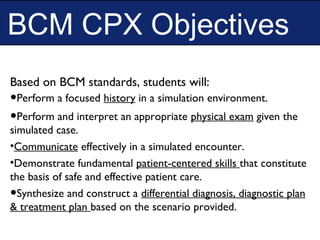
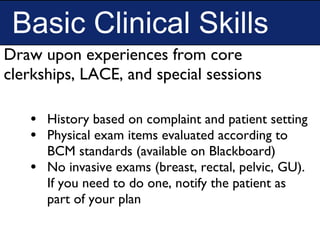
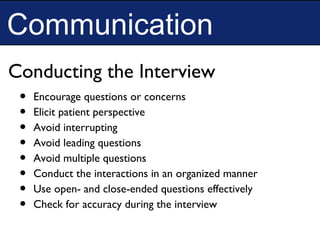
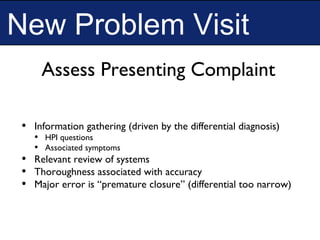
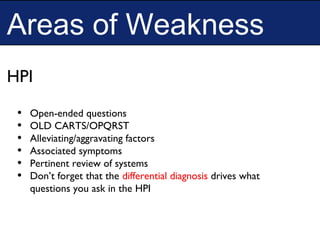
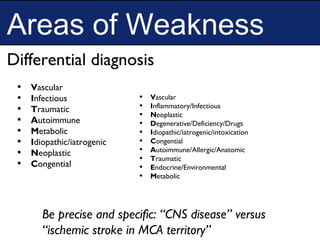
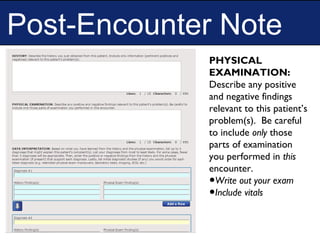
The document summarizes the goals, objectives, framework, and logistics of the BCM Clinical Performance Examination (CPX). The CPX assesses third-year medical students' clinical skills, including history taking, physical exam, communication, and clinical reasoning. It consists of 4 simulated patient cases that students work through individually. Stations evaluate students' basic clinical skills, interpretation of findings, problem solving, and presentation of cases. The document provides guidance on competencies assessed, exam structure and timing, cases types, areas of weakness to focus on, and information on preparing for and scheduling the exam.