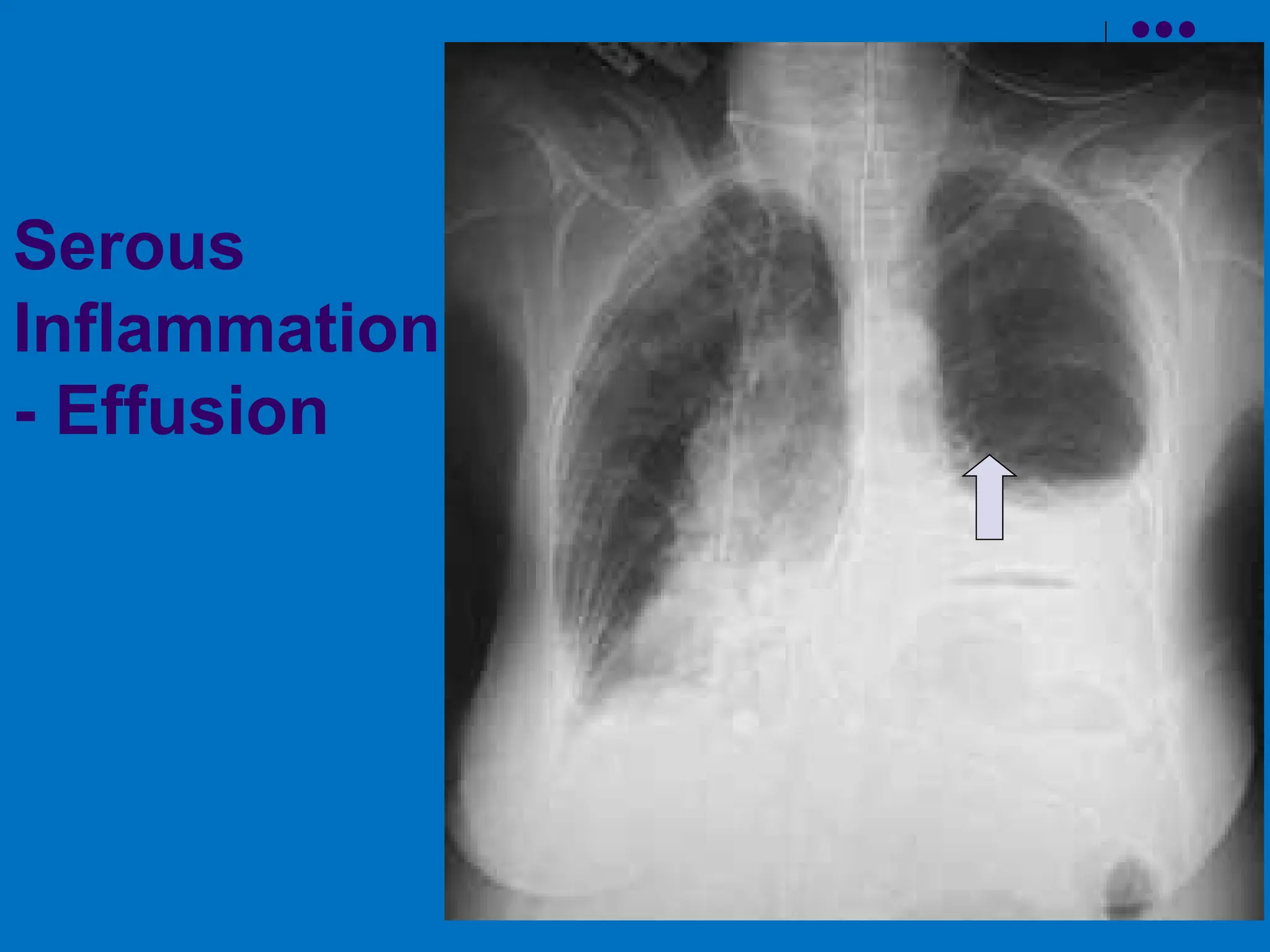
The document discusses the cellular events involved in inflammation, particularly leukocyte recruitment, activation, and the processes of margination, rolling, adhesion, and transmigration of leukocytes. It outlines various mechanisms by which leukocytes respond to injury and migrate towards chemotactic stimuli, including phagocytosis and the formation of neutrophil extracellular traps (NETs). Additionally, it covers the potential outcomes of acute inflammation, including resolution, scarring, and the development of chronic inflammation.




![ Emigration of leukocytes: margination, rolling, adhesion,
diapedesis, migration
Neutrophils predominate (6-24 hours) and replaced by
Monocytes (24-48 hours)
Upregulation of molecules
E-selectin (endothelium) - rolling, adhesion [induced by IL-1
and TNF]
P-selectin (endothelium, platelets) - rolling [present in Weibel-
Palade bodies]
L-selectin (leukocytes) - homing](https://image.slidesharecdn.com/acuteinflammation2-250110103251-4c005e1b/75/Acute-Inflammation-and-cellular-events-in-5-2048.jpg)