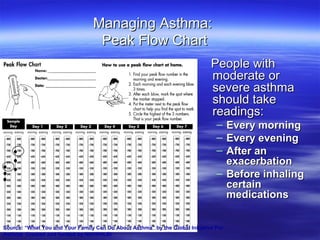
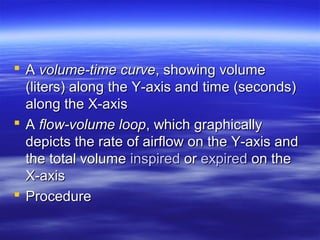
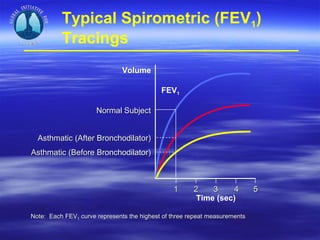
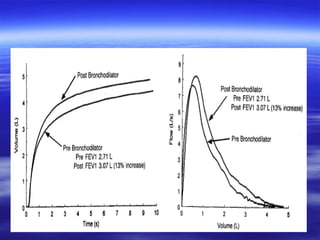
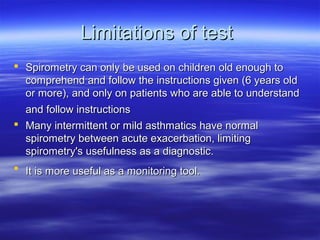
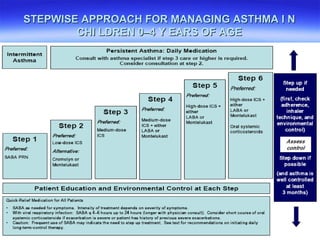
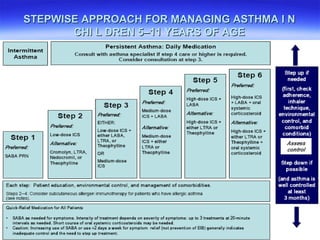
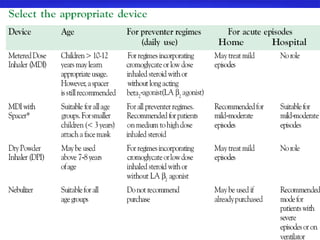
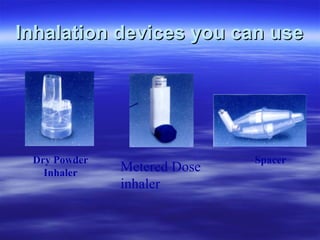
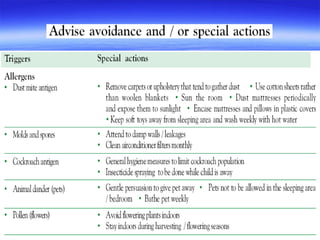
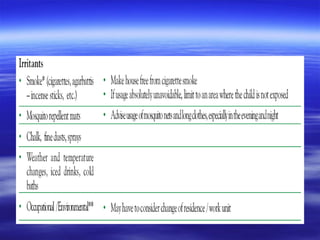
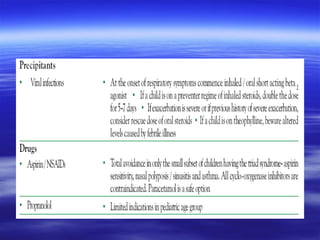
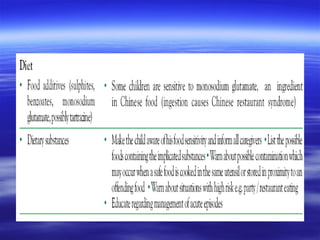
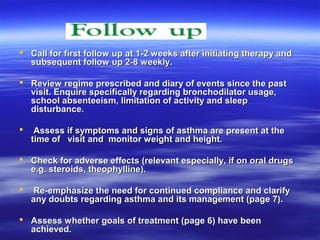
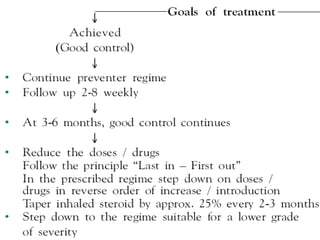
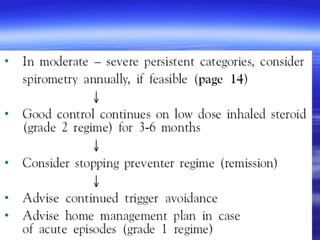
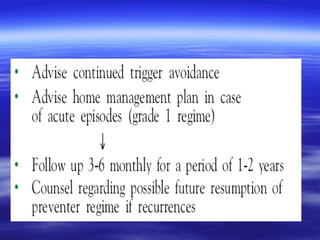
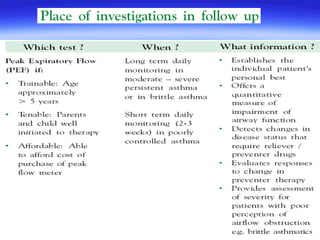
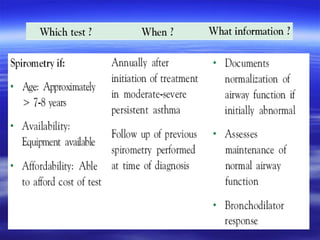
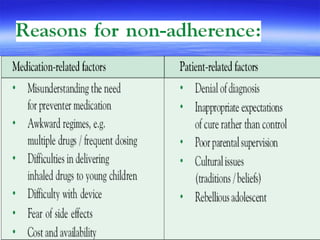
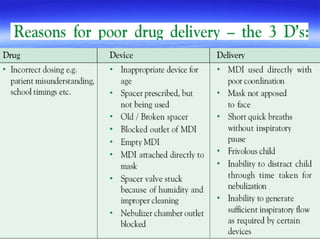
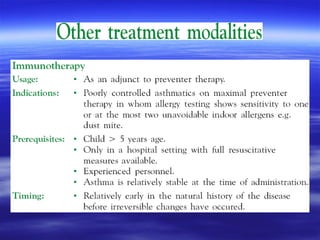
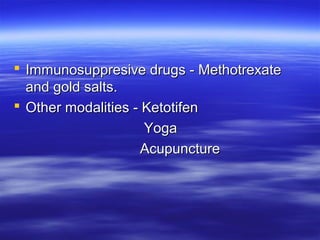
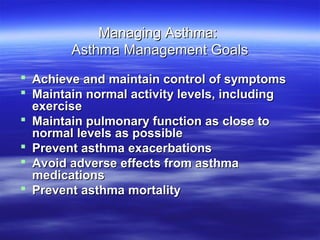
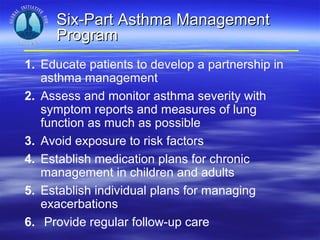
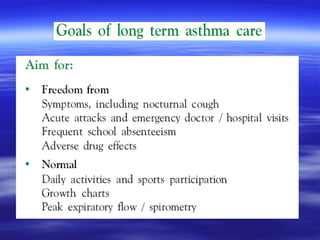
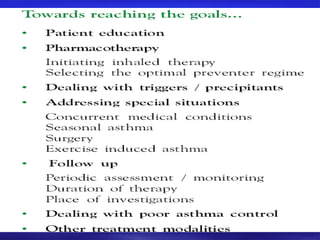
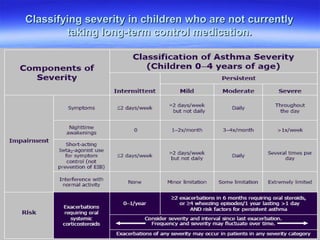
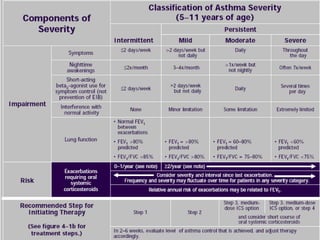
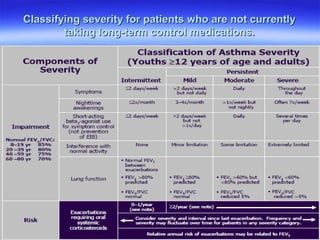
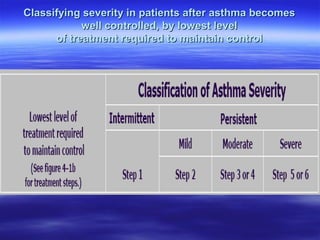
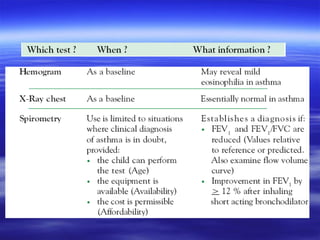
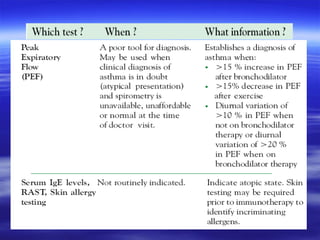
This document provides information on asthma management guidelines and tools. It discusses the goals of asthma management, which include achieving control of symptoms, maintaining normal activity levels, pulmonary function, and preventing exacerbations and mortality. It outlines a six-part asthma management program involving education, assessment, avoiding triggers, medication plans, managing exacerbations, and follow-up care. Classification systems for severity are presented for children and adults. Peak flow meters, spirometry, inhaler devices, and stepwise treatment approaches are also summarized.
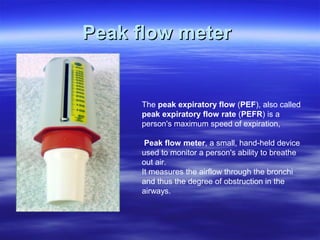
![An easy to remember approximation is: PEFR (L/min) = [Height (cm) - 80] x 5](https://image.slidesharecdn.com/asthma2010newginaguidelines-120921010443-phpapp01/85/Asthma-2010-new-gina-guidelines-pediatric-13-320.jpg)