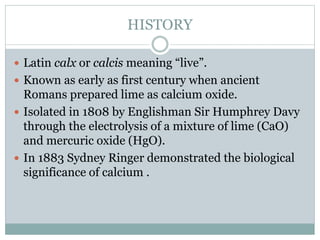
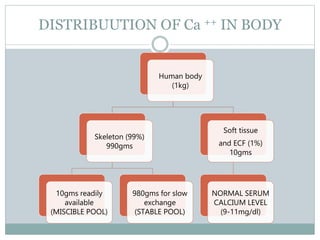
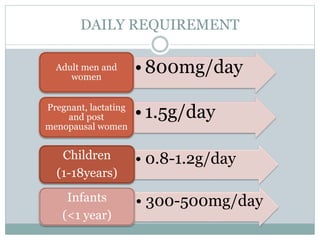
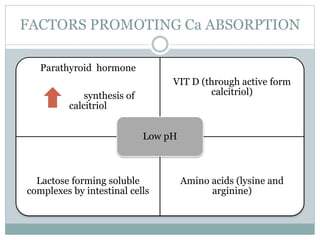
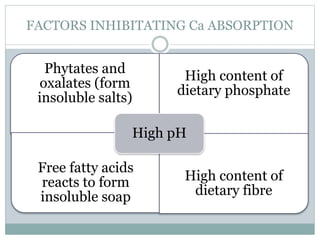
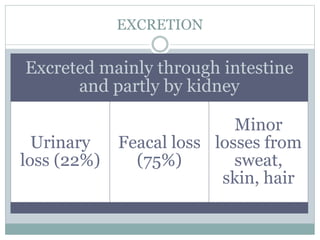
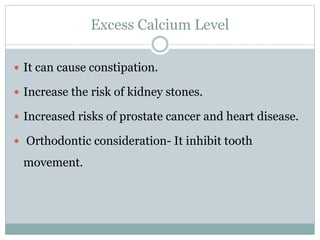
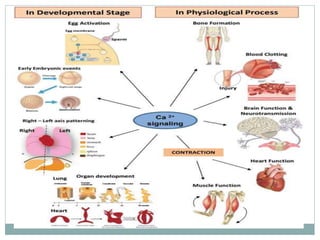
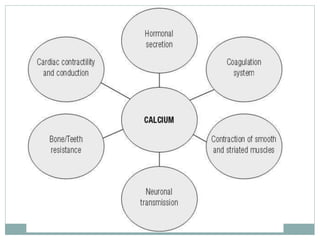
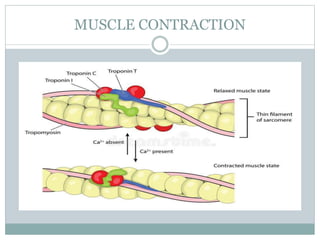
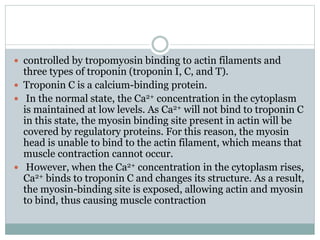
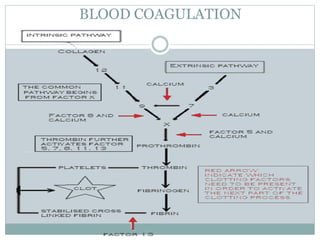
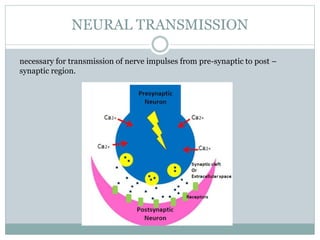
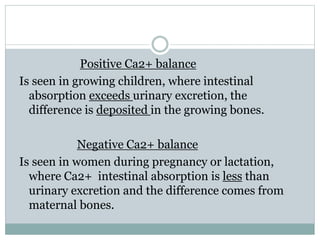
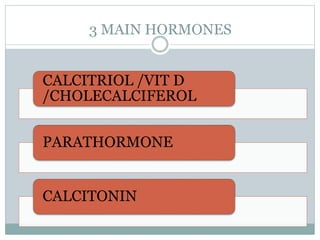
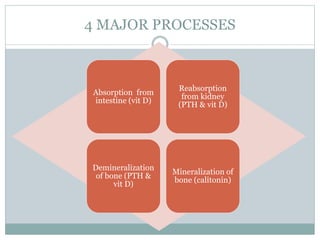
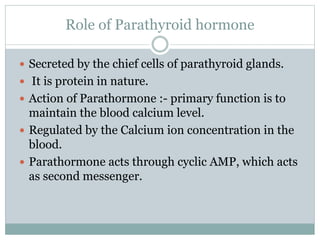
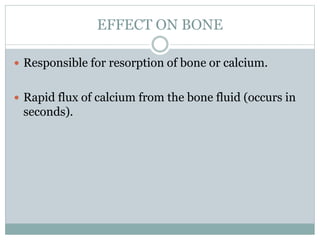
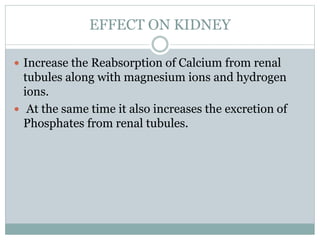
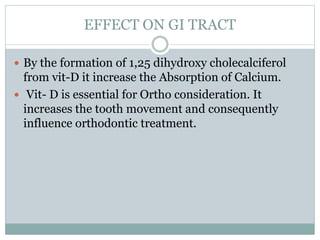
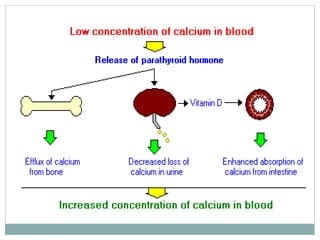
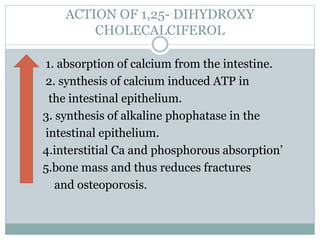
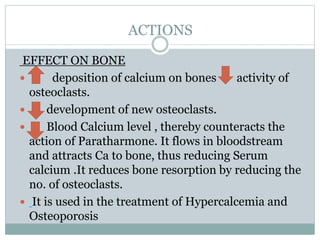
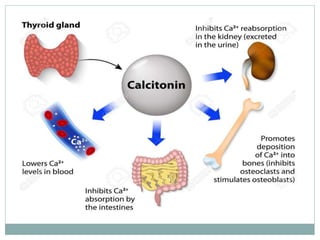
The document provides a comprehensive overview of calcium metabolism, including its history, distribution in the body, daily requirements, sources, absorption mechanisms, and factors affecting absorption. It elaborates on the functions of calcium in bone mineralization, muscle contraction, blood coagulation, and neural transmission, as well as how homeostasis is maintained by various hormones. Additionally, the document discusses the implications of calcium levels on orthodontic tooth movement, emphasizing the importance of calcium in dental health.