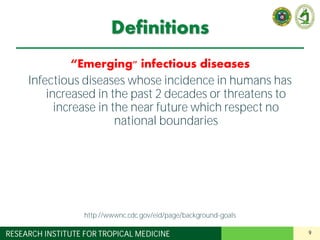
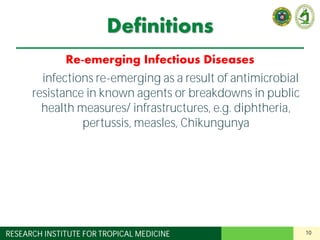
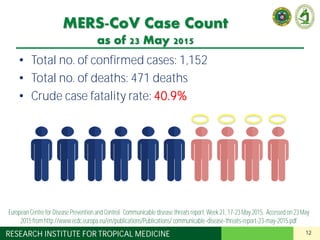
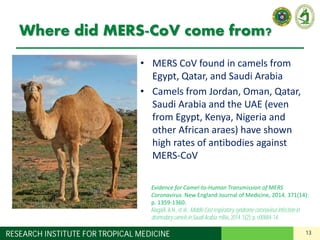
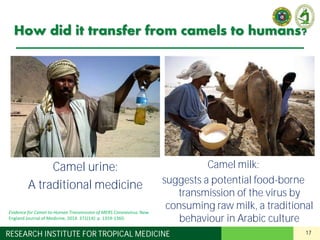
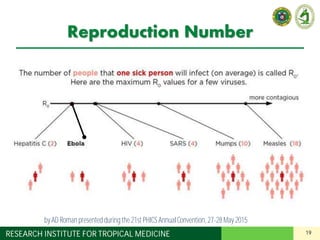
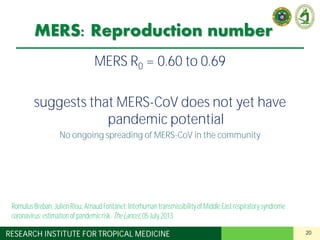
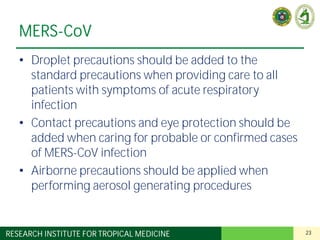
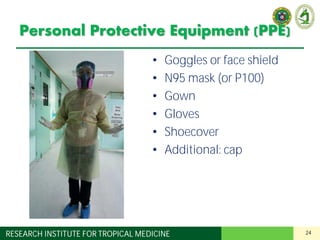
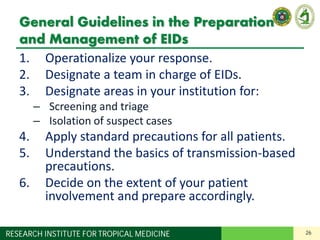
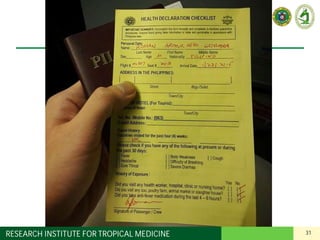
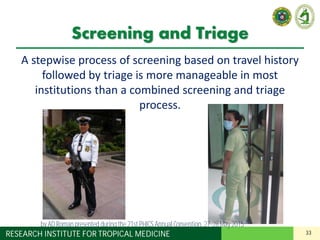
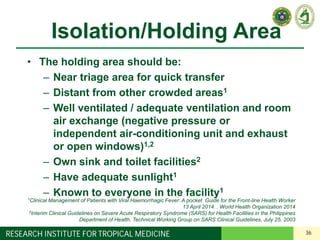
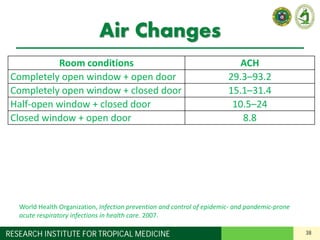
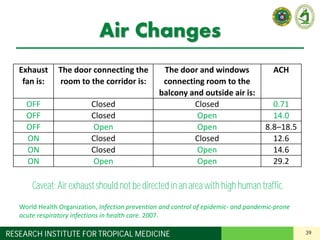
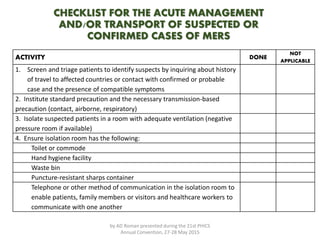
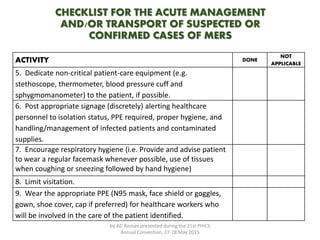
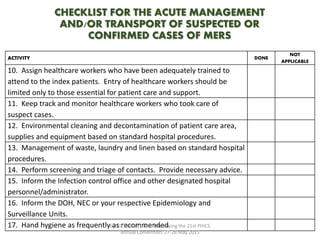
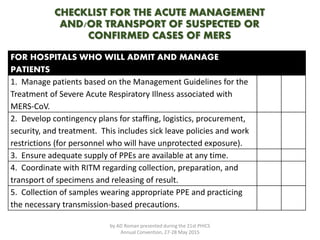
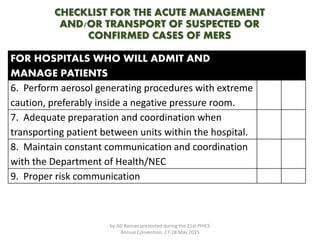
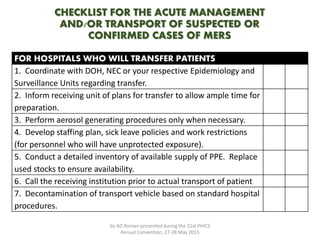
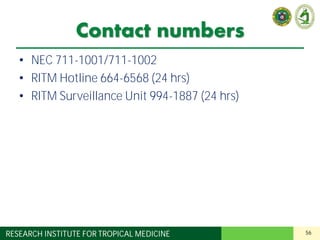
The document is a comprehensive guide on preparing for and managing emerging infectious diseases (EIDs), emphasizing the importance of operationalizing responses and establishing dedicated teams. It outlines general guidelines for hospitals, including the need for screening, triage, and isolation areas, as well as the use of personal protective equipment (PPE) for healthcare workers. Current concerns focus on MERS-CoV transmission and preventive measures for healthcare settings to ensure patient and worker safety.