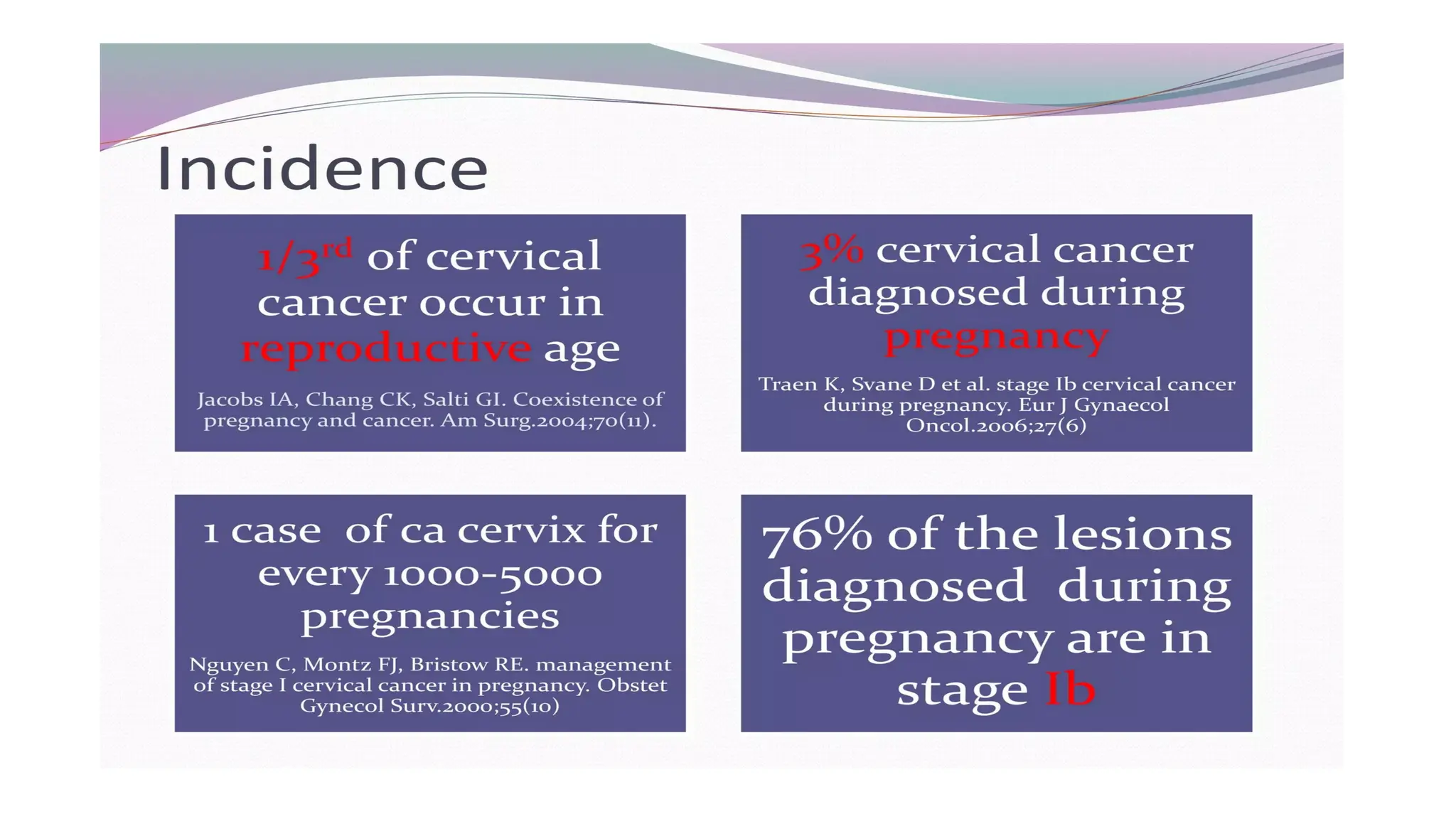
The document discusses the management of cervical cancer during pregnancy, highlighting imaging techniques and treatment options based on the gestational age and cancer stage. It addresses the safety of various diagnostic methods, the impact of pregnancy on disease progression, and the considerations for delivery methods. Key conclusions include the importance of antenatal checkups for early detection and tailored treatment strategies depending on the progression of the disease and the stage of pregnancy.