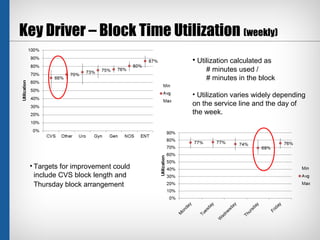
The case study explores the implications of an overflow policy for post-surgery observation patients on inpatient bed utilization, highlighting a significant need for additional observation beds due to patient volume projections. Key findings indicate that delays are influenced by scheduling issues and mismatched block time utilization, necessitating operational alternatives such as reclaiming pre-admission testing rooms for patient care. The study suggests potential trade-offs between increasing observation patient transfers to inpatient floors and managing anticipated delays.