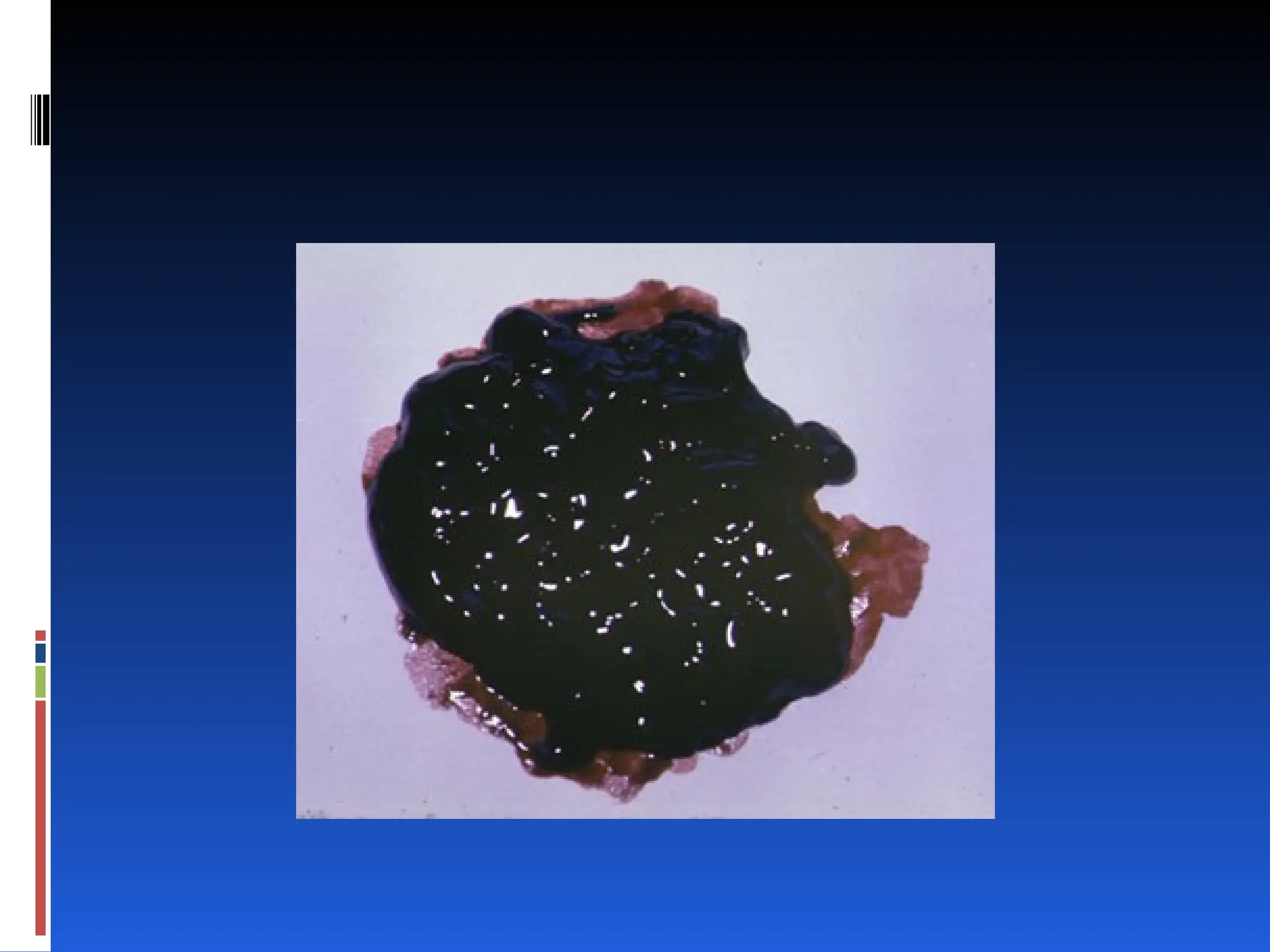
The document discusses the approach to managing gastrointestinal bleeding, highlighting its epidemiology, diagnostic methods, and management strategies. It emphasizes the importance of rapid assessment, stabilization, and the need for timely consultations with specialists to improve patient outcomes. Key findings include the differentiation between upper and lower gastrointestinal bleeding, common causes, and the significance of laboratory testing in evaluating patients.