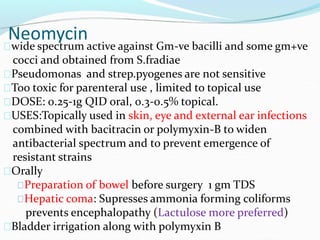
This document discusses aminoglycoside antibiotics. It defines aminoglycosides as having polybasic amino groups linked glycosidically to amino sugars. It then classifies some common aminoglycosides as streptomycin, gentamicin, kanamycin, and amikacin. The document discusses the properties, mechanisms of action, resistance, pharmacokinetics, toxicities and interactions of aminoglycosides. It provides more detailed information about specific aminoglycosides including streptomycin, gentamicin, kanamycin, tobramycin, and neomycin.