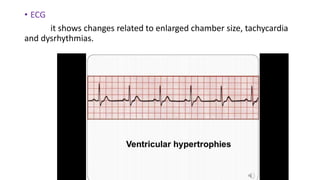
This document defines and describes cardiomyopathy, including its causes, types, symptoms, diagnosis, and treatment. Cardiomyopathy is a group of diseases that weaken and enlarge the heart muscle. There are three main types - dilated, hypertrophic, and restrictive cardiomyopathy. Symptoms vary depending on the type but can include fatigue, shortness of breath, chest pain, and edema. Diagnosis involves tests like echocardiogram, ECG, cardiac catheterization and MRI. Treatment may include medications, lifestyle changes, implanted devices like pacemakers, and even heart transplantation in severe cases. The goal of treatment is to improve cardiac function and quality of life.