” Dr. Charles said good night. “If I wanted to take on a new partner, that could work out well,” thought Dr. Lou. “It might be interesting to check into this. I wonder what his asking price would be? It could not be too much more than the value of my practice; although his patients are a bit younger and some of his equipment is a little newer. The Exhibit 8/8: Industrial Medicine as a New Career for Dr. Mickael “Industrial Medicine” is an emerging physician specialty. Training in this new field entails postgraduate work and board certification. As yet, only a few schools provide such training. One is located in Cincinnati, Ohio, which is geographically close enough to be feasible for Dr. Mickael. The time spent in actual attendance amounts to one two-week training period beginning in June of the year in which a physician is accepted for the training. Two additional training periods are each one week in duration: these take place in the months of October and March. After this, the physician was expected to individually study for and take the board certification exams, which were given only once per year; the exams were comprehensive and extended over a two-day period. Training Program Costs: Industrial Medicine
- 38. University Residency: Three, on-site class sessions $4,000.00 Per night cost for room 47.87 Books and supplies (total) 580.53 Transportation, Air: Three, round-trip fares $1,650.00 Transportation, Ground: Car rental, per week with unlimited mileage $125.45 both08.indd 602both08.indd 602 11/11/08 11:46:32 AM11/11/08 11:46:32 AM 6 0 3 initial hospital proposal to buy me out indicated that my practice was worth about $175,000. So that means I should be able to negotiate with Dr. Charles for a little less than $200,000.” It was 9:30 P.M. when Dr. Lou finally left the office, and he still had hospital rounds to make. “This is another situation caused by these insurance regula- tions,” he thought. “I feel as though I’m continuously updating patients’ hospital records throughout the day, and more of my patients require hospitalization more often than they did when they were younger. All things being equal, I’m
- 39. earning considerably less for doing the same things I did a decade ago, and in addition the paperwork has increased exponentially. There has to be a better way for me to deal with this business of practicing medicine.” E N D O F T H E D AY both08.indd 603both08.indd 603 11/11/08 11:46:33 AM11/11/08 11:46:33 AM STRATEGIC MANAGEMENT OF HEALTH CARE ORGANIZATIONS 7TH EDITION 1 Chapter 4 Internal Environmental Analysis and Competitive Advantage
- 40. 2 Chapter 4 Learning Objectives Understand the role of internal environmental analysis in identifying the basis for sustained competitive advantage. 3 Chapter 4 Learning Objectives Understand the role of internal environmental analysis in identifying the basis for sustained competitive advantage. Describe the organizational value chain, including the components of the service delivery and support activities. 4 Chapter 4 Learning Objectives Understand the role of internal environmental analysis in identifying the basis for sustained competitive advantage.
- 41. Describe the organizational value chain, including the components of the service delivery and support activities. Understand the ways in which value can be created at various places in the organization with the aid of the value chain. 5 Chapter 4 Learning Objectives Use the value chain to identify organizational strengths and weaknesses. 6 Chapter 4 Learning Objectives Use the value chain to identify organizational strengths and weaknesses. Determine the competitive relevance of each strength and weakness with the aid of a series of carefully formulated questions. 7
- 42. Chapter 4 Learning Objectives Use the value chain to identify organizational strengths and weaknesses. Determine the competitive relevance of each strength and weakness with the aid of a series of carefully formulated questions. Describe how competitively relevant strengths and weaknesses can be used to suggest strategic actions. 8 Develop a Strategy Strategy of the Organization External Environment Internal Environment Directional Strategies, Leadership Should Do
- 43. Can Do Wants To Do 9 The Strategic Planning Process Strategic Planning Situation Analysis Strategy Formulation Planning the Implementation External Analysis Internal Analysis Directional Strategies Service Delivery Strategies Support Strategies Action Plans Directional Strategies Adaptive Strategies
- 44. Market Entry Strategies Competitive Strategies 10 Internal Analysis Whereas external analysis asked “what should we do?”, internal analysis addresses “what can we do?” 11 Internal Analysis Whereas external analysis asked “what should we do?”, internal analysis addresses “what can we do?” Identify strengths (competitive advantages) and weaknesses (competitive disadvantages) 12
- 45. The Health Care Value Chain Pre-Service Market Research Target Market Services Offered/ Banding Pricing Distribution/Logistics Promotion Point-of-Service Clinical Operations Quality Process Innovation Marketing Patient Satisfaction After-Service Follow-up Clinical Marketing Billing Follow-on Clinical Marketing Service Delivery Add Value 13 The Health Care Value Chain Organizational Culture
- 46. Shared Assumptions Shared Values Behavioral Norms Organizational Structure Function Division Matrix Strategic Resources Financial Human Information Technology Support Activities Add Value 14 The Health Care Value Chain Pre-Service Market Research Target Market Services Offered/ Banding Pricing Distribution/Logistics Promotion Point-of-Service Clinical Operations Quality Process Innovation Marketing Patient Satisfaction After-Service Follow-up Clinical Marketing Billing Follow-on
- 47. Clinical Marketing Organizational Culture Shared Assumptions Shared Values Behavioral Norms Organizational Structure Function Division Matrix Strategic Resources Financial Human Information Technology Support Activities Service Delivery Add Value Add Value 15 Description of Value Chain Components Service DeliveryValue Chain ComponentDescriptionService DeliveryThe activities in the value chain that are directly involved in ensuring access to, provision of, and follow-up for health servicesPre-Service Market/Marketing ResearchDetermine the services that create value prior to the actual delivery of health services, determine appropriate target market Target MarketThe process of identifying recognizable groups (segments) that make up the market and selecting appropriate groups upon which to focus Services Offered/BrandingInformation dissemination to present to prospective patients and other stakeholders regarding the range and location of available services PricingCharge schedule for available services Distribution/LogisticsActivities and systems that facilitate patient/customer entry into the service delivery system, including appointments and registration
- 48. PromotionActivities that ensure all the elements needed to deliver health services are available at the appropriate place at the appropriate time 16 Description of Value Chain Components Service DeliveryValue Chain ComponentDescriptionPoint-of- Service Clinical Operations Quality Process InnovationThose service delivery activities that create value at the point where services are actually delivered The activities that convert the human and non-human resources into health services Actual provision of health services to the individual patient Marketing Patient SatisfactionActivities and groups of activities that are designed specifically to improve the quality and quantity of health services Activities to offer new products, seek new customers, provide better services delivery, and cause services to be perceived as higher value 17 Description of Value Chain Components Service DeliveryValue Chain ComponentDescriptionAfter-
- 49. Service Follow-up Clinical MarketingActivities that create value after the patient has received the health services Activities designed to determine the effectiveness of or the patient’s satisfaction with health services received BillingActivities that assist in determining what other services need to be delivered Value creating activities that ensure more understandable and efficient billing procedures Follow-on Clinical MarketingActivities that facilitate entry into another value chain (from hospital to home care, etc.) 18 Description of Value Chain Components Support ActivitiesValue Chain ComponentDescriptionSupport ActivitiesThe activities in the value chain that are designed to aid in the efficient and effective delivery of health servicesOrganizational Culture Shared Assumptions Shared Values Behavioral NormsThe overarching environment within which the health services organization operates The assumptions employees and others share in the organization regarding all aspects of service delivery (e.g., needs of patients, goals of the organization) The guiding principles of the organization and its employees The understandings people in the organization have regarding excellence, risk taking, etc. Understandings about behavior in the organization that can create value for patients
- 50. 19 Exhibit 4-2: Description of Value Chain Components Support ActivitiesValue Chain ComponentDescriptionOrganizational Structure Function Division MatrixThose aspects of organization structure that are capable of creating value for customers/patients Structure based on process or activities used by employee (e.g., surgery, finance, human resources) Major units operate relatively autonomously subject to overarching policy guidelines (e.g., hospital division; outpatient division; northwest division) Two-dimensional structure where more than a single authority structure operates simultaneously (e.g., interdisciplinary team with representatives from medicine, nursing, administration) 20 Exhibit 4-2: Description of Value Chain Components Support ActivitiesValue Chain ComponentDescriptionStrategic Resources Financial Human Information
- 51. TechnologyValue-creating financial, human, information resources, and technology necessary for the delivery of health services Financial resources required to provide the facilities, equipment, and specialized competencies demanded by the delivery of health services Individuals with the specialized skills and commitment to deliver health services Hardware, software, and information processing systems needed to support the delivery of health services The facilities and equipment required to provide health services 21 Identifying Current and Potential Competitive Advantage Resources Resource-based View: Valuable, expensive or difficult-to-copy resources Non-human Factors Competencies Knowledge and skill based Human Factors Socially complex and require large numbers of people engaged in coordinated activities Capabilities Organization’s ability to deploy resources and competencies to produce its capability
- 52. 22 Strategic Thinking Map – Step 1 Identify Strengths and Weaknesses Pre-Service Point-of-Service After-Service Culture Structure Strategic Resources Service Delivery Strengths & Weaknesses Support Activities Strengths & Weaknesses 23 Strategic Thinking Map – Step 2 Evaluate Competitive Relevance of Strengths and Weaknesses Value Rare
- 53. Imitable Sustainable Competitively Relevant Strengths Competitively Relevant Weaknesses 24 Strategic Thinking Map – Step 3 Focus on Competitive Strengths and Competitive Weaknesses Competitive Advantages Competitive Disadvantages 25 Some Sources of Competitive Advantage Strong financial holdings or backing Desirable location State-of-the-art facilities or equipment Difficult to obtain information Intellectual property Especially when protected by patents Reputation Positive image
- 54. Name recognition Goodwill Strong leadership/competent management Effective communication A positive organizational culture Tangible Intangible 26 Strategic Thinking What strengths can be considered competitive advantages? Is the Value of the Strength High or Low?Is the Strength Rare?Is the Strength Easy or Difficult to Imitate?Can the Strength be Sustained?High/LowYes/NoEasy/DifficultYes/No 27 Is the Value of the Strength High or Low? (High/Low?)Is the Strength Rare? (Yes/No)Is the Strength Easy or Difficult to Imitate? (Easy/Difficult)Can the Strength Be Sustained? (Yes/No)ImplicationsHNEYNo competitive advantage. Most competitors have the strength and those that do not can develop it easily and sustain it. Because the strength is widely possessed and can be sustained, it is likely that it already has become a minimum condition for long-term success.HNENNo competitive
- 55. advantage. Most competitors have the strength and it is easy to develop. However, the strength generally is not sustainable. If the organization is the only organization in the service area that cannot sustain the strength, it will become a short-term competitive disadvantage.HNDYNo competitive advantage. Many competitors possess the strength but it is difficult to develop, so care should be taken to maintain this strength. Because the strength is widely possessed and can be sustained, it is likely that it already has become a minimum condition for long-term success. Strategic Thinking Map of Competitive Advantages Relative to Strengths in General 28 Is the Value of the Strength High or Low? (High/Low?)Is the Strength Rare? (Yes/No)Is the Strength Easy or Difficult to Imitate? (Easy/Difficult)Can the Strength Be Sustained? (Yes/No)ImplicationsHNDNNo competitive advantage. Many competitors possess the strength but it is difficult to develop, and those who do possess it will not be able to sustain the strength. If the organization is the only organization that can not sustain the strength, it will become a long-term competitive disadvantage.HYEYShort-term competitive advantage. Because the strength is valuable and rare, competitors will do what is necessary to develop this easy-to-imitate strength. The organization should exploit this short-term advantage but should not base long-term strategies on this type of strength. Over time, this strength may become a minimum condition for long- term success.HYENShort-term advantage but not a source of long-term competitive advantage. The strength is easy to imitate
- 56. but cannot be sustained. The organization should not base long- term strategies on this type of strength but may obtain benefits of short-term advantage. Strategic Thinking Map of Competitive Advantages Relative to Strengths in General 29 Strategic Thinking Map of Competitive Advantages Relative to Strengths in GeneralIs the Value of the Strength High or Low? (High/Low?)Is the Strength Rare? (Yes/No)Is the Strength Easy or Difficult to Imitate? (Easy/Difficult)Can the Strength Be Sustained? (Yes/No)ImplicationsHYDYLong-term competitive advantage. This strength is rare in the service area, difficult to imitate by competitors, and can be sustained by the organization. If the value is very high, it may be worth “betting the organization” on this strength.HYDNShort-term competitive advantage but not a strength that can be sustained over the long run. Although rare and difficult to imitate, the strength cannot be sustained. This strength should be exploited for as long as possible. 30 Strategic Thinking What weaknesses can be considered competitive disadvantages?
- 57. Is the weakness of High or Low Value?Is the Weakness Common (Not Rare) Among Competitors?Is the Weakness Easy or Difficult to Fix?Can Competitors Sustain Their Advantage?High/LowYes/NoEasy/DifficultYes/No 31 Is the Weakness of High or Low Value? (High/Low?)Is the Weakness Common (Not Rare) Among Competitors? (Yes/No)Is the Weakness Easy or Difficult to Correct? (Easy/Difficult)Can Competitors Sustain Their Advantage? (Yes/No)ImplicationsHYEYNo competitive disadvantage. Although a weakness of the organization, most other competitors are also weak in this area. However, the weakness is easy to correct and competitors will likely work to correct the weakness. If the organization fails to correct the weakness, competitors could achieve a short-term competitive advantage. Over time, correcting this weakness is likely become a minimum condition for long-term success.HYENNo competitive disadvantage. Although a weakness of the organization, most other competitors are also weak in this area. However, the weakness is easy to correct. It is likely most competitors will work to correct the weakness and therefore no organization will be able to sustain their advantage. Strategic Thinking Map of Competitive Disadvantages Relative to Weakness
- 58. 32 Is the Weakness of High or Low Value? (High/Low?)Is the Weakness Common (Not Rare) Among Competitors? (Yes/No)Is the Weakness Easy or Difficult to Correct? (Easy/Difficult)Can Competitors Sustain Their Advantage? (Yes/No)ImplicationsHYDYNo competitive disadvantage. Although a weakness of the organization, most other competitors are also weak in this area and it is difficult to correct. However, this situation is dangerous and should be addressed to ensure competitors do not overcome this difficulty and correct it first. If competitors correct the weakness and continue to sustain their advantage the weakness could become a long-term competitive disadvantage.HYDNNo competitive disadvantage. Although a weakness of the organization, most other competitors are also a weak in this area and it is difficult to correct. It is likely this weakness is chronic among competitors in the service area as corrections in the weakness tend to erode over time. Strategic Thinking Map of Competitive Disadvantages Relative to Weakness 33 Is the Weakness of High or Low Value? (High/Low?)Is the Weakness Common (Not Rare) Among Competitors? (Yes/No)Is the Weakness Easy or Difficult to Correct? (Easy/Difficult)Can
- 59. Competitors Sustain Their Advantage? (Yes/No)ImplicationsHNEYShort-term competitive disadvantage. Most competitors are not weak in this area, however, the weakness is easy to correct. The organization should move quickly to correct this type of weakness because most other competitors are not weak in this area. Correcting this weakness is likely to become a minimum condition for long- term success.HNENShort-term competitive disadvantage. Competitors are not weak in this area, however, the weakness is easy to correct. The organization should move quickly to correct the weakness. It is likely all competitors will correct the weakness and therefore cannot sustain any advantage. Strategic Thinking Map of Competitive Disadvantages Relative to Weakness 34 Is the Weakness of High or Low Value? (High/Low?)Is the Weakness Common (Not Rare) Among Competitors? (Yes/No)Is the Weakness Easy or Difficult to Correct? (Easy/Difficult)Can Competitors Sustain Their Advantage? (Yes/No)ImplicationsHNDYSerious competitive disadvantage. The weakness is valuable, most competitors do not have it, it is difficult for the organization to correct, and competitors can sustain their advantage. If the weakness is of very high value, it may threaten the survival of the organization.HNDNShort-term competitive disadvantage. The weakness is valuable, most competitors do not have it, it is difficult for the organization to correct, however, competitors cannot sustain their advantage. Until this area becomes a weakness for most competitors in the
- 60. service area or the weakness corrected by the organization, it will continue to be a serious disadvantage. Strategic Thinking Map of Competitive Disadvantages Relative to Weakness 35 Questions for Evaluating the Internal Strategic Assumptions Have the strengths and weaknesses been correctly identified? Is there a clear basis on which to compete? Does the strategy exploit the strengths and avoid the major weaknesses of the organization? Are the competitive advantages related to the critical success factors in the service area? Have we protected our short- and long-term competitive advantages? Has the competition made strategic moves that have weakened our competitive advantages? Are we creating new competitive advantages? 36 Chapter 4 Conclusions After reading Chapter 4, you should be able to define the following terms:
- 61. Key TermsKey TermsAfter-ServiceService DeliveryCapabilityStrategic CapabilityCompetencyStrengthCompetitive AdvantageStretchCompetitive Relevant StrengthSupport ActivitiesCompetitive Relevant WeaknessSustained Competitive AdvantagePoint-of-ServiceValuePre-ServiceValue ChainResource-Based-ViewWeaknessResources 37 Assignment For ABC Long-Term Care Facility presented in the following slides, determine their competitive advantages and competitive disadvantages by completing the “Determining Competitive Advantage” and “Determining Competitive Disadvantage” Tables. In a separate table of your design, provide your conclusions and rationale for your competitive advantages and competitive disadvantages. 38 External Issues, Competitor Analysis and Critical Success FactorsExternal IssuesCompetitor Strengths and WeaknessesCritical Success FactorsMedicaid and Medicare reimbursement declining
- 62. Increasing penetration of managed care Capitation on the horizon CON laws disappearing Systems of care forming (Integrated systems) Changing medical technology Group practices growing Aging population Mergers and alliances increasing Some horizontal integration Changing social structure and family roles Established HMOs and PPOs Increasing CompetitionCompetitor 1 S – part of a viable system of care S – good information system S – patient base mostly HMO S – good image S – new facility W – new in the market W – poor location W – no internal continuum of care (nursing only) W – shortage of technical staff W – not currently efficient Competitor 2 S – low cost provider (efficient) S – strong management S – developing many alliances with other providers W – independent free standing facility W – patient base mostly Medicaid and Medicare W – shortage of technical staff High quality service/image Low Cost Provider Part of an Integrated System ABC Long-Term Care Facility
- 63. 39 Strengths and WeaknessesStrengthsWeaknessS – highly skilled and caring clinical staff S – recent financial turnaround S – facilities/campus remodeled S – good patient base (many referrals through informal alliances) S – good reputation/image S – excellent dietary department S – good location S – strong internal continuum of care (three levels of care) S – religious affiliationW – shortage of technical staff W – many problems with patient records W – lack of management depth W – many billing problems W – information system is out-of-date W – no strategic planning W – some supply/inventory problems W – aging facility W – narrowing financial margins W – independent facility W – some turnover of staff ABC Long-Term Care Facility
- 64. 40 Identifying Competitive Advantage Questions for Strengths: Can we build a competitive advantage based on this strength? If we have a strength that is valuable, rare in the service area, difficult to imitate and one that we can sustain, then this factor provides competitive advantage. Lack of real value, rareness in the industry or those strengths that are easy to imitate or that can not be sustained create less of an advantage. Questions for Weaknesses: Can our competitors build a competitive advantage against us because we are weak in this area? Weaknesses must be evaluated in terms of importance in the service area. Even though we are weak in an area, we must ask if these factors are important in creating competitive advantage for others. Thus, is the weakness valuable in the service area, is it rare among competitors, etc. If valuable but not rare, difficult to imitate and easy to sustain, we will have a significant competitive disadvantage. 41 Determining Competitive Advantage Possible Results for a Long-term Care OrganizationValue? High/LowRare? Yes/NoImitate? Hard/EasySustain? Yes/NoS – highly skilled and caring
- 65. clinical staffS – recent financial turnaroundS – facilities/campus remodeledS – good patient base (many referrals through informal alliances)S – good reputation/imageS – excellent dietary departmentS – good locationS – strong internal continuum of care (three levels of care)S – religious affiliation ABC Long-Term Care Facility 42 Determining Competitive DisadvantagePossible Results for a Long-term Care OrganizationValue? High/LowCommon? Yes/NoAble to Correct? Hard/EasyCompetitors can Sustain? Yes/NoW – shortage of technical staffW – problems with patient recordsW – lack of management depthW – many billing problemsW – information system out-of-dateW – no strategic planningW – supply/inventory problemsW – aging facilityW – narrowing financial marginsW – independent facility (not part of a continuum)W – some turnover of staff ABC Long-Term Care Facility 43
- 66. STRATEGIC MANAGEMENT OF HEALTH CARE ORGANIZATIONS 7TH EDITION 1 Service Area Competitor Analysis Chapter 3 2 Chapter 3 Learning Objectives Understand the importance of service area competitor analysis as well as its purpose.
- 67. 3 Chapter 3 Learning Objectives Understand the importance of service area competitor analysis as well as its purpose. Understand the relationship between general and health care environmental issue identification and analysis and service area competitor analysis. 4 Chapter 3 Learning Objectives Understand the importance of service area competitor analysis as well as its purpose. Understand the relationship between general and health care environmental issue identification and analysis and service area competitor analysis. Define and analyze the service area for a health care organization or specific health service.
- 68. 5 Chapter 3 Learning Objectives Understand the importance of service area competitor analysis as well as its purpose. Understand the relationship between general and health care environmental issue identification and analysis and service area competitor analysis. Define and analyze the service area for a health care organization or specific health service. Conduct a service area structure analysis for a health care organization. 6 Chapter 3 Learning Objectives Understand strategic groups and be able to map competitors’ strategies along important service and market dimensions.
- 69. 7 Chapter 3 Learning Objectives Understand strategic groups and be able to map competitors’ strategies along important service and market dimensions. Understand the elements of service area competitor analysis and assess likely competitor strategies. 8 Chapter 3 Learning Objectives Understand strategic groups and be able to map competitors’ strategies along important service and market dimensions. Understand the elements of service area competitor analysis and assess likely competitor strategies. Aggregate general environmental and health care industry issues with service area and competitor issues and synthesize specific strategy implications. 9 Chapter 3 Learning Objectives Understand strategic groups and be able to map competitors’ strategies along important service and market dimensions.
- 70. Understand the elements of service area competitor analysis and assess likely competitor strategies. Aggregate general environmental and health care industry issues with service area and competitor issues and synthesize specific strategy implications. Suggest several questions to initiate strategic thinking. 10 The Strategic Planning Process Strategic Planning Situation Analysis Strategy Formulation Planning the Implementation External Analysis Internal Analysis Directional Strategies Directional Strategies Adaptive Strategies
- 71. Market Entry Strategies Competitive Strategies Service Delivery Strategies Support Strategies Action Plans 11 Focus of Service Area Competitor Analysis Avoid surprises in the marketplace. 12 Focus of Service Area Competitor Analysis Avoid surprises in the marketplace. Provide a forum for leaders to discuss and evaluate their assumptions about the organization’s capabilities, market position, and competition.
- 72. 13 Focus of Service Area Competitor Analysis Avoid surprises in the marketplace. Provide a forum for leaders to discuss and evaluate their assumptions about the organization’s capabilities, market position, and competition. Make everyone aware of significant and formidable competitors to whom the organization must respond. 14 Focus of Service Area Competitor Analysis Avoid surprises in the marketplace. Provide a forum for leaders to discuss and evaluate their assumptions about the organization’s capabilities, market position, and competition. Make everyone aware of significant and formidable competitors to whom the organization must respond. Help the organization learn from rivals through benchmarking (specific measures comparing the organization with its competitors on a set of key variables).
- 73. 15 Focus of Service Area Competitor Analysis Build consensus among executives on the organization’s goals and capabilities, thus increasing their commitment to the chosen strategy. 16 Focus of Service Area Competitor Analysis Build consensus among executives on the organization’s goals and capabilities, thus increasing their commitment to the chosen strategy. Foster strategic thinking throughout the organization. 17 Focus of Service Area Competitor Analysis Build consensus among executives on the organization’s goals and capabilities, thus increasing their commitment to the chosen strategy. Foster strategic thinking throughout the organization. Identify market niches and discontinuities.
- 74. 18 Focus of Service Area Competitor Analysis Build consensus among executives on the organization’s goals and capabilities, thus increasing their commitment to the chosen strategy. Foster strategic thinking throughout the organization. Identify market niches and discontinuities. Select a viable strategy. 19 Focus of Service Area Competitor Analysis Build consensus among executives on the organization’s goals and capabilities, thus increasing their commitment to the chosen strategy. Foster strategic thinking throughout the organization. Identify market niches and discontinuities. Select a viable strategy. Contribute to the successful implementation of the strategy.
- 75. 20 Focus of Service Area Competitor Analysis Build consensus among executives on the organization’s goals and capabilities, thus increasing their commitment to the chosen strategy. Foster strategic thinking throughout the organization. Identify market niches and discontinuities. Select a viable strategy. Contribute to the successful implementation of the strategy. Anticipate competitors’ moves. 21 Focus of Service Area Competitor Analysis Build consensus among executives on the organization’s goals and capabilities, thus increasing their commitment to the chosen strategy. Foster strategic thinking throughout the organization. Identify market niches and discontinuities. Select a viable strategy. Contribute to the successful implementation of the strategy. Anticipate competitors’ moves. Shorten the time required to respond (countermoves) to a competitor’s moves.
- 76. 22 Obstacles to Effective Service Area Competitor Analysis Misjudging industry and service area boundaries Poor identification of the competition Overemphasis on competitors’ visible competence Overemphasis on where, rather than how, to compete Faulty assumptions about the competition Paralysis by analysis 23 Service Area Competitor Analysis Define the Service Categories 24 Service Area Competitor Analysis Define the Service Categories Define the Service Area
- 77. 25 Service Area Competitor Analysis Define the Service Categories Define the Service Area Create a Service Area Profile 26 Service Area Competitor Analysis Define the Service Categories Define the Service Area Create a Service Area Profile Conduct Service Area Structure Analysis 27 Service Area Competitor Analysis Define the Service Categories Define the Service Area Create a Service Area Profile Conduct Service Area Structure Analysis Conduct Competitor Analysis
- 78. 28 Service Area Competitor Analysis Define the Service Categories Define the Service Area Create a Service Area Profile Conduct Service Area Structure Analysis Conduct Competitor Analysis Map Strategic Groups 29 Service Area Competitor Analysis Define the Service Categories Define the Service Area Create a Service Area Profile Conduct Service Area Structure Analysis Conduct Competitor Analysis Map Strategic Groups Synthesize Analyses 30
- 79. Beginning a Service Area Competitor Analysis Defining the Service Category 31 Beginning a Service Area Competitor Analysis Defining the Service Category Determining Service Area Boundaries 32 Beginning a Service Area Competitor Analysis Defining the Service Category Determining Service Area Boundaries Service Area Profile 33 Beginning a Service Area Competitor Analysis Defining the Service Category
- 80. Determining Service Area Boundaries Service Area Profile Service Area Structure Analysis 34 Bargaining Power of Suppliers Suppliers Bargaining Power of Buyers Buyers Substitutes Threat of Substitute Products or Services Rivalry Potential Entrants
- 81. Rivalry Among Existing Competitors Threat of New Entrants Services Analysis – Five Forces that Indicate the Viability of a Product or Service 35 Service Area Structural Analysis Porter’s Five Forces Threat of new entrants to the market 36 Barriers to Entry Existing organizations have economies of scale High volume, lower costs. Existing product or service differentiation It costs a great deal (capital) to get into this type of business Switching from one service provider to another is expensive Exclusive access to distribution channels Current service providers have developed cost advantages
- 82. independent of scale There are government or legal constraints 37 Service Area Structural Analysis Porter’s Five Forces Threat of new entrants to the market Level of rivalry among existing organizations 38 Intensity of Rivalry Numerous or equally balanced competitors? Slow market growth for these types of services? High fixed costs (buildings, equipment)? Competitors’ products or services are pretty much the same? Switching from one service provider to another is easy? Difficult to leave the business once in it? Competitors place great importance on achieving success?
- 83. 39 Service Area Structural Analysis Porter’s Five Forces Threat of new entrants to the market Level of rivalry among existing organizations Threat of substitute products and services 40 Threats of Substitute Services Many services available that perform about the same function There are lower cost substitute services Buyers of the service tend to experiment or substitute often Buyers of the service have difficulty in telling the difference in the effectiveness of the alternatives 41 Service Area Structural Analysis Porter’s Five Forces Threat of new entrants to the market
- 84. Level of rivalry among existing organizations Threat of substitute products and services Bargaining power of buyers (customers) 42 Bargaining Power of Buyers Buyers of the service purchase in large volume or concentrates purchases Purchases products that are standard Buyers view all providers as having about the same service and quality? Buyers have low switching costs in changing to another provider Buyers have low profitability or narrow margins Pose a threat of backward integration Buyers could begin providing the service themselves? Buyers has low quality requirements Has enough information to gain bargaining leverage 43 Service Area Structural Analysis Porter’s Five Forces Threat of new entrants to the market
- 85. Level of rivalry among existing organizations Threat of substitute products and services Bargaining power of buyers (customers) Bargaining power of suppliers 44 Bargaining Power of Suppliers Few suppliers (personnel, equipment, materials) Few substitutes for the supplies The supplier’s products or services are unique The product or service supplied is important to the buyer’s business Switching costs from one supplier to another are high The buyer’s industry is not considered an important customer The suppliers pose a threat of forward integration 45 Favorable Forces If all five forces are favorable: Little or friendly competition
- 86. 46 Favorable Forces If all five forces are favorable: Little or friendly competition Difficult for new competitors to enter the business 47 Favorable Forces If all five forces are favorable: Little or friendly competition Difficult for new competitors to enter the business Few or no good substitutes for the product or service
- 87. 48 Favorable Forces If all five forces are favorable: Little or friendly competition Difficult for new competitors to enter the business Few or no good substitutes for the product or service Buyers will not control the price, quality, design, or volume 49 Favorable Forces If all five forces are favorable: Little or friendly competition Difficult for new competitors to enter the business Few or no good substitutes for the product or service Buyers will not control the price, quality, design, or volume Suppliers will not control the inputs to production
- 88. 50 Unfavorable Forces If all five forces are unfavorable: A great deal or very unfriendly competition 51 Unfavorable Forces If all five forces are unfavorable: A great deal or very unfriendly competition Easy for new competitors to enter the business 52 Unfavorable Forces If all five forces are unfavorable: A great deal or very unfriendly competition Easy for new competitors to enter the business
- 89. Many good substitutes for the product or service 53 Unfavorable Forces If all five forces are unfavorable: A great deal or very unfriendly competition Easy for new competitors to enter the business Many good substitutes for the product or service Buyers will control the price, quality, design, or volume 54 Unfavorable Forces If all five forces are unfavorable: A great deal or very unfriendly competition Easy for new competitors to enter the business Many good substitutes for the product or service Buyers will control the price, quality, design, or volume Suppliers will control the inputs to production
- 90. 55 Services Analysis A “Three Star” Product or Service Bargaining Power of Suppliers Suppliers Bargaining Power of Buyers Buyers Substitutes Threat of Substitute Products or Services Rivalry
- 91. Potential Entrants Rivalry Among Existing Competitors Threat of New Entrants 56 Services Analysis Evolving Products/Services Viability Bargaining Power of Suppliers
- 92. Suppliers Bargaining Power of Buyers Buyers Substitutes Threat of Substitute Products or Services Rivalry Potential Entrants Rivalry Among Existing Competitors Threat of New Entrants 57
- 93. Services Analysis Evolving Products/Services Viability Bargaining Power of Suppliers Suppliers Bargaining Power of Buyers Buyers Substitutes Threat of Substitute Products or Services Rivalry Potential Entrants Rivalry Among Existing Competitors Threat of New Entrants
- 94. 58 Services Analysis Evolving Products/Services Viability New Regulations or Political Changes New Technologies or Services Improvement Social or Demographic Changes Economic Changes Competitive Changes 59 Beginning a Service Area Competitor Analysis Defining the Service Category Determining Service Area Boundaries Service Area Profile
- 95. Service Area Structure Analysis Competitor Analysis 60 Competitor Analysis & Strategic Groups What are the strengths and weaknesses of your competitors? Can your competitors be “mapped” with respect to two or more dimensions? 61 Competitor Analysis and Mapping Strategic Groups Competitor Strengths and Weaknesses 62 Competitor Analysis and Mapping Strategic Groups
- 96. Competitor Strengths and Weaknesses Service Category Critical Success Factor Analysis 63 Beginning a Service Area Competitor Analysis Defining the Service Category Determining Service Area Boundaries Service Area Profile Service Area Structure Analysis Competitor Analysis Map Strategic Groups 64 Beginning a Service Area Competitor Analysis Defining the Service Category Determining Service Area Boundaries Service Area Profile Service Area Structure Analysis Competitor Analysis
- 97. Map Strategic Groups 65 Service Area Plastic Surgery Competitors For the Charlotte service area, a majority of the plastic surgery practices are pursuing one of four basic strategies and, for the most part, do not engage in between-group competition. Strategic groups one and two have some overlap; however, physicians in group two engage in Third World country medical missions. There is considerable within-group competition particularly in group three where there is a focus on luxurious surroundings and personal attention. Non board-certified plastic surgeons are not shown on this map. Service Area Assisted-Living Competitors
- 98. For this service area, assisted living organizations are pursuing four basic strategies: high price with highly specialized services (Strategic Group 1), low price with few ancillary services (Strategic Group 2), medium price with some (selected) services (Strategic Group 3), and high price with many services (Strategic Group 4). The primary (direct) competitors for these organizations are other organizations within their own strategic group. Customers who seek the attributes of one strategic group, such as highly specialized rehabilitation services, are unlikely to be attracted to another strategic group. These assisted-living organizations should change strategic cautiously as a decision to add services may move an organization to a new strategic group and therefore a new set of competitors. Note that in this example there may be an opportunity to enter or move toward a medium-cost, many services niche and become a strategic group of one. *Range of services included skilled nursing, organized social activities, outings, physical therapy, education, rehabilitation, speech therapy, Alzheimer’s care, nutritional services, infusion, pharmacy, homemaker services, live-ins, companions, and so on.
- 99. 67 Beginning a Service Area Competitor Analysis Defining the Service Category Determining Service Area Boundaries Service Area Profile Service Area Structure Analysis Competitor Analysis Map Strategic Groups Synthesize the Analyses 68 Strategic Thinking Questions Validating the Strategic Assumptions Is the strategy consonant with the competitive environment? Do we have an honest and accurate appraisal of the competition? Have we underestimated the competition? Has the rivalry in the service category/service area changed? Have the barriers to entering the service category/service area changed? Does the strategy leave us vulnerable to the power of a few major customers?
- 100. 69 Strategic Thinking Questions Validating the Strategic Assumptions Has there been any change in the number or attractiveness of substitute products or services? Is the strategy vulnerable to a successful strategic counterattack by competitors? Does the strategy follow that of a strong competitor? Does the strategy pit us against a powerful competitor? Is our market share sufficient to be competitive and generate an acceptable profit? 70 Chapter 3 Conclusions After reading Chapter 3, you should be able to define the following terms: Key TermsKey TermsCompetitive AdvantageService Area ProfileCompetitor AnalysisService Area Structural AnalysisCritical Success Factor AnalysisService CategoryMapping CompetitorsStrategic GroupsService AreaStrategic ResponseService Area Competitor Analysis
- 101. 71 Assignment Service Area Competitor Analysis For the organization and community you selected in the assignment from Chapter 2, complete the task in the next slide. Specifically: Identify the service category and service area; Conduct a Service Area Structural Analysis; Identify the key competitors and try to list their strengths and weaknesses; and Group or Map the competitors into strategic groups. 72