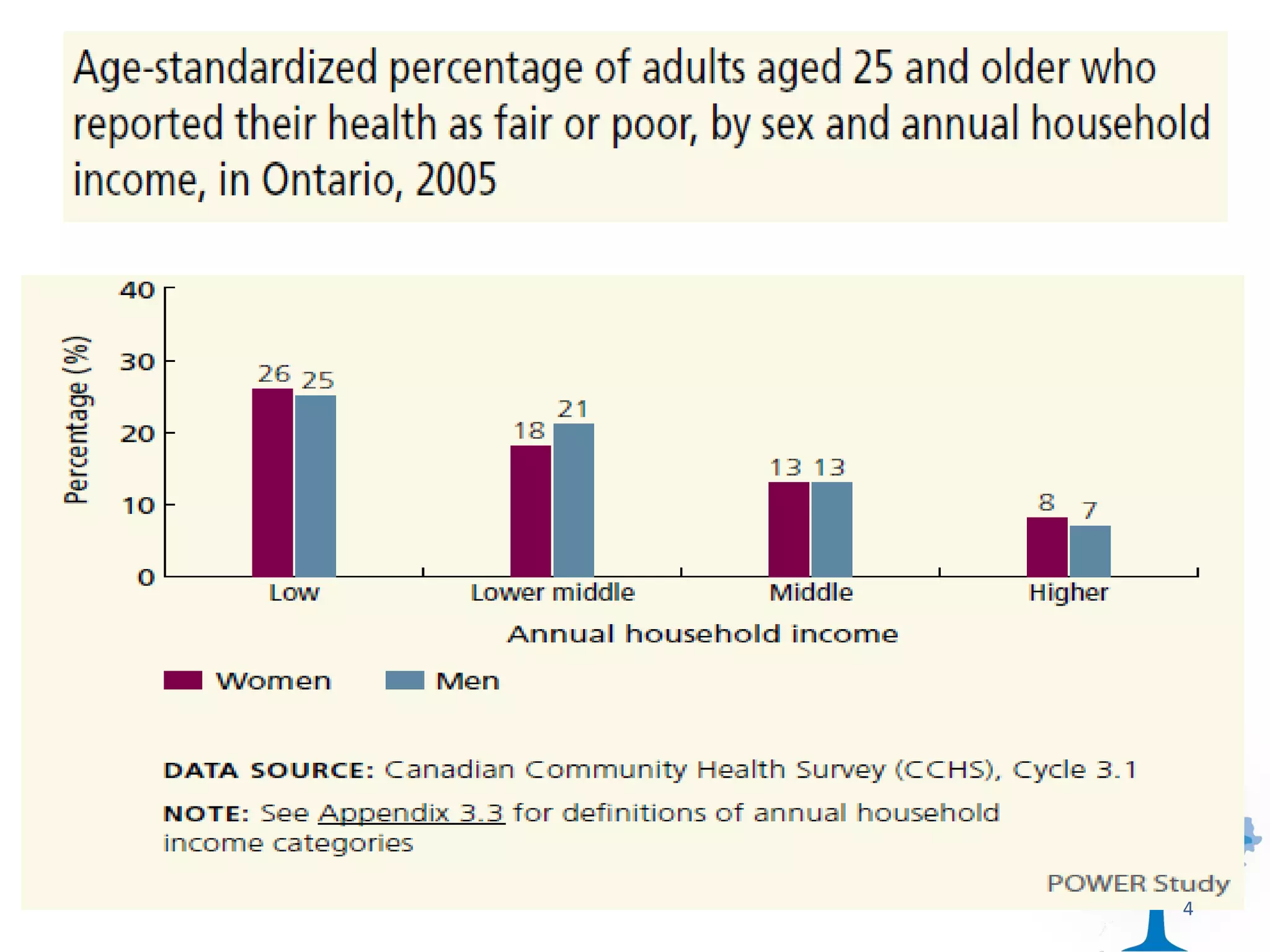
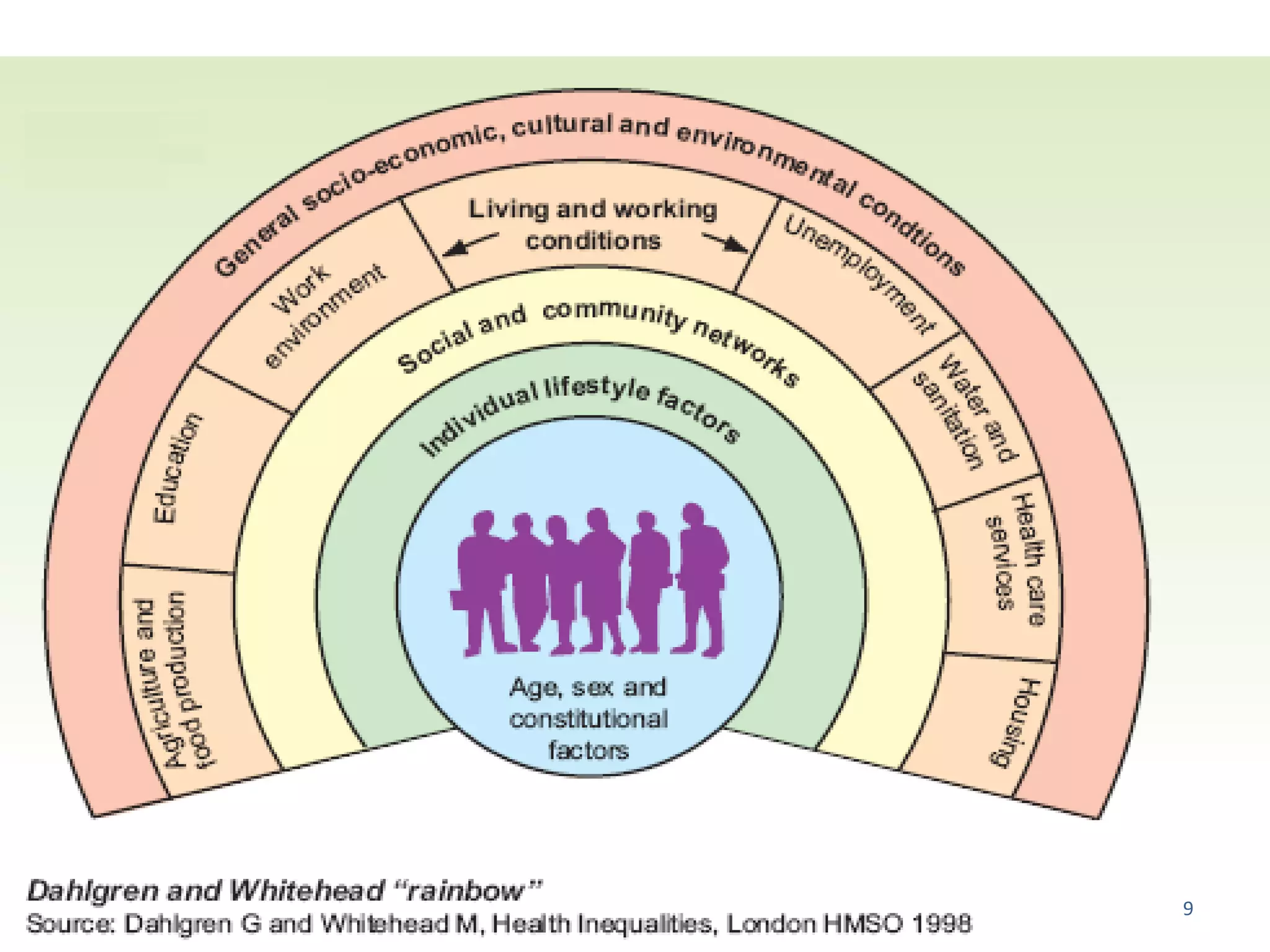
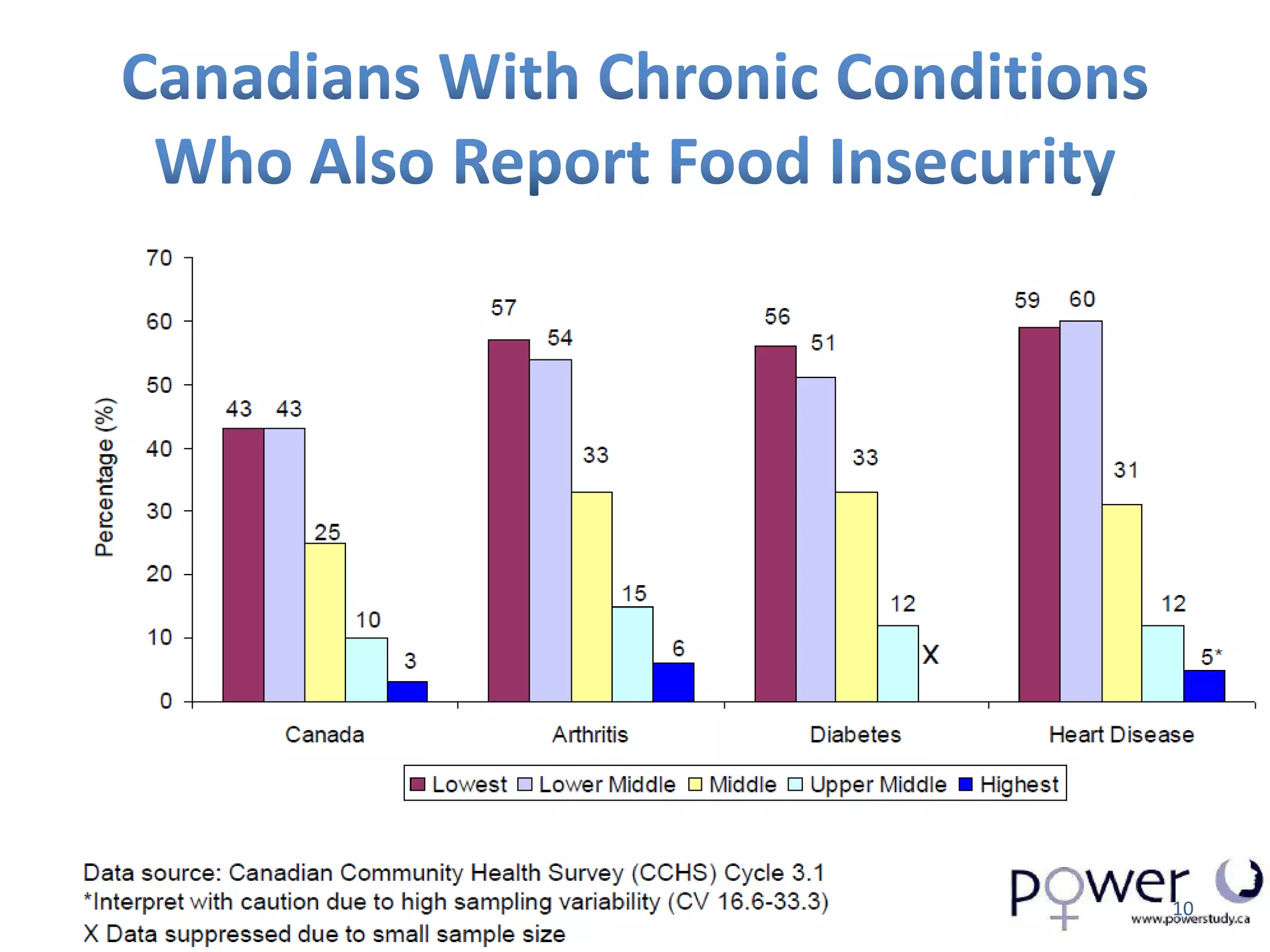
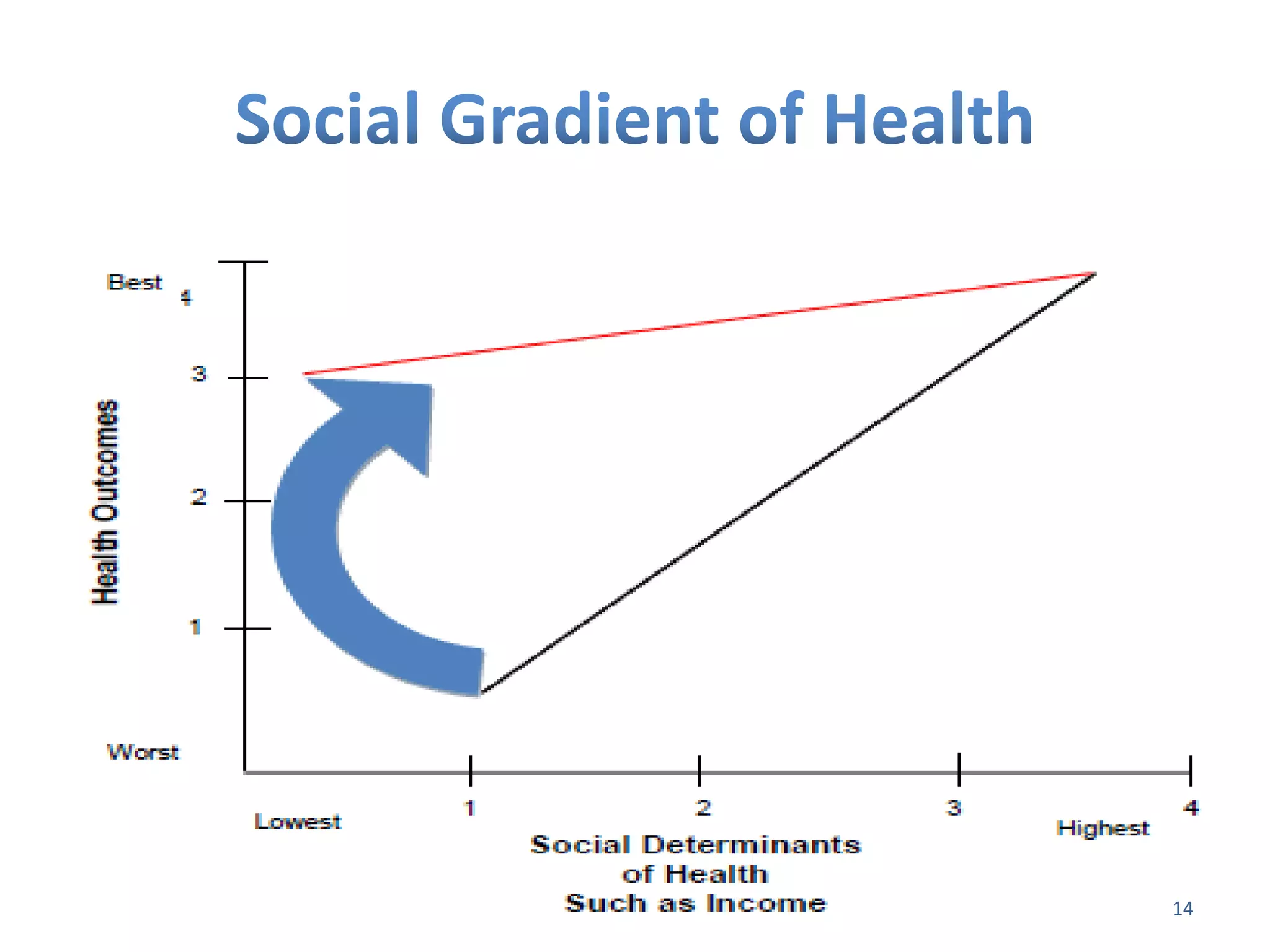
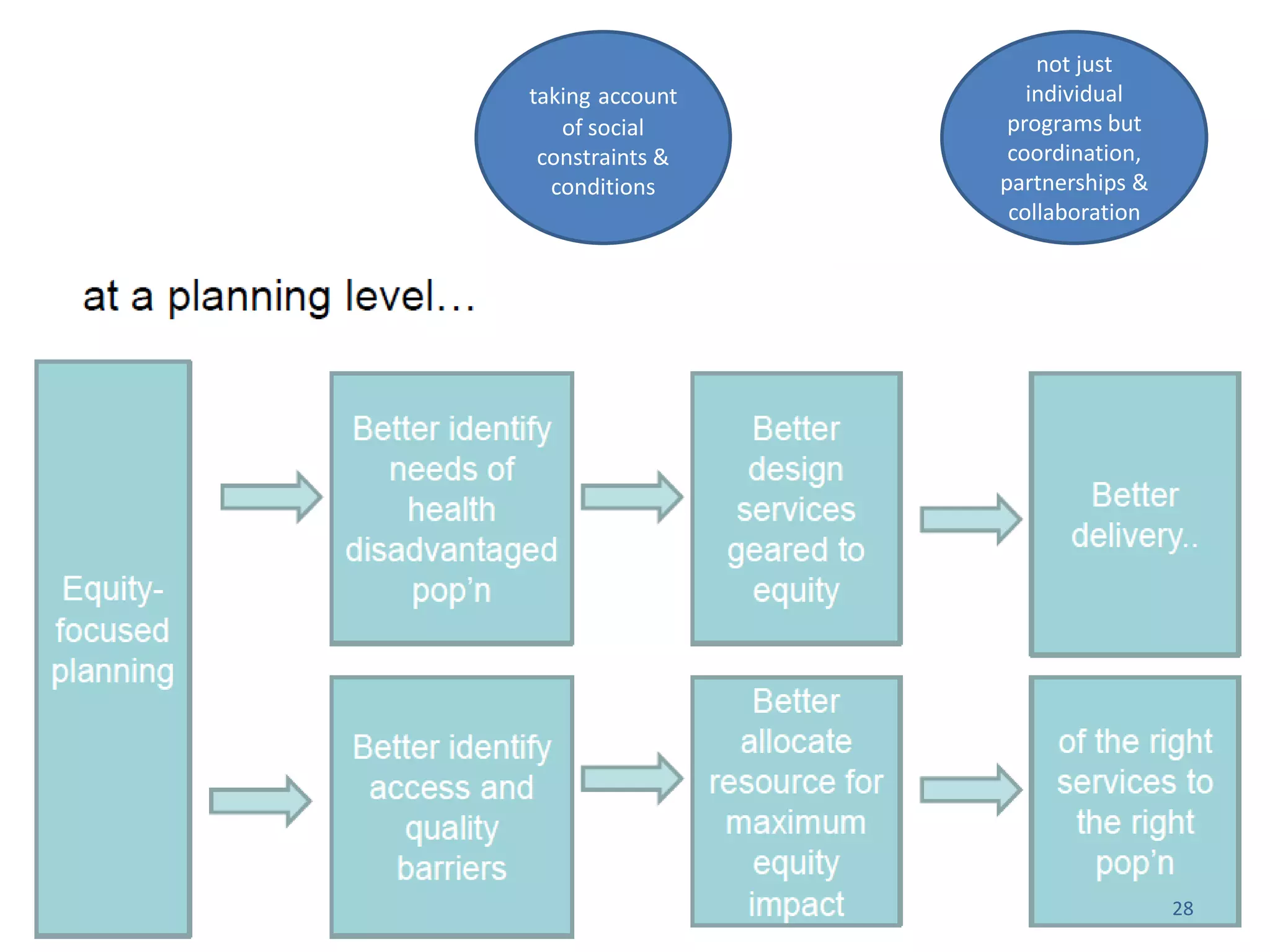
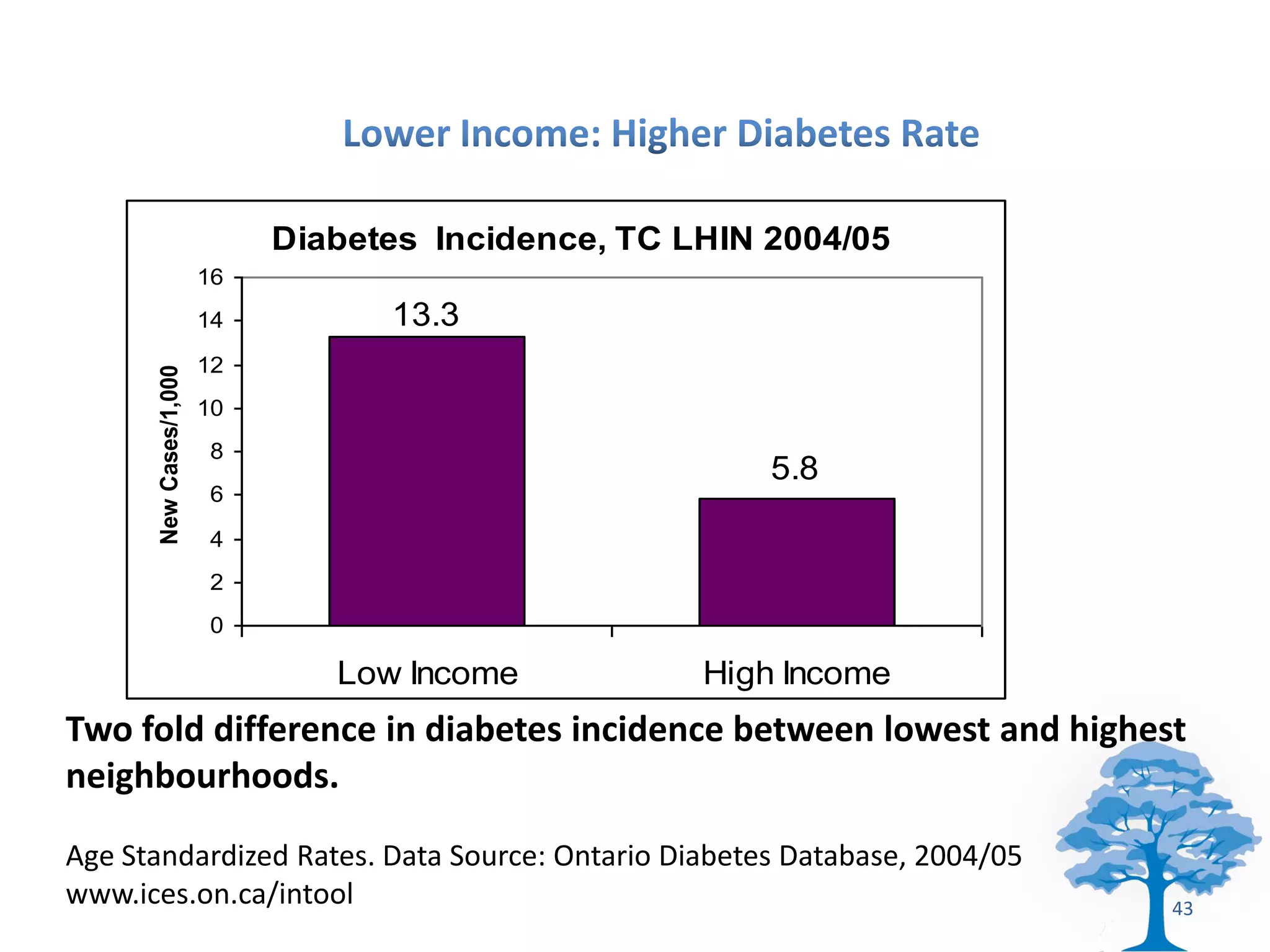
The document discusses the pervasive health disparities in Ontario, emphasizing the need for a comprehensive health equity strategy to address the systemic roots of these inequalities. It outlines the importance of equitable access to quality healthcare and the integration of social determinants of health in policy design and program interventions. The document highlights successful international examples and concludes with a call for targeted actions and collaborative efforts to close the health equity gap.