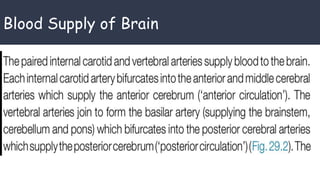
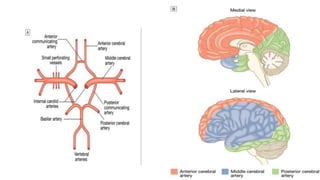
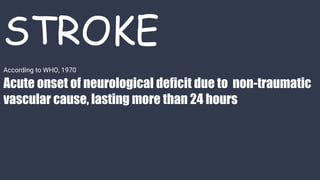
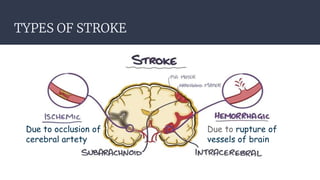
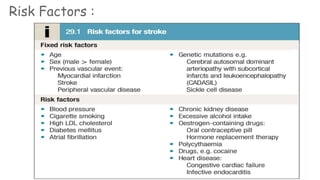
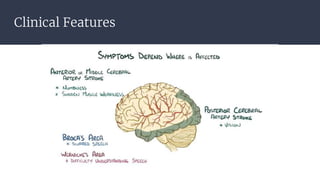
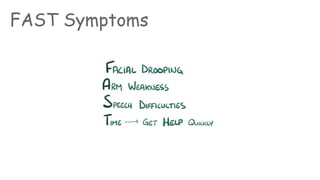
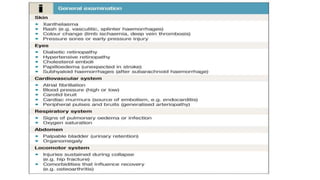
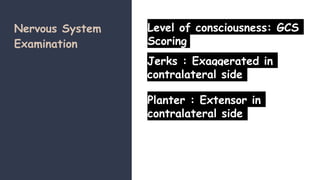
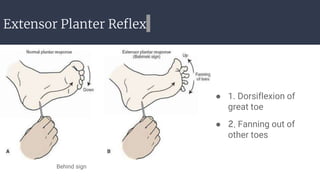
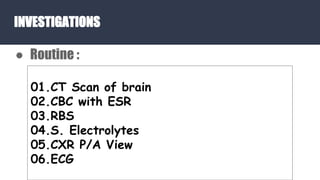
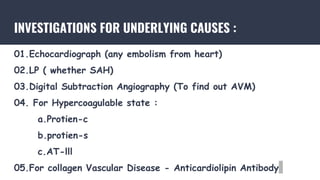
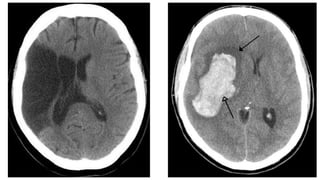
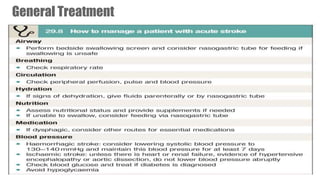
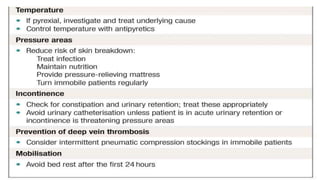
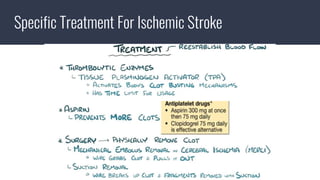
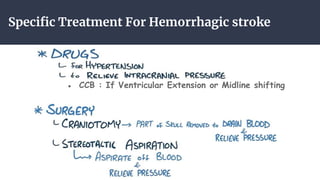
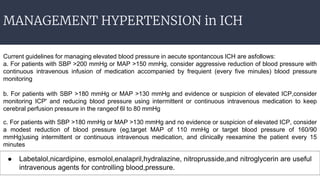
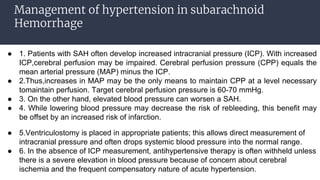
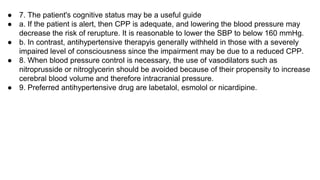
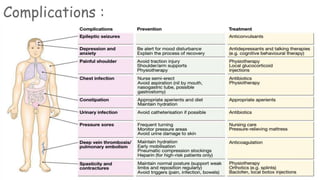
The document outlines the approach to managing stroke patients, detailing the types of strokes, associated risk factors, and key clinical features for diagnosis. It highlights the importance of CT scans and various investigations, along with general and specific treatment protocols for ischemic and hemorrhagic strokes. Furthermore, it discusses the management of hypertension in cases of intracerebral hemorrhage and subarachnoid hemorrhage, emphasizing targeted blood pressure control and monitoring intracranial pressure.