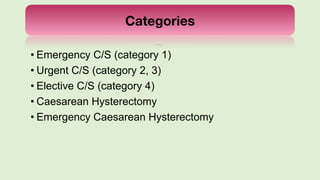
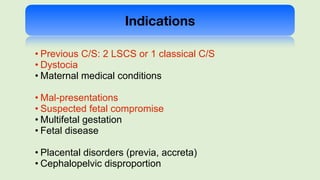
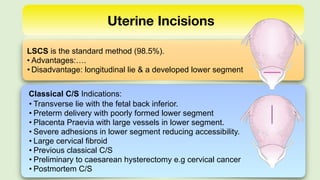
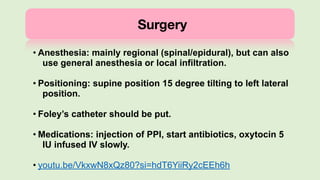
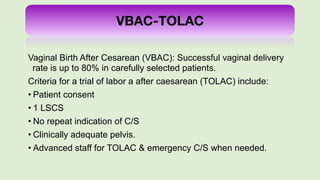
The document provides a comprehensive overview of caesarean sections (c/s), including their history, types, indications, surgical preparation, and post-operative care. It emphasizes the increasing prevalence of c/s globally and details various complications associated with both caesarean and vaginal births after caesarean (VBAC). Additionally, it outlines criteria for trial of labor after caesarean (TOLAC) to facilitate successful vaginal deliveries.