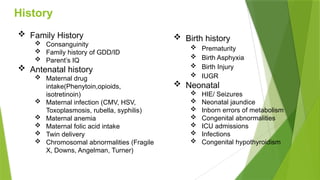
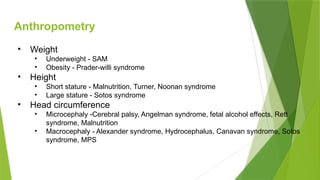
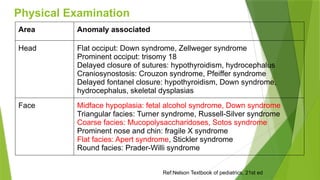
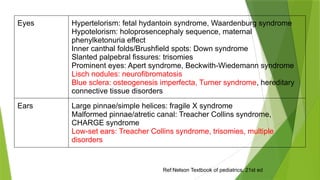
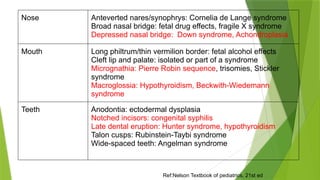
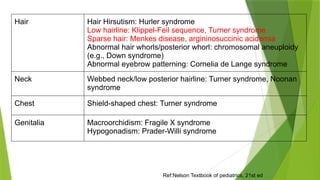
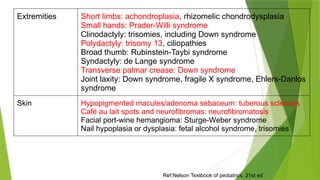
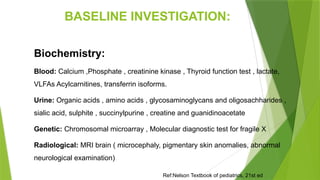
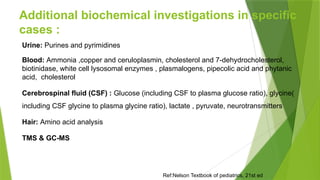
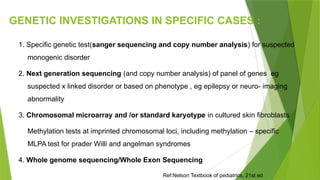
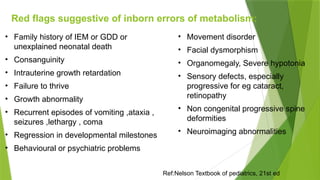
The document outlines a comprehensive approach to diagnosing children with developmental delays, highlighting the importance of taking detailed medical and family histories, and conducting thorough physical examinations. It lists various associated conditions, physical anomalies, and recommended investigations, including biochemical analyses and genetic testing. Additionally, red flags are identified for inborn errors of metabolism that should prompt further evaluation.