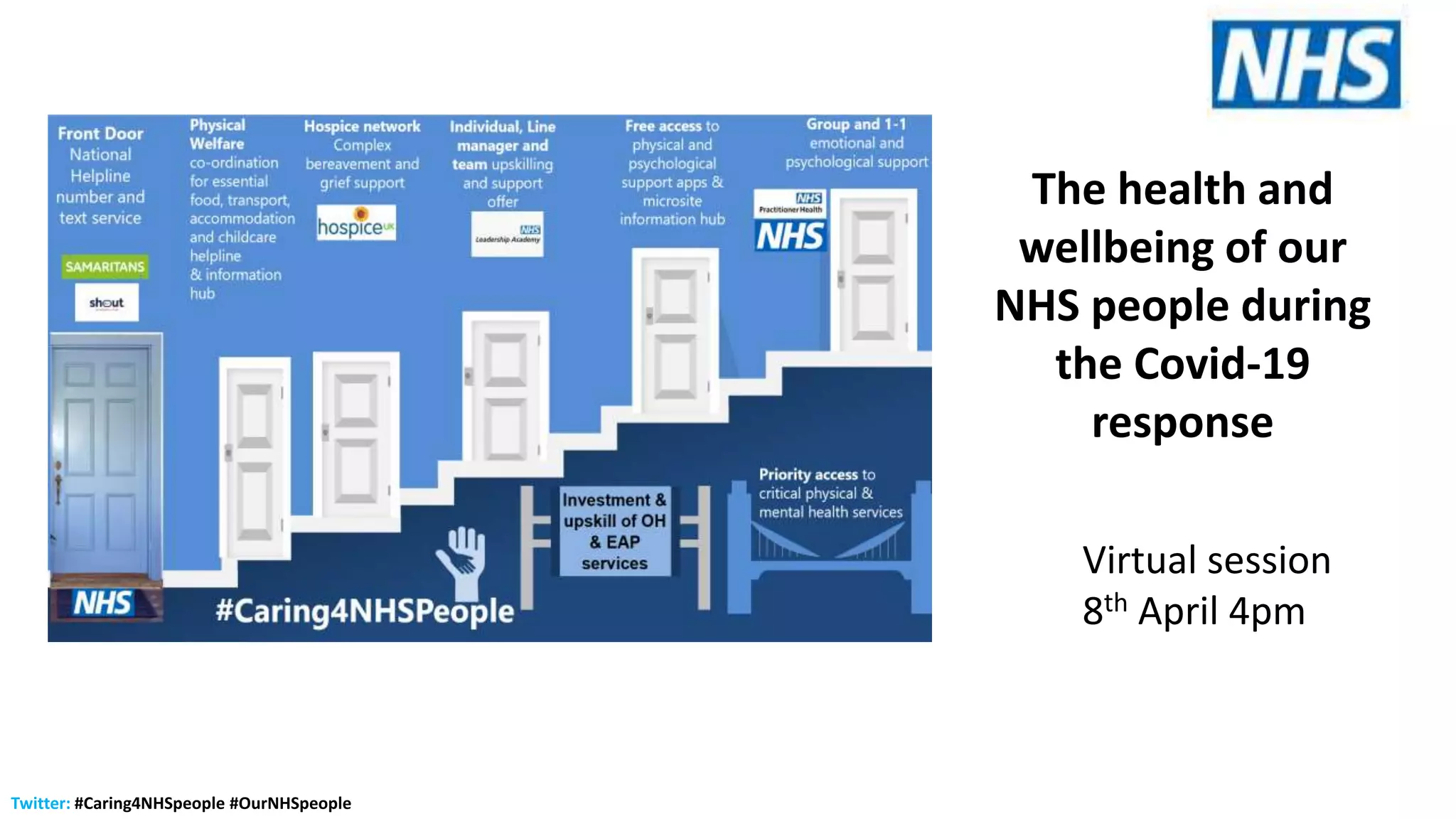
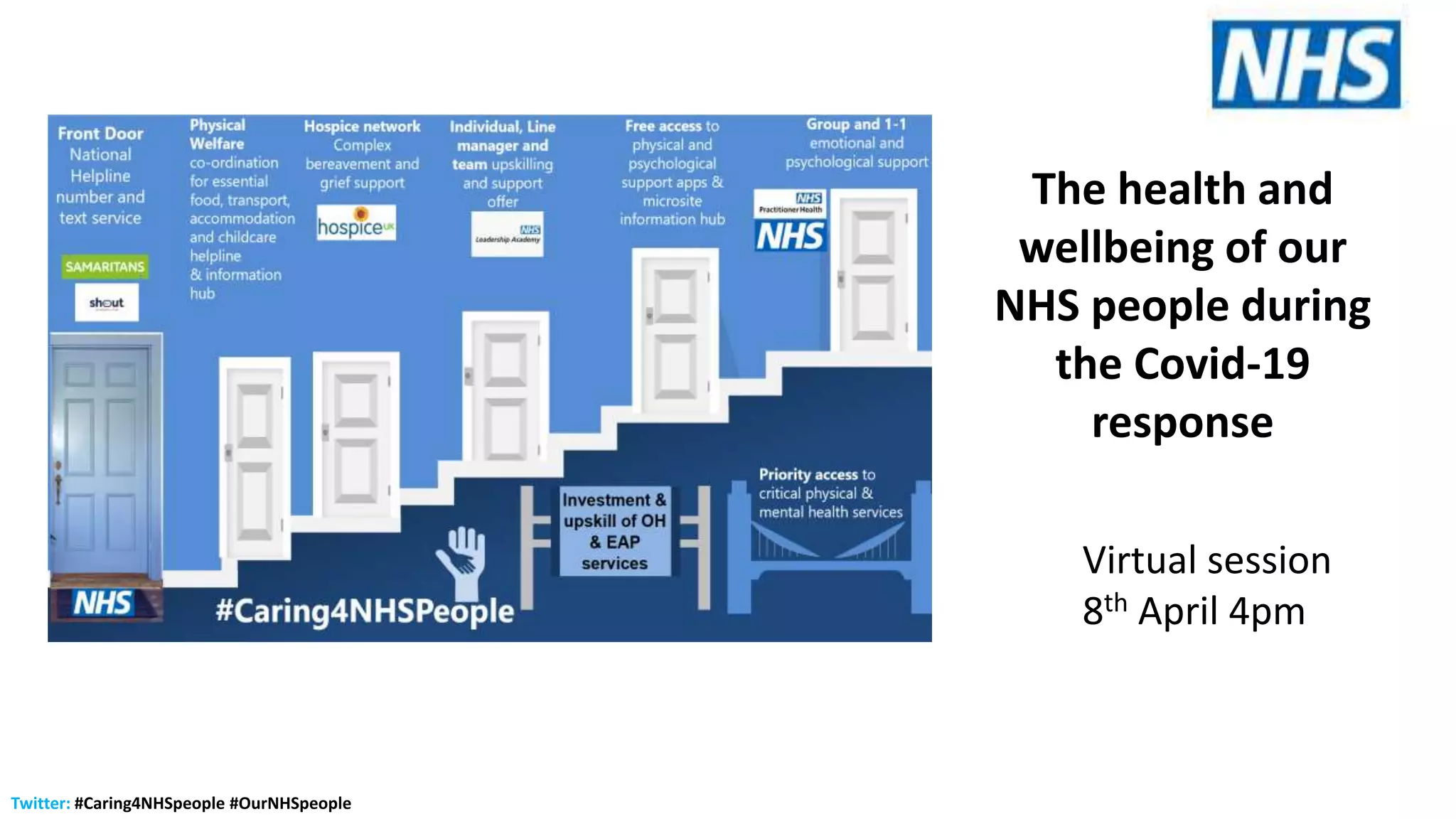
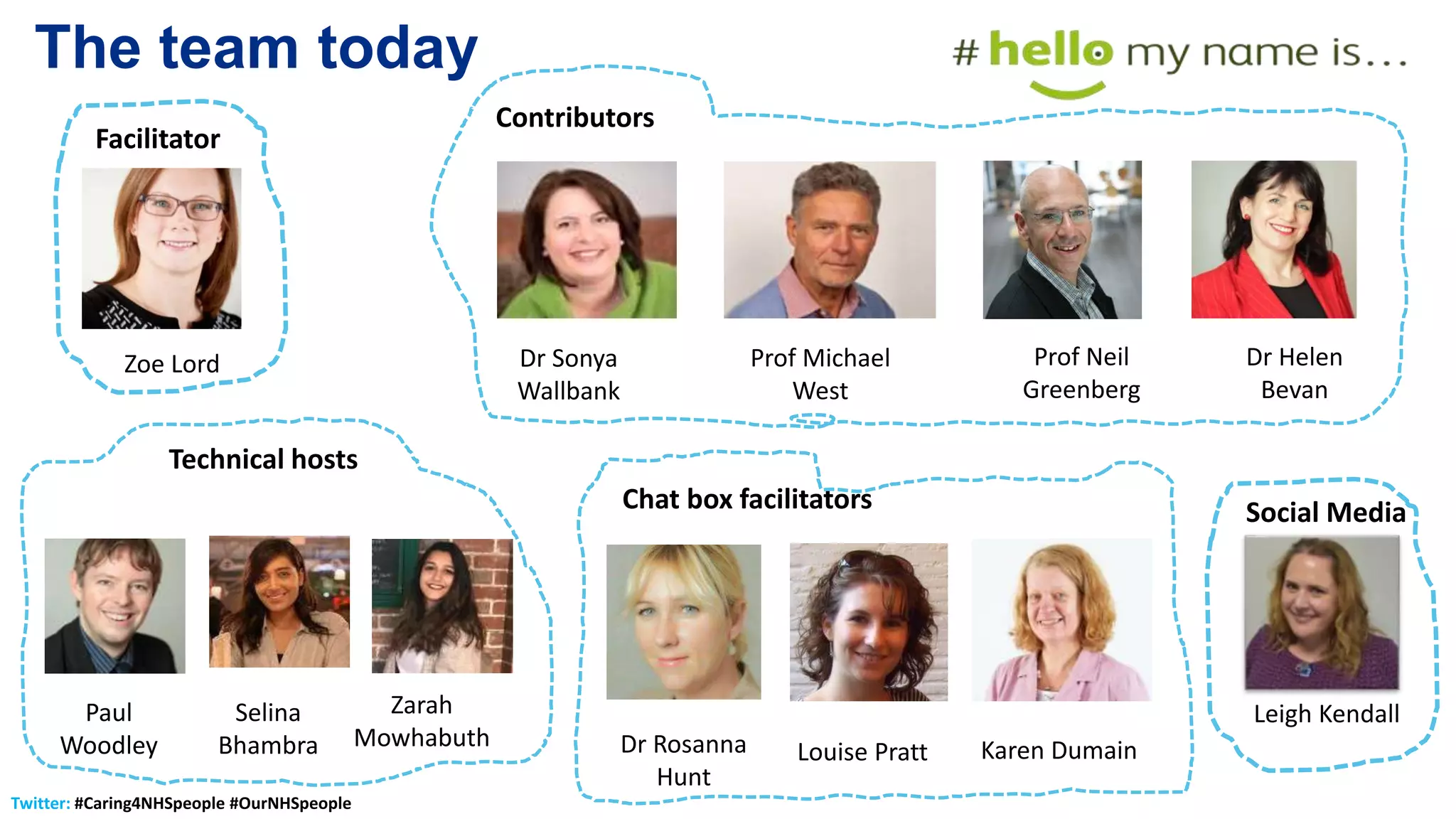
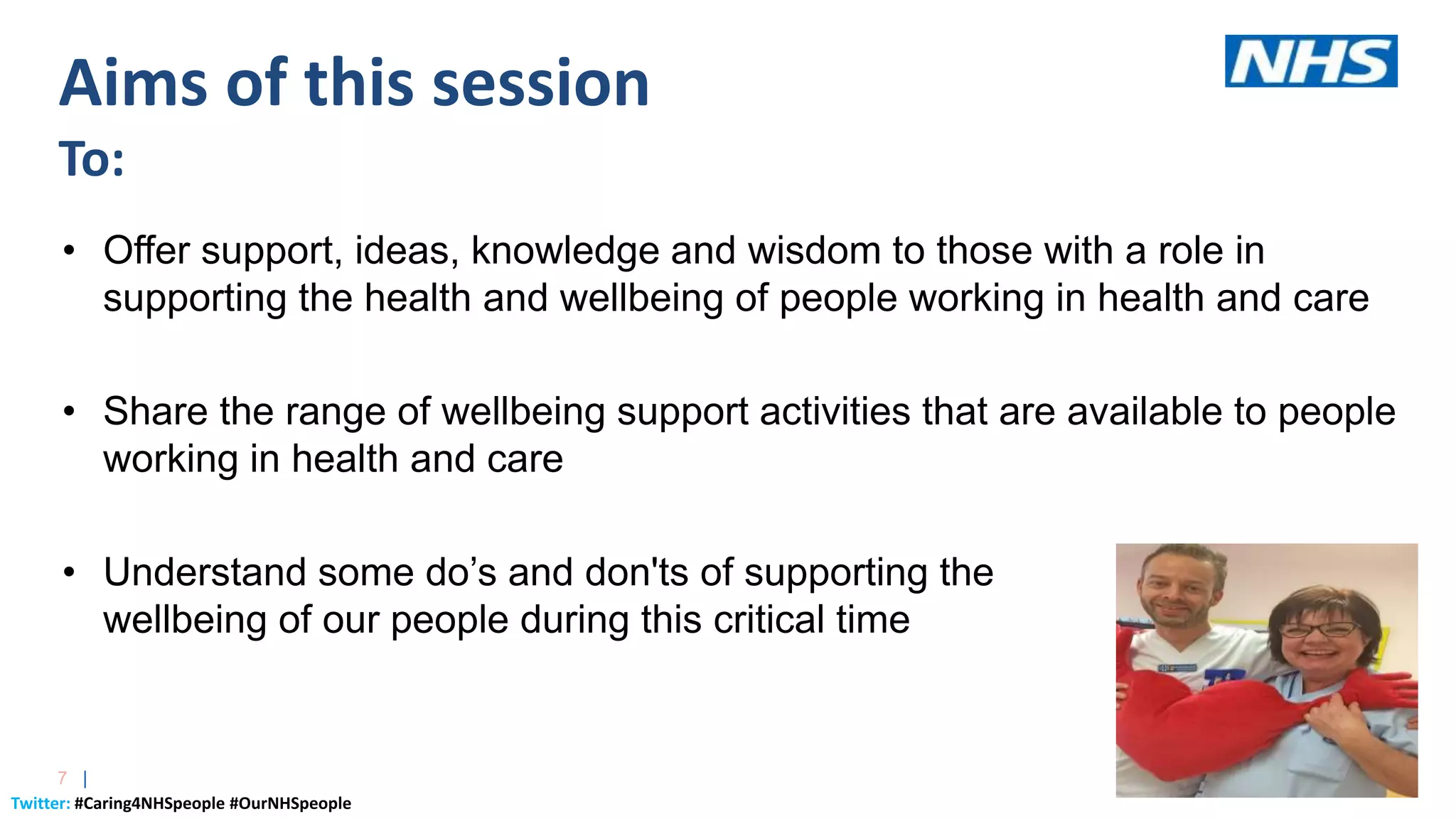
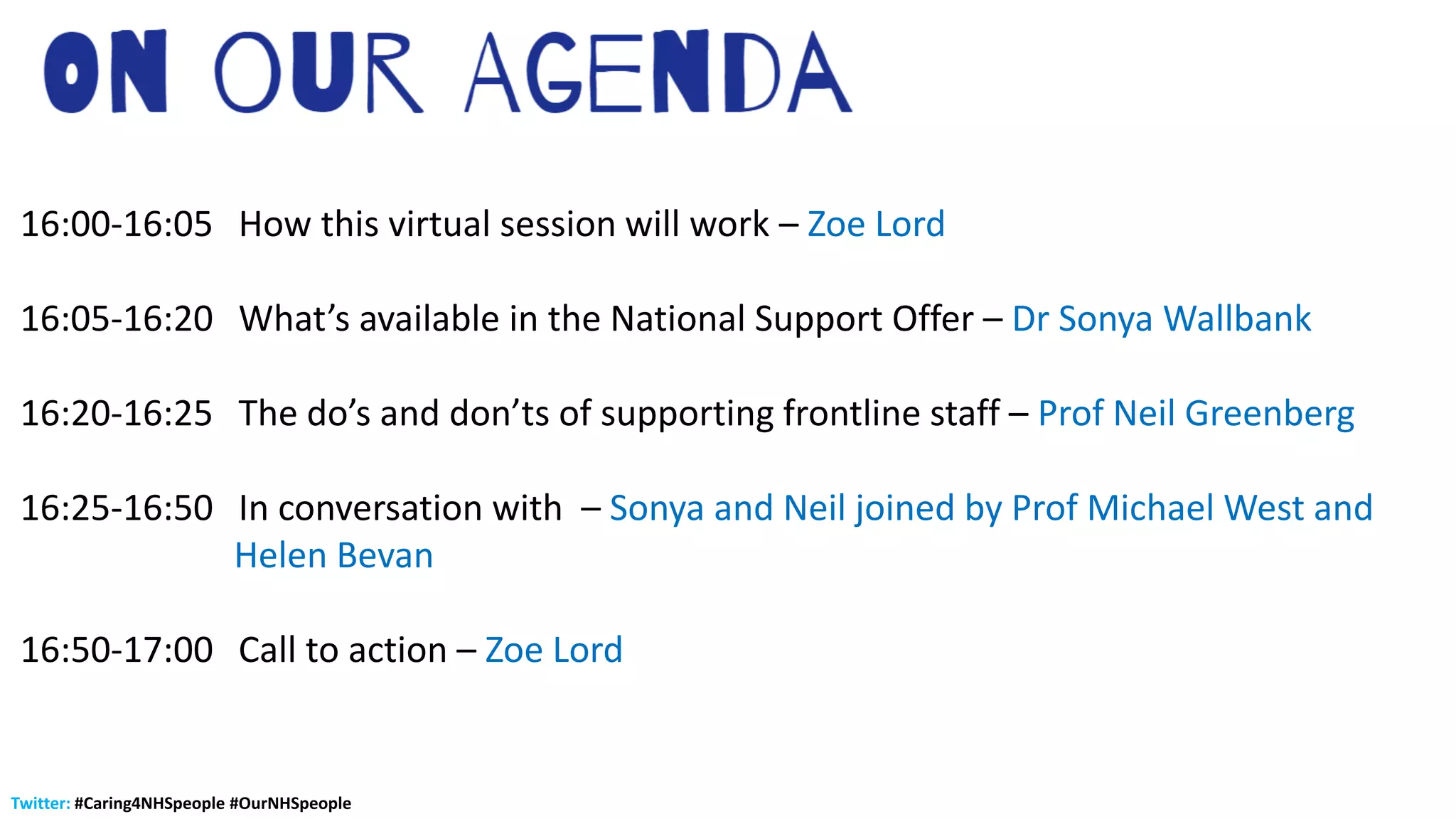
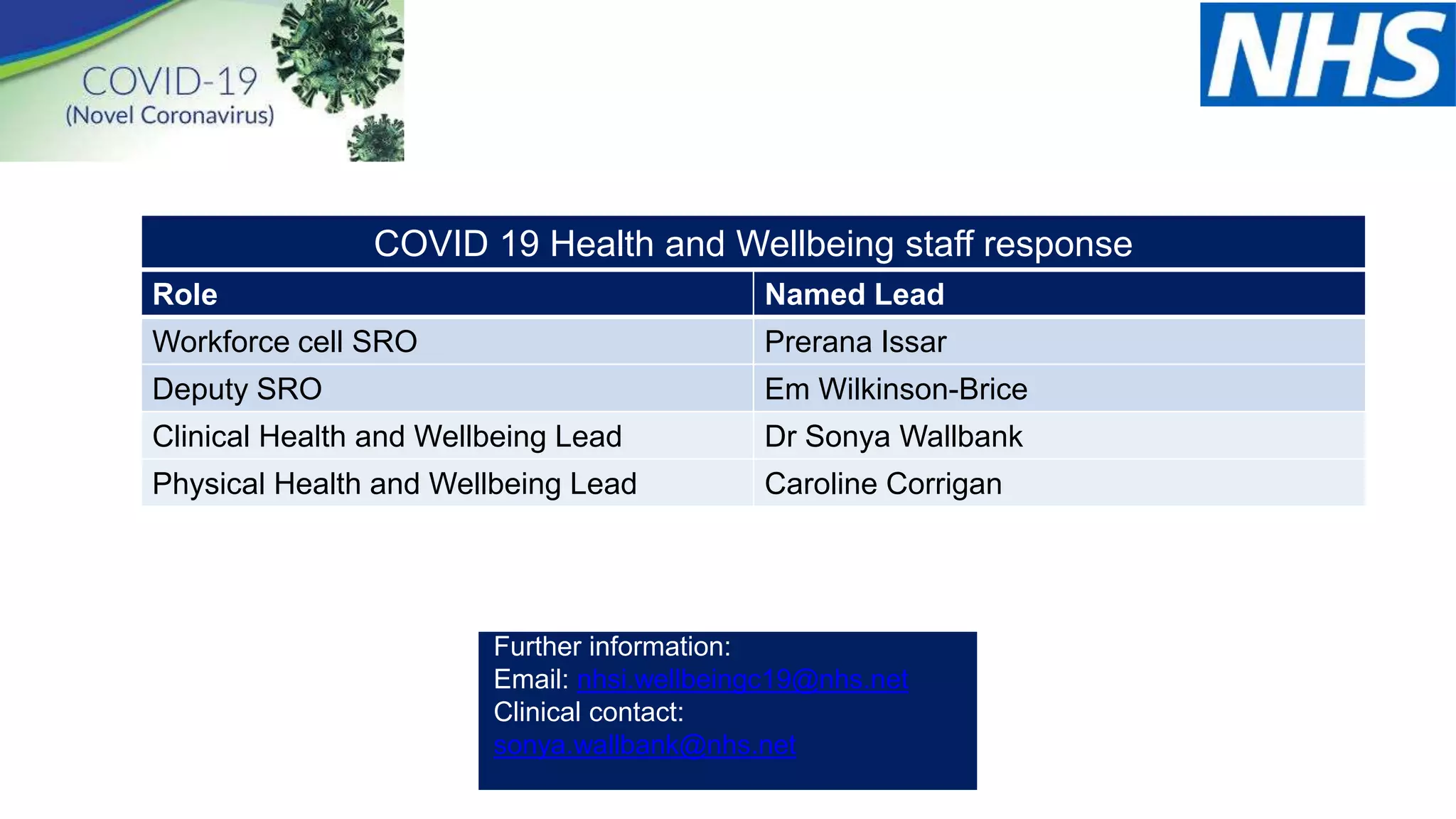
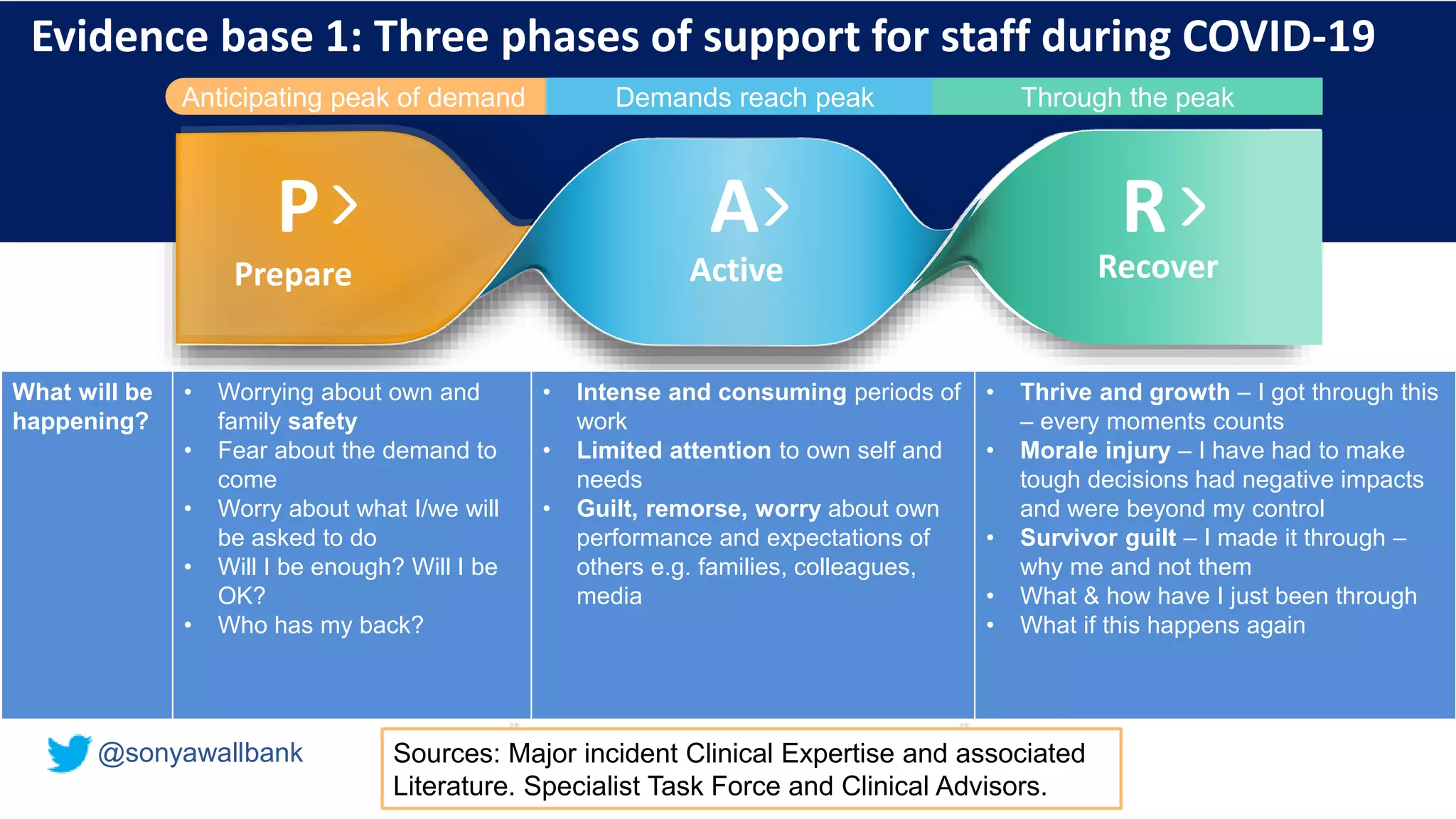
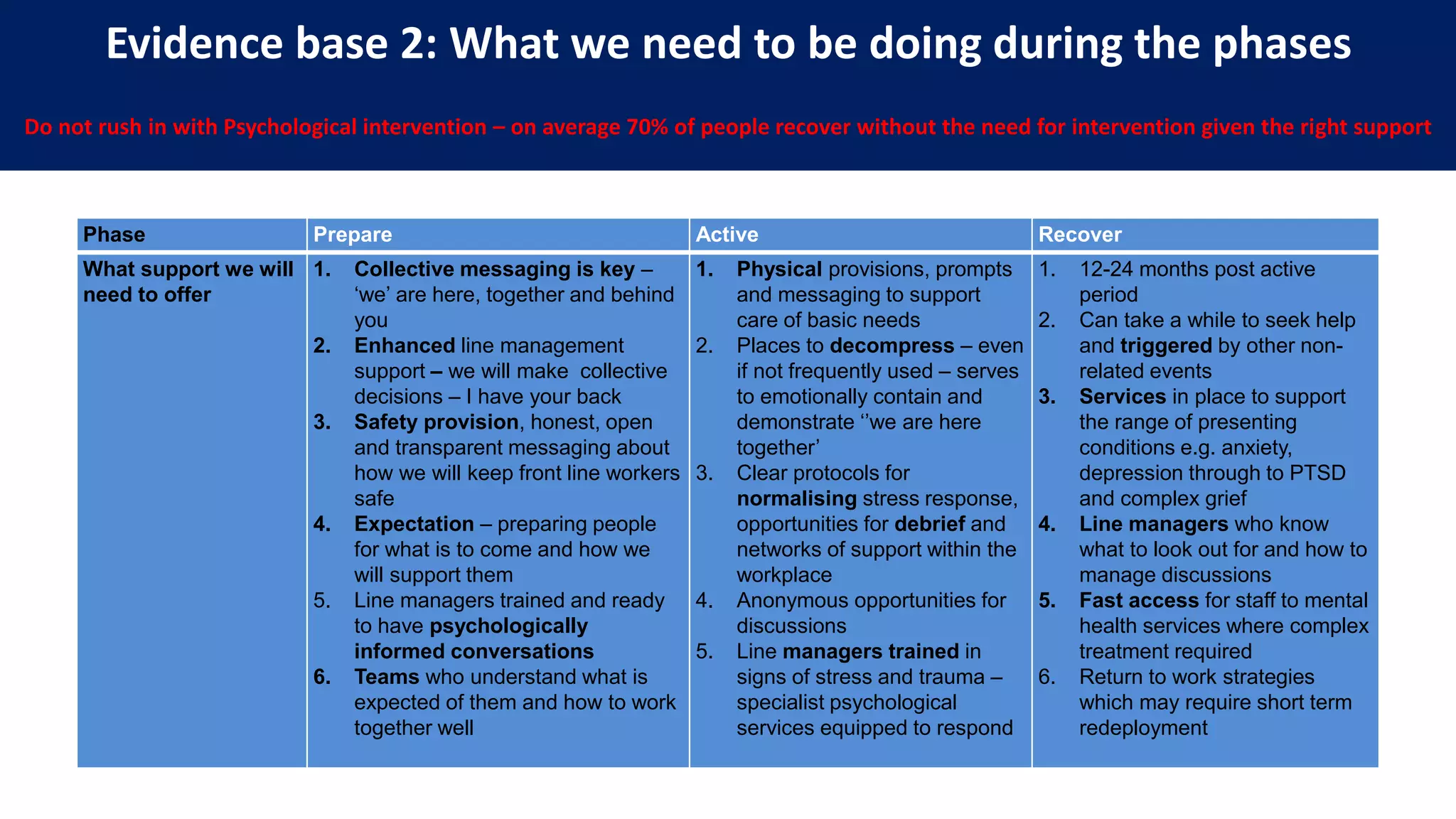
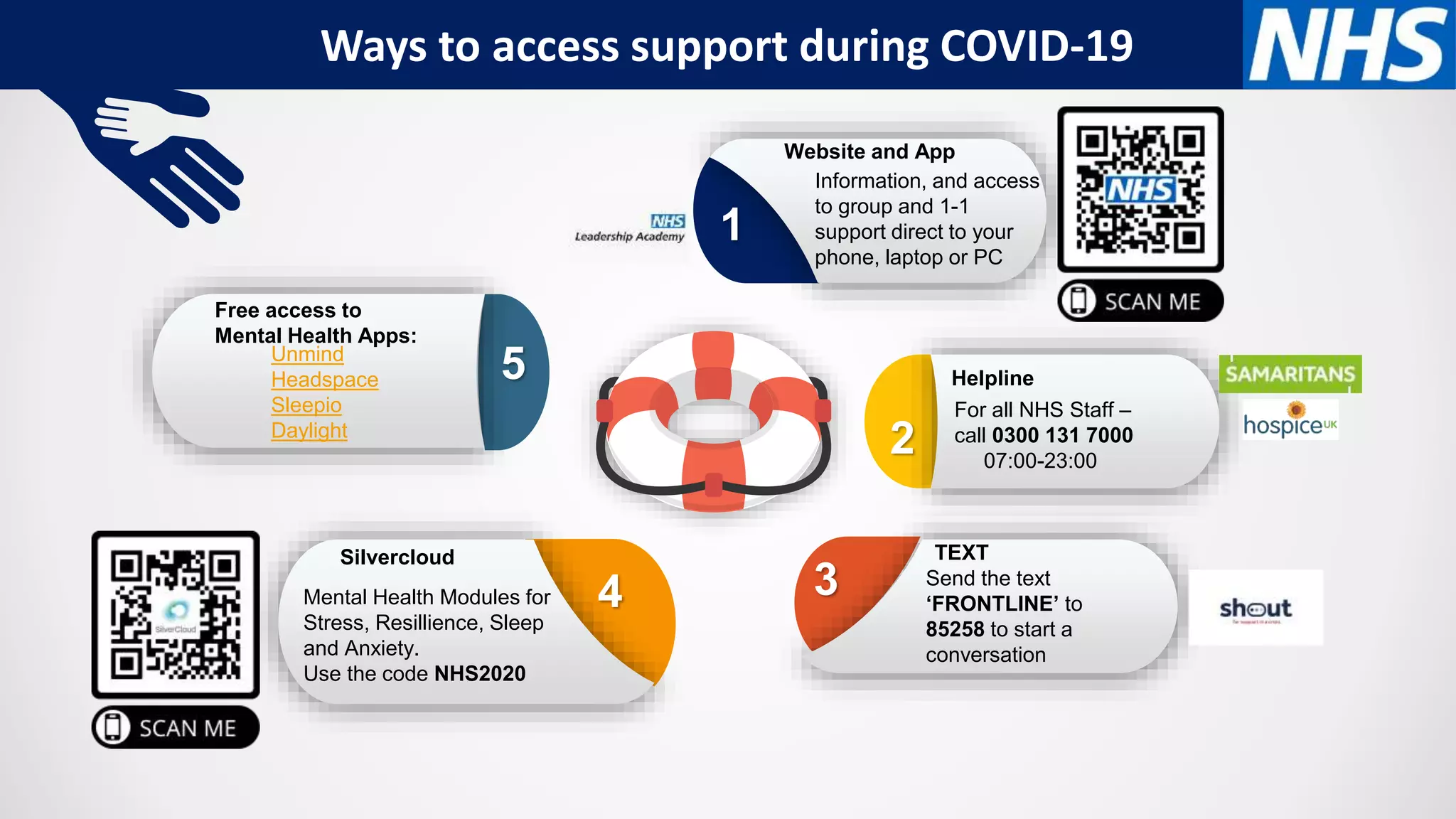
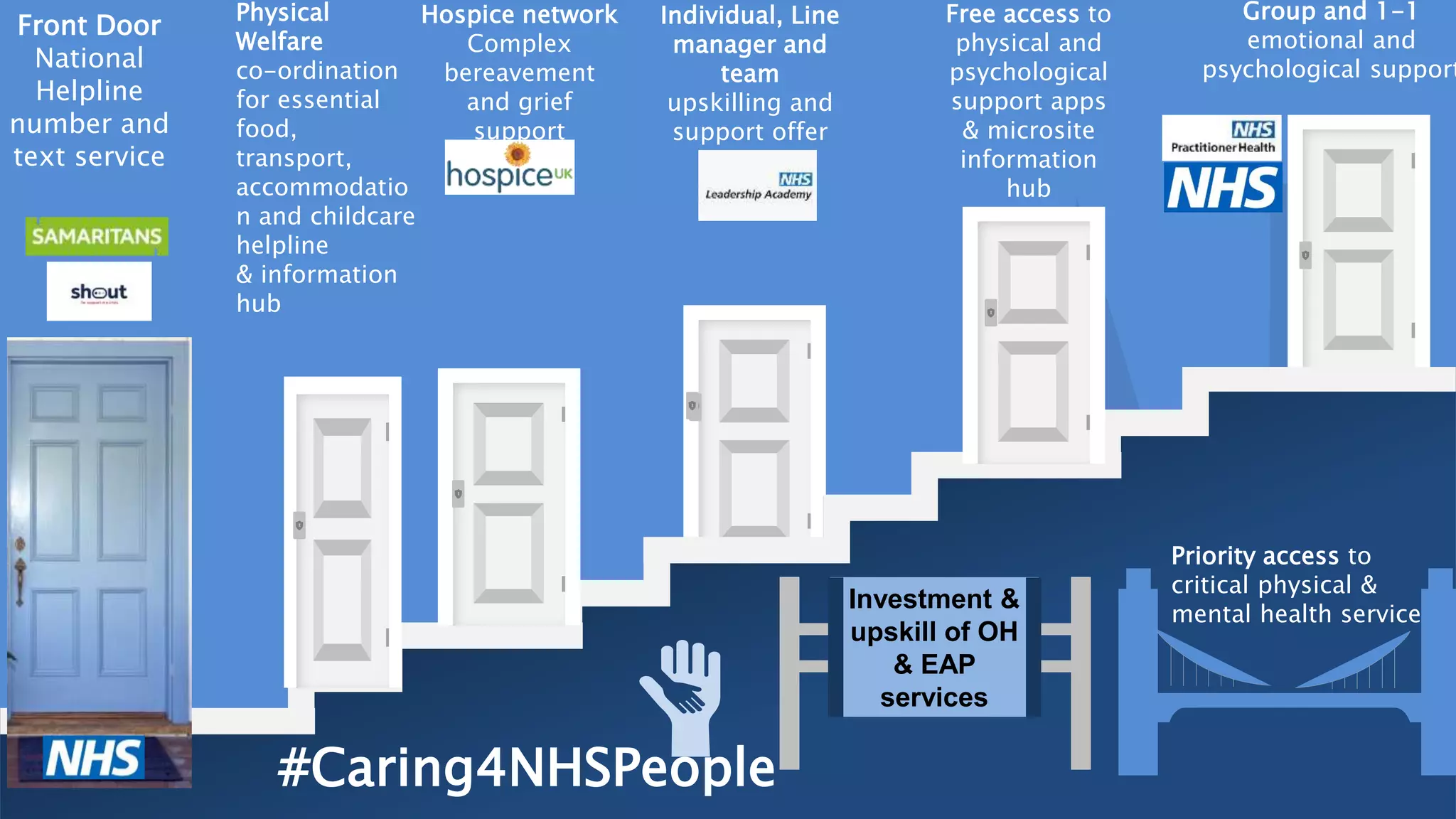
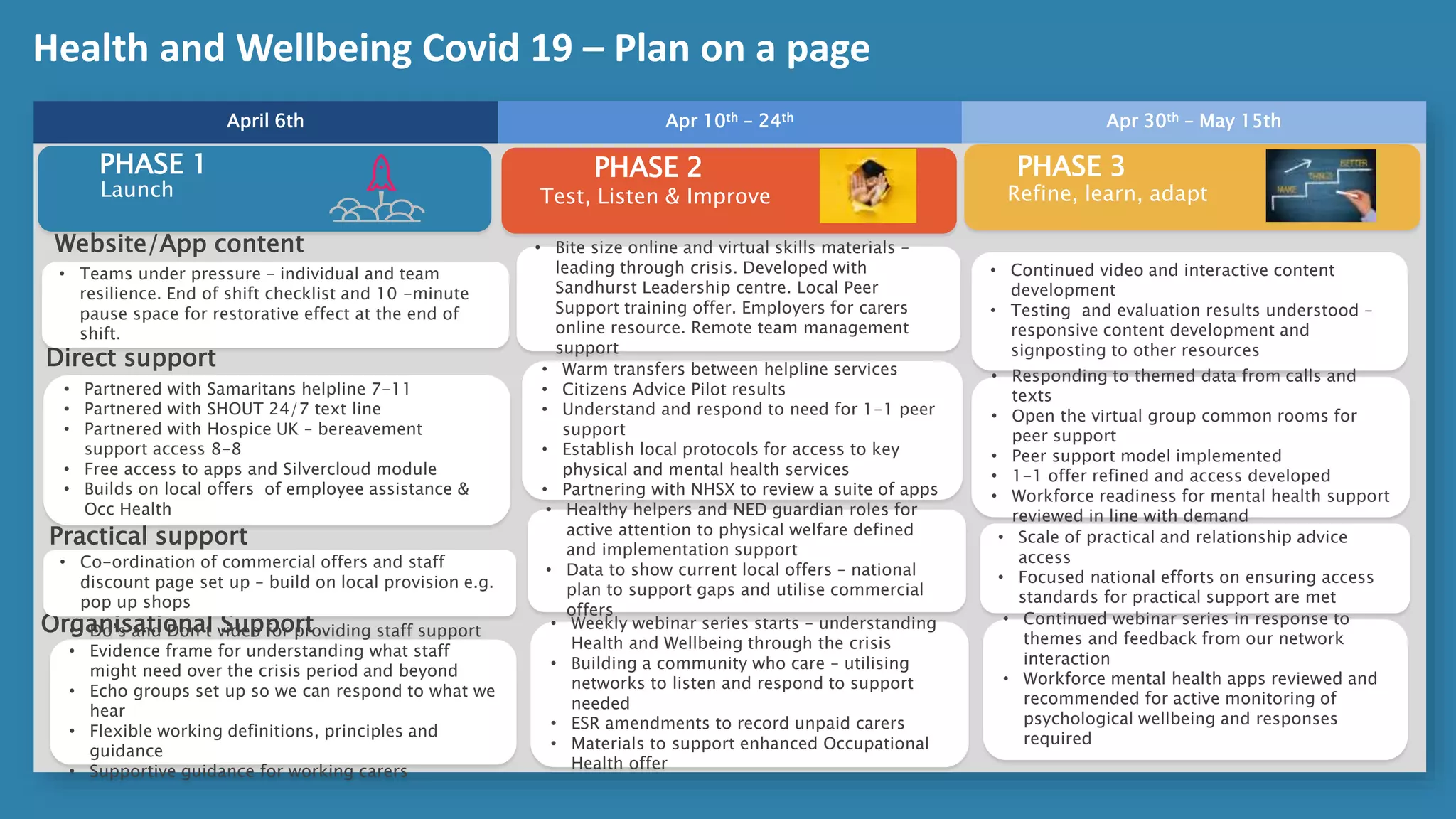
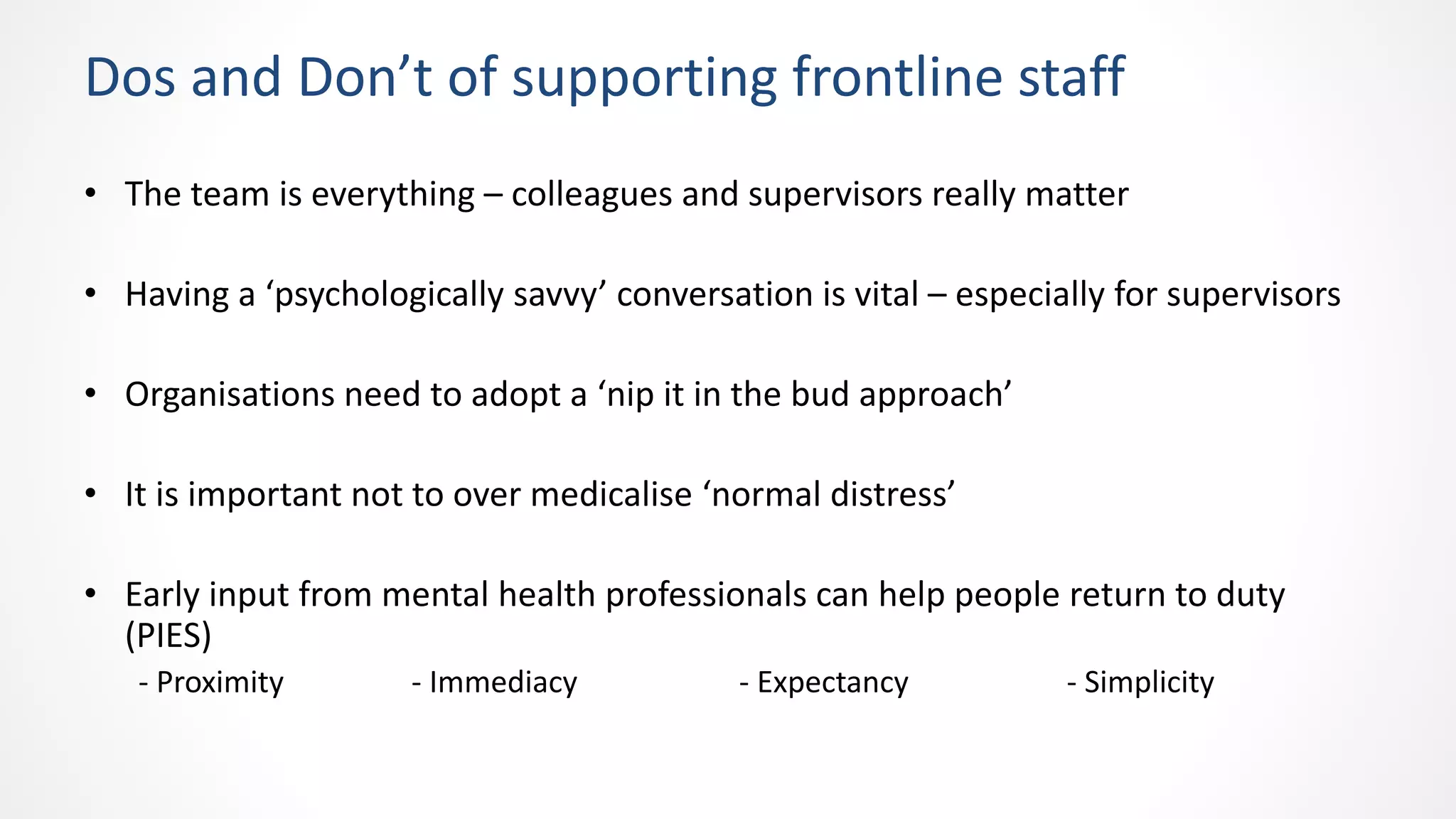
The document outlines a virtual session discussing the health and wellbeing of NHS staff during the COVID-19 response, scheduled for April 8th. The session aims to share support resources and strategies for frontline workers, including mental health services and peer support. It emphasizes the importance of collective support, clear communication, and understanding the psychological needs of staff during and after the crisis.