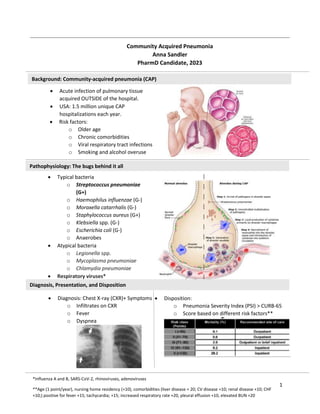
The document discusses community-acquired pneumonia (CAP), including its pathophysiology as an acute infection of the pulmonary tissue acquired outside of the hospital. It provides details on the diagnosis, presentation, and treatment of CAP, noting that typical bacteria include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Empiric antibiotic treatment options for CAP are outlined depending on a patient's risk factors, comorbidities, and severity of illness.