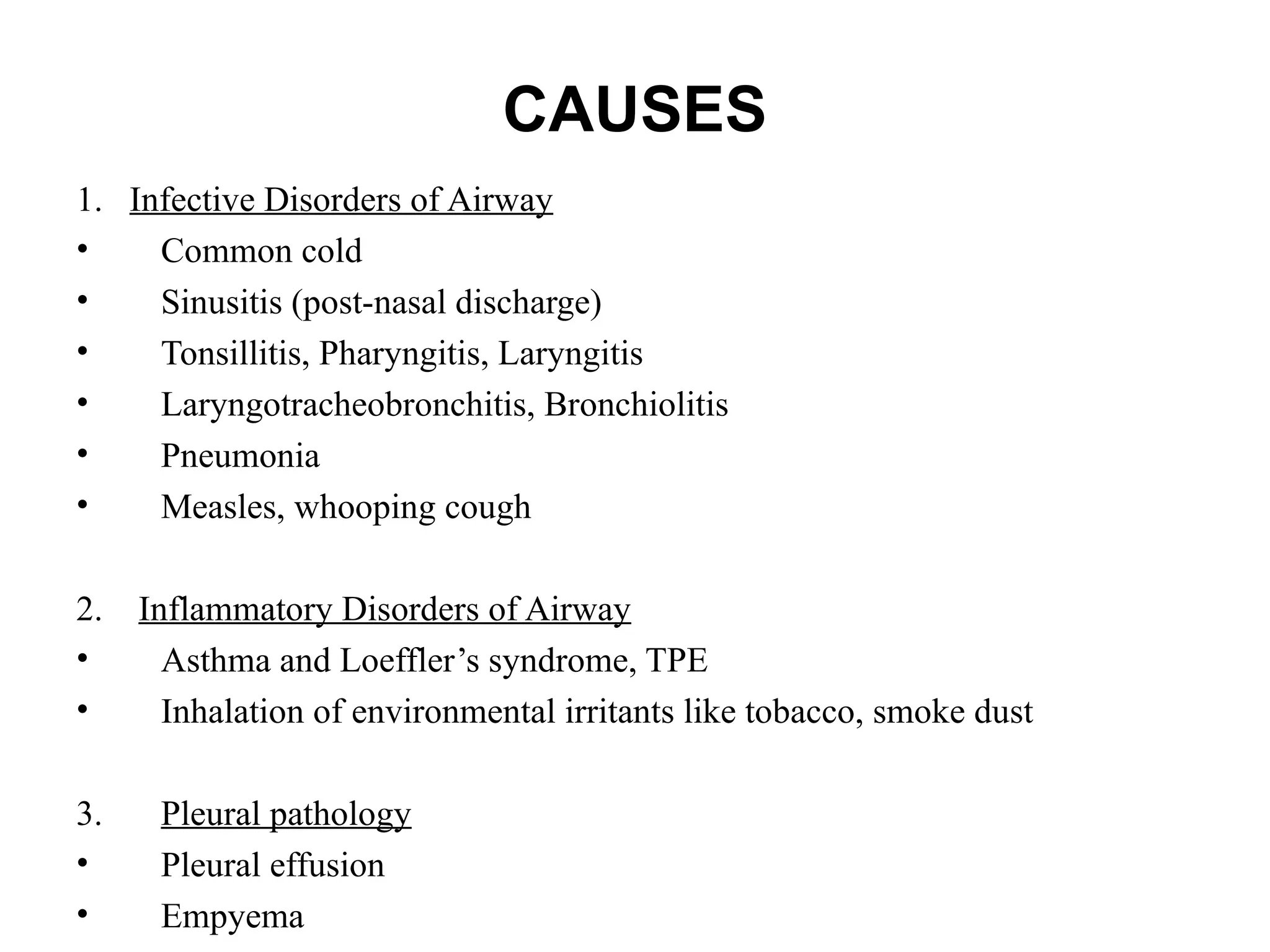
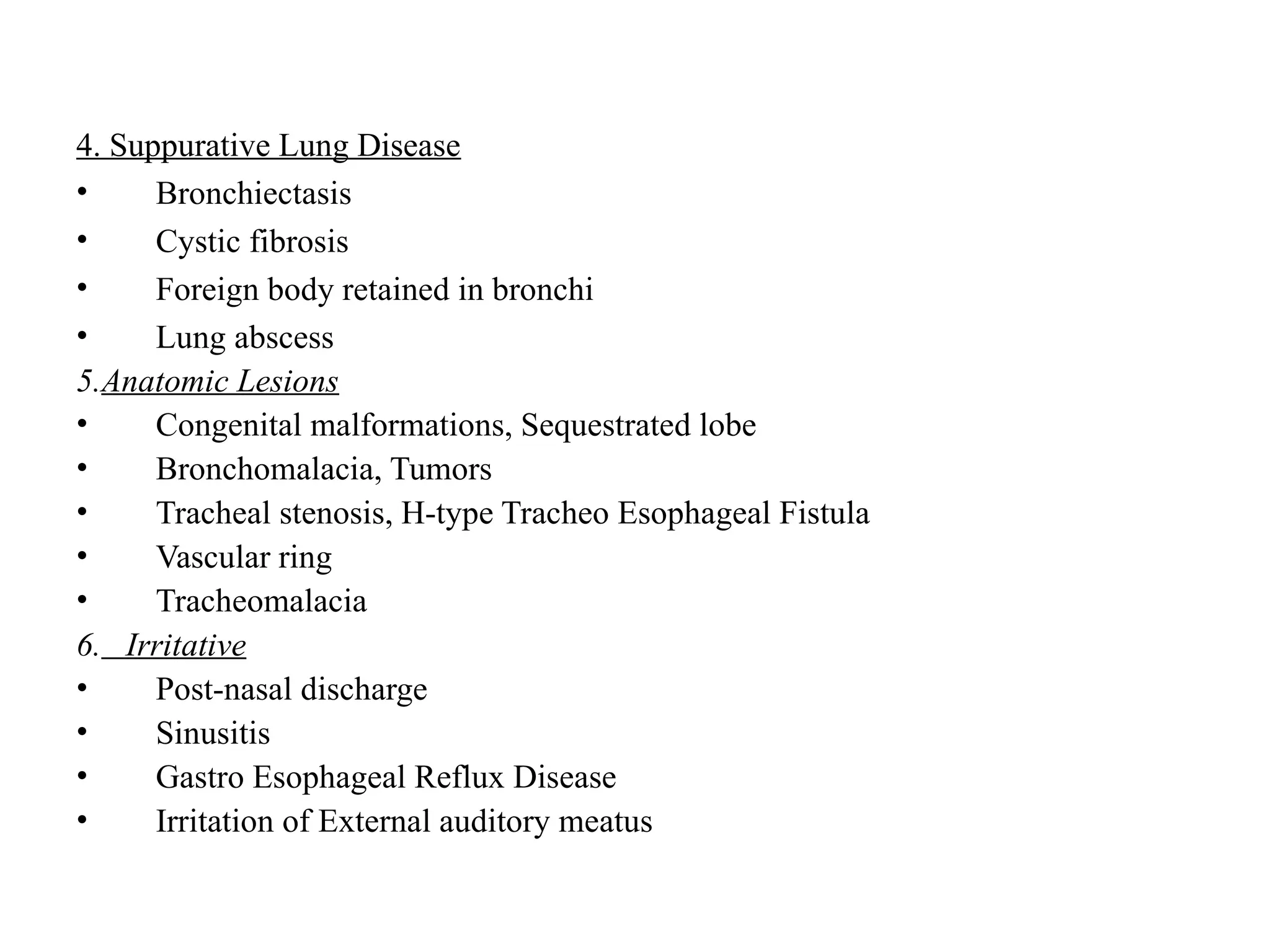
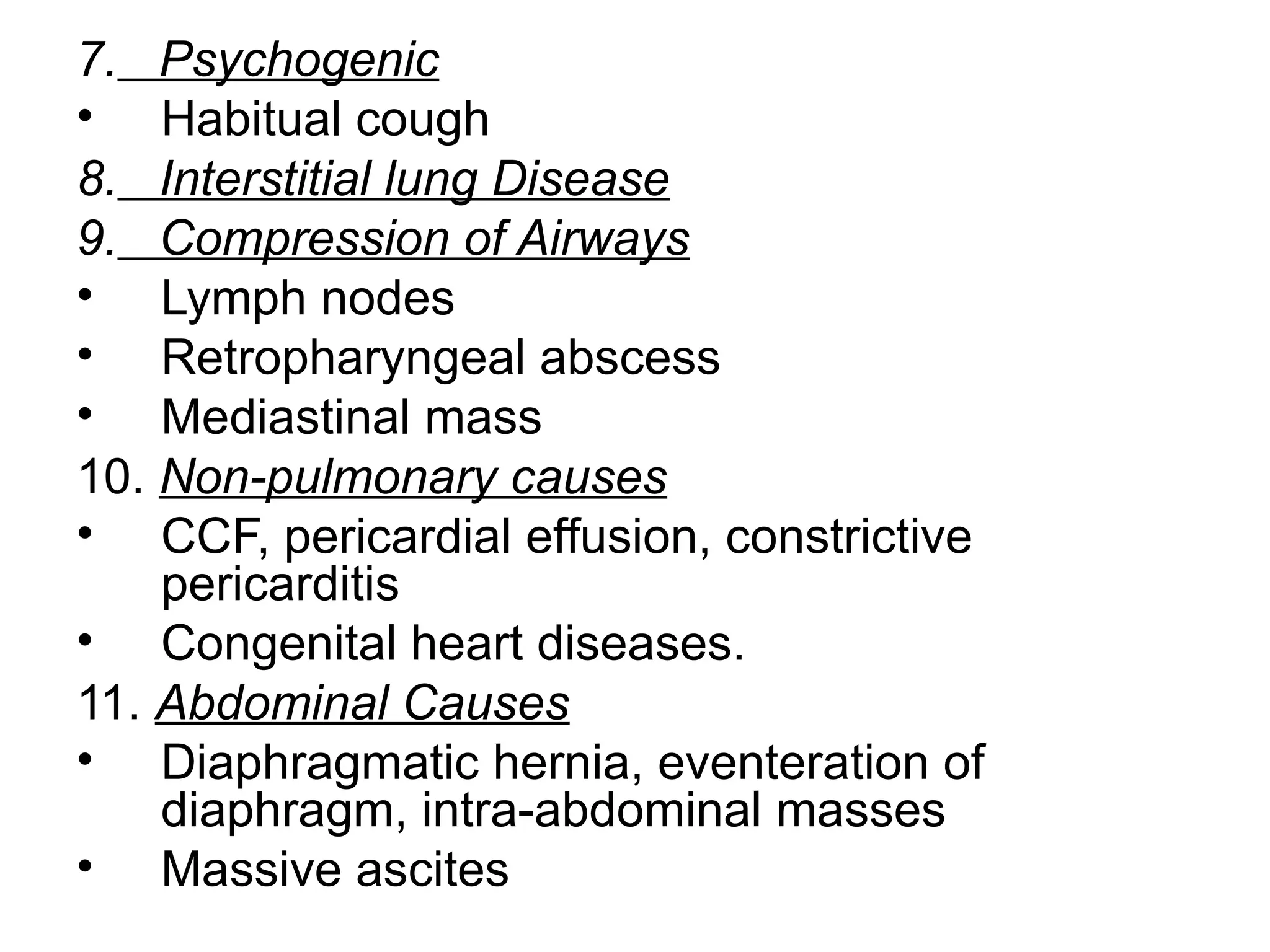
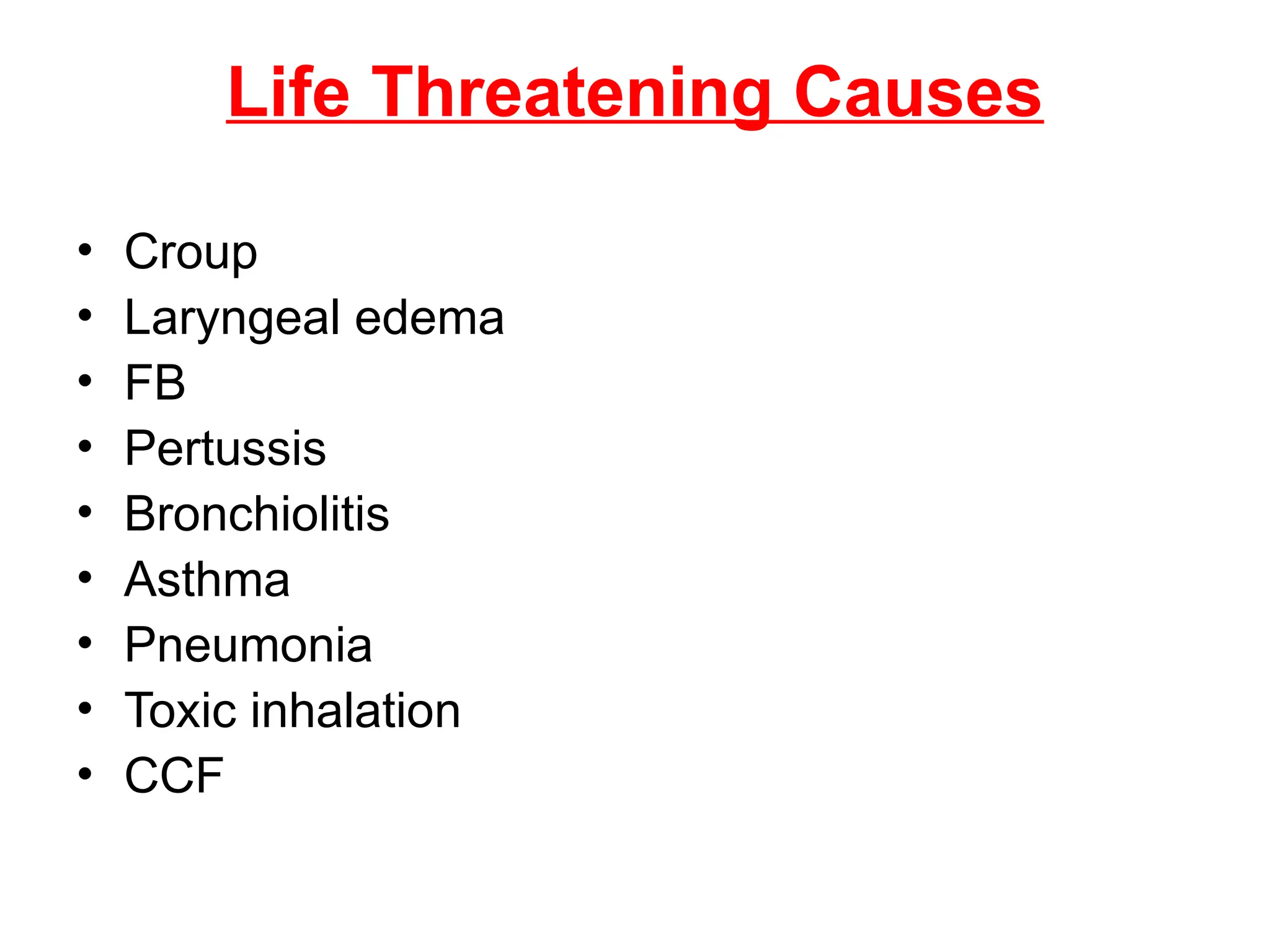
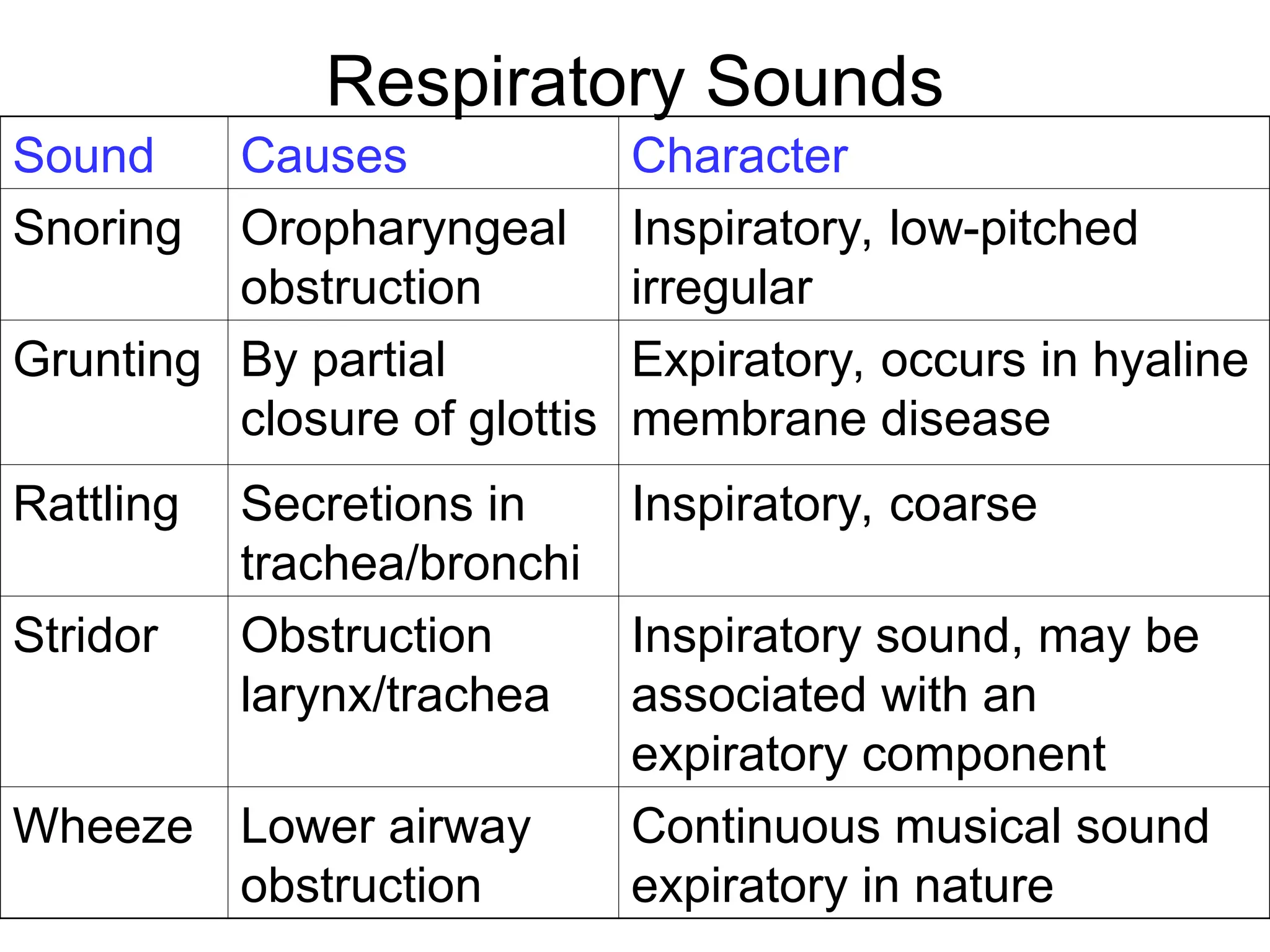
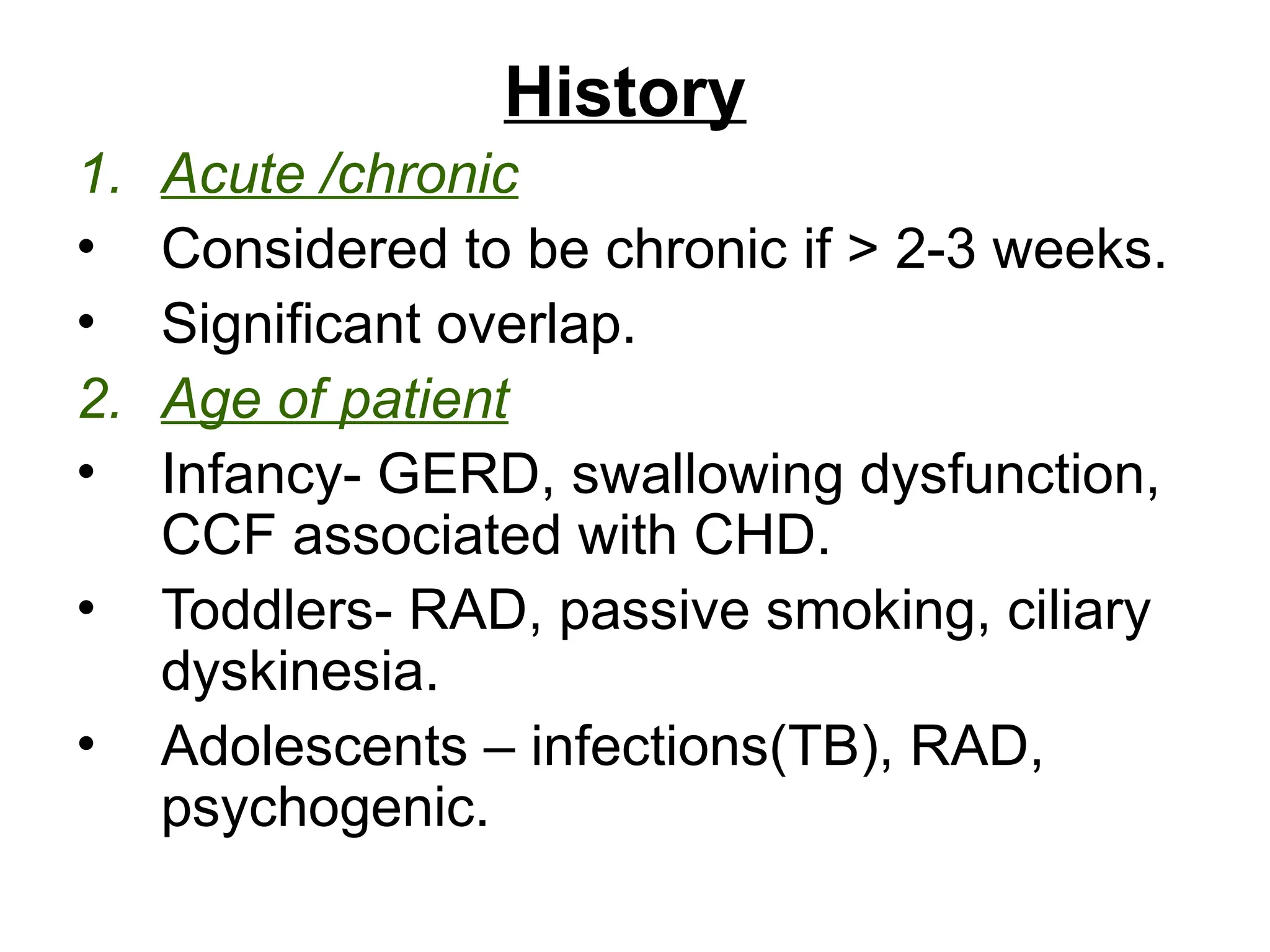
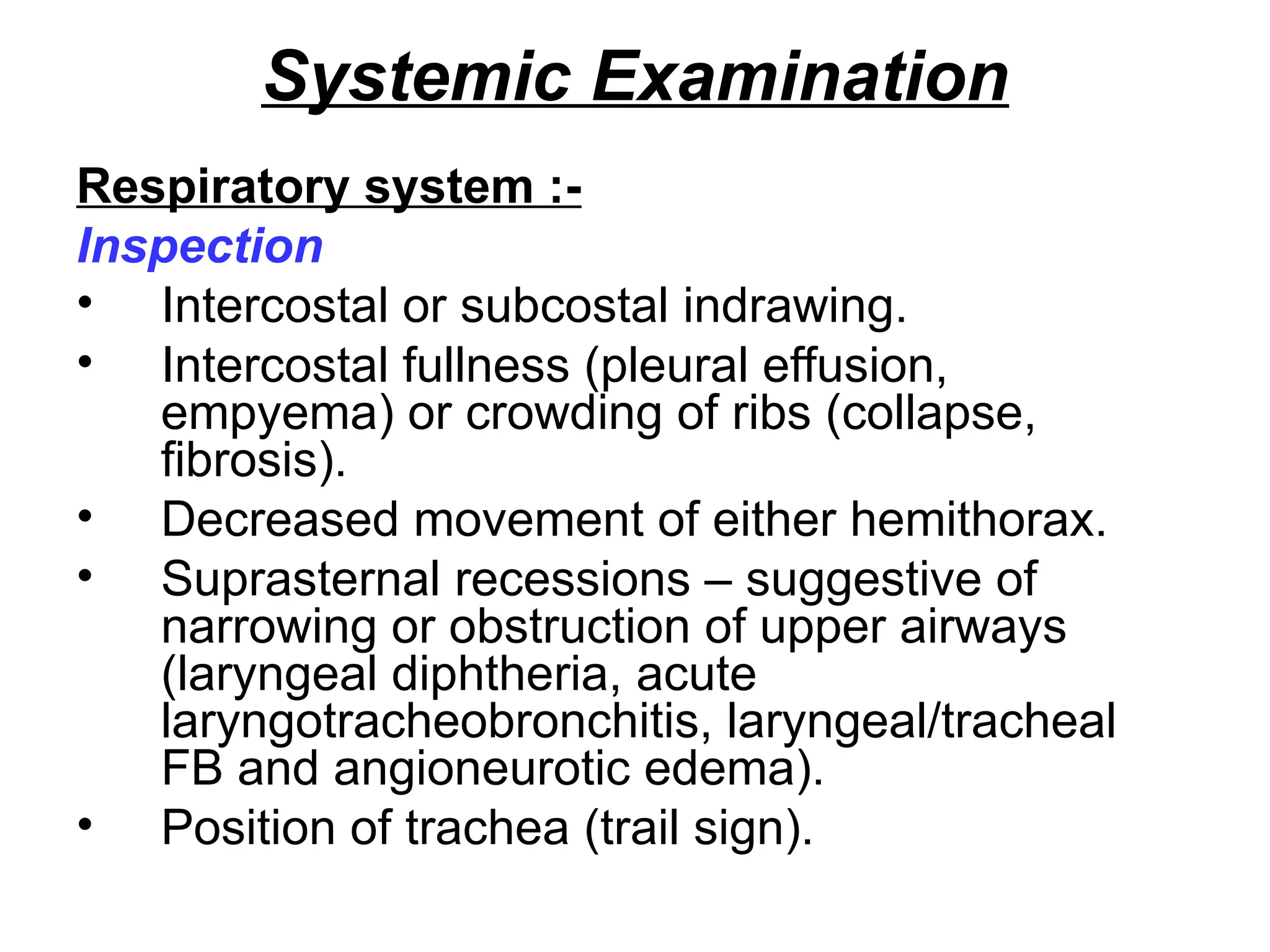
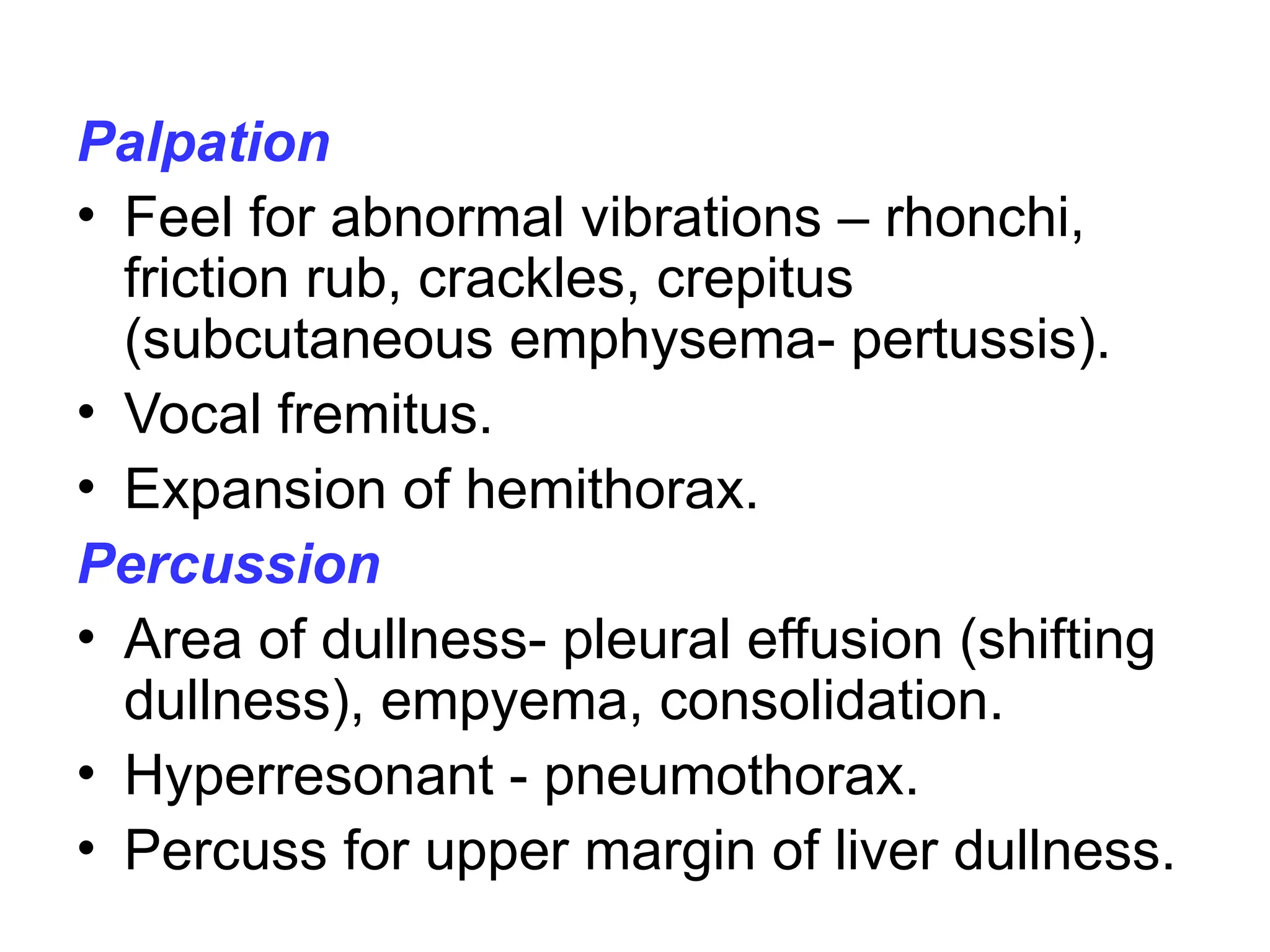
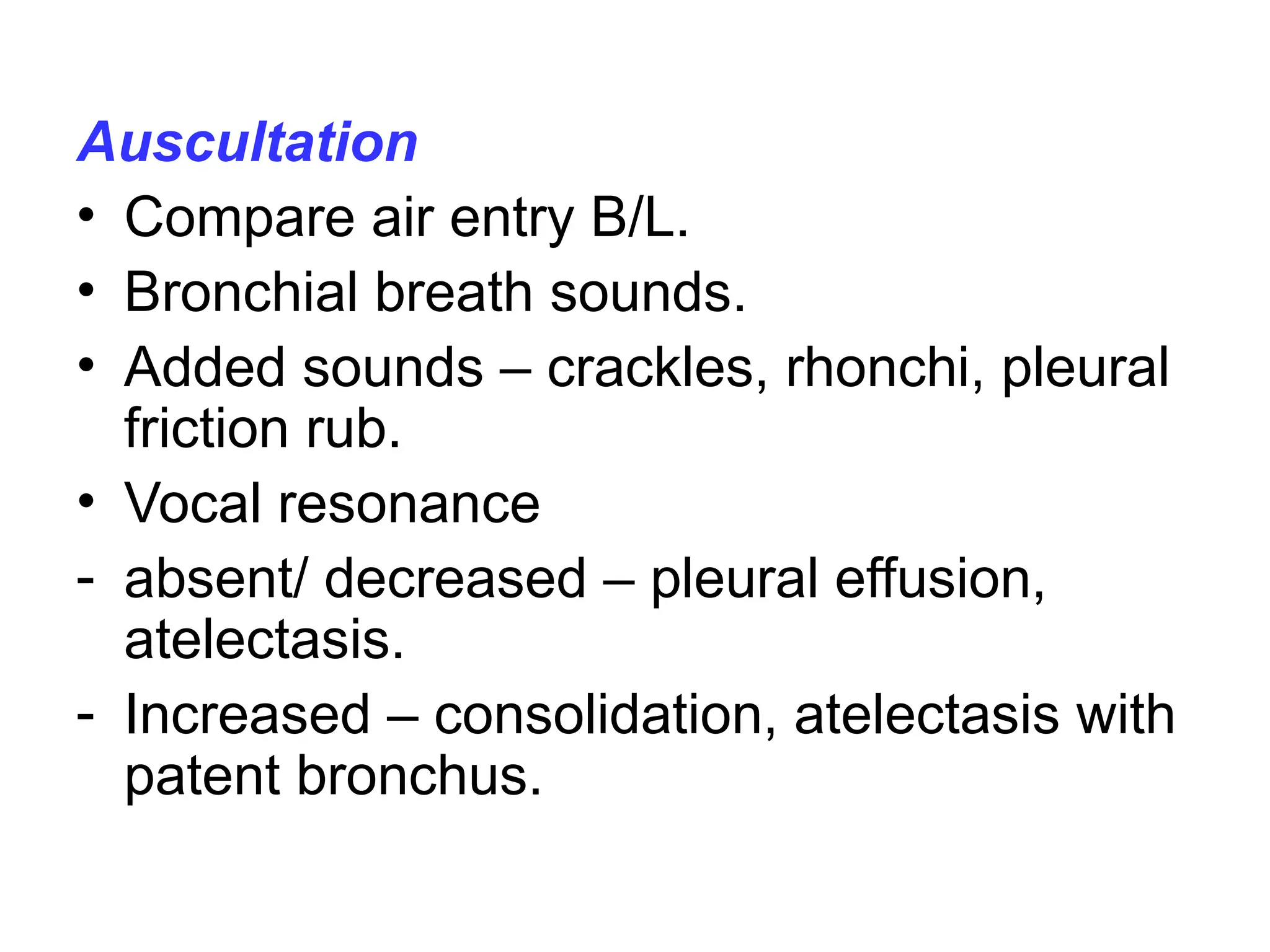
The document outlines the pathophysiology and causes of cough, detailing various respiratory disorders and other conditions leading to cough reflex stimulation. It emphasizes the importance of patient history, cough characteristics, and physical examination for diagnosis, along with investigations such as blood tests and imaging. Additionally, it highlights potential life-threatening causes and the necessity of considering non-pulmonary factors contributing to cough.