This document contains a series of questions and answers related to adult reconstructive surgery of the hip and knee. It includes radiographs, diagrams, and descriptions of clinical scenarios. For one scenario, it describes radiographs of an 82-year old man with loosening of the tibial component of a total knee arthroplasty. The preferred treatment is listed as revision of the tibial component with porous metal augmentation.
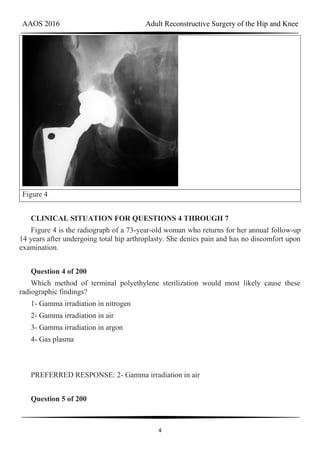
![AAOS 2016 Adult Reconstructive Surgery of the Hip and Knee
2
Video 1 for reference
For severe tibial defects (Anderson Orthopaedic Research Institute [AORI] types 2 and 3),
metaphyseal fixation is necessary to achieve construct fixation during revision TKA.
Metaphyseal fixation may be achieved with cement, structural allograft, or conical metallic
implants. The major concerns regarding structural allograft are graft resorption and mechanical
failure and technical issues related to fashioning the graft and obtaining a good host-allograft
interface. In a systematic review, porous metal cones were associated with a decreased
loosening rate in AORI 2 and 3 defects compared to structural allografts. Metallic trabecular
metal cones and metaphyseal porous coated sleeves provide a stable construct with which to
support the tibial component during revision TKA. Clinical results with these devices include
good metaphyseal fixation for severe tibial bone defects.
Question 2 of 200
Patient-specific instrumentation (PSI) reliably demonstrates which benefit over
conventional intramedullary guidance systems?
1- Lower cost
2- Improved functional outcomes
3- Better coronal alignment
4- Fewer trays
PREFERRED RESPONSE: 4- Fewer trays](https://image.slidesharecdn.com/aao2016recon-180708071603/85/Aao2016-recon-3-320.jpg)


















![AAOS 2016 Adult Reconstructive Surgery of the Hip and Knee
50
5- Anterior knee pain
6- Malalignment
PREFERRED RESPONSE: 6- Malalignment
DISCUSSION
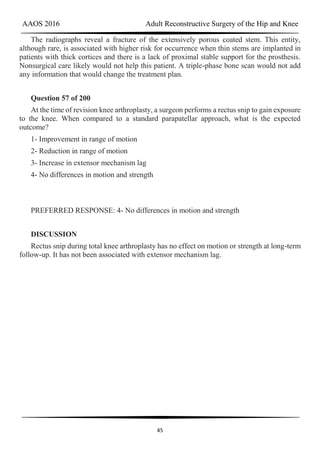
Figure 58 reveals a posttraumatic valgus deformity. Correction of valgus with lateral soft-
tissue release places tension on the peroneal nerve, resulting in an increased risk for nerve
palsy. Figures 59a (lateral view) and 59b (Merchant view) illustrate juvenile rheumatoid
arthritis with tibiofibular fusion and lateral patellar dislocation. Chronic patellar dislocation is
associated with contracture of the lateral retinacular soft tissues and increased risk for patellar
subluxation or dislocation after TKA. Extensor mechanism realignment, possibly including
tibial tubercle osteotomy and/or proximal soft-tissue realignment, may be required during
TKA to centralize the extensor mechanism. Figures 60a (anteroposterior [AP] view) and 60b
(lateral view) reveal a fused knee in full extension.
TKA after fusion is associated with multiple complications including skin necrosis,
infection, and instability. The skin is contracted because of limited knee motion and has
multiple scars (Figure 60c). Mobilization of the skin during and after knee arthroplasty can
place excess tension on the soft tissues, resulting in skin necrosis and infection. Treatment
consisting of prompt debridement and soft-tissue coverage, usually with medial gastrocnemius
muscle transposition, is required. Figure 61 shows a knee with prior tibial tubercle fixation
and marked patella infera. Shortening of the patellar ligament is associated with restricted knee
motion. This may necessitate more extensile exposure using tibial tubercle osteotomy or rectus
snip during TKA to obtain adequate surgical exposure. The inferior position of the patella can
cause impingement between the patellar component and tibial insert, resulting in anterior knee
pain. Restoring a more normal position of the patella may necessitate distal positioning of the
femoral component as well as tibial tubercle osteotomy with proximal recession of the
osteotomized tibial tubercle. Figures 62a (AP view of the distal femur) and 62b (AP view of
the proximal femur) show a posttraumatic deformity with a large retained intramedullary rod.
There is a varus distal femoral deformity that is not severe enough to necessitate extra-articular
corrective osteotomy. However, intramedullary hardware precludes use of conventional
intramedullary instrumentation, so computer navigation or patient-specific cutting guides will
be necessary to orient the bone cuts and avoid implant malalignment.
Question 63 of 200
Injury to the popliteal artery during total knee arthroplasty (TKA) is most likely when
placing a sharp retractor
1- directly posterior to the posterior cruciate ligament (PCL).](https://image.slidesharecdn.com/aao2016recon-180708071603/85/Aao2016-recon-51-320.jpg)






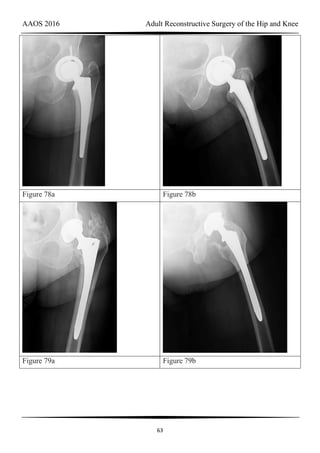




![AAOS 2016 Adult Reconstructive Surgery of the Hip and Knee
76
1- Isolated head and liner revision
2- 2-stage exchange
3- Acute hemodialysis
4- Femoral component revision
5- Acetabular component revision
6- Revision total hip (all components)
PREFERRED RESPONSE: 1- Isolated head and liner revision
Question 94 of 200
A 70-year-old man has a posterior dislocation 20 years after undergoing cementless THA
with a metal-on-polyethylene bearing. Acetabular inclination is 55 degrees with neutral
version. This is his third dislocation, and he has been treated with closed reduction 3 times
during the past month. His ESR is 42 mm/h (reference range [rr], 0-20 mm/h) and CRP level
is 16.2 mg/L (rr, 0.08-3.1 mg/L). Joint aspiration reveals a cell count of 865 cells (55%
neutrophils).
1- Isolated head and liner revision
2- 2-stage exchange
3- Acute hemodialysis
4- Femoral component revision
5- Acetabular component revision
6- Revision total hip (all components)
PREFERRED RESPONSE: 5- Acetabular component revision
DISCUSSION
Treatment options for various pathologic conditions after THA can be challenging, and
there are often multiple potential options. Question 91 involves a patient who has fractured a
modular ceramic acetabular liner, and an isolated head and liner exchange should be sufficient.
Question 92 involves a patient with markedly elevated serum metal ions and abductor
dysfunction, suggesting poor bearing function and a probable adverse local tissue reaction
(ALTR). Additionally, the acetabular component position is suboptimal, and complete](https://image.slidesharecdn.com/aao2016recon-180708071603/85/Aao2016-recon-77-320.jpg)


















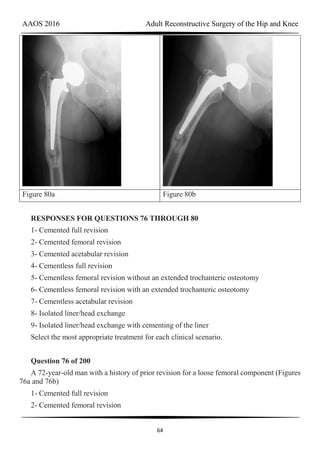
![AAOS 2016 Adult Reconstructive Surgery of the Hip and Knee
103
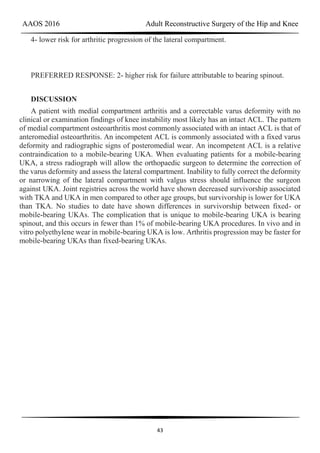
Question 124 of 200
A 56-year-old woman underwent a total knee arthroplasty 2 years ago and now has pain
and swelling. Radiographs of her knee are unremarkable. Her C-reactive protein (CRP) level
is 3.0 (reference range [rr], 0.08–3.1 mg/L), and her erythrocyte sedimentation rate (ESR) is
18 mm/h (rr, 0-20 mm/h). Aspiration of the knee reveals a white blood cell (WBC) count of
1200/mm3 with a differential of 30% neutrophils and 70% monocytes. Cultures will not be
available for several days, and the patient has not been taking antibiotics. Based on these
findings, the most appropriate next step is
1- arthrotomy, irrigation, and tibial polyethylene exchange.
2- parenteral antibiotics.
3- nonsurgical treatment without antibiotics.
4- removal of the implant and a 2-stage procedure.
PREFERRED RESPONSE: 3- nonsurgical treatment without antibiotics.
DISCUSSION
ESR and CRP level are recommended as starting points in the workup for the diagnosis or
exclusion of periprosthetic joint infection (PJI). When both the ESR and CRP findings are
within defined limits, PJI is unlikely. When both test findings are positive, PJI must be
considered and further investigation is warranted. Clinicians need to be aware of other
inflammatory conditions such as rheumatoid arthritis that can lead to elevation of
inflammatory markers.
A high likelihood of infection is noted when the knee aspirate contains more than 2500
WBCs per high-powered field (HPF) with a differential count exceeding 60% neutrophils.
Using these criteria, Mason demonstrated a sensitivity of 98% and a specificity of 95% for
infection diagnosis.
For this patient, the inflammatory markers are within normal limits. The aspiration result
is below 2500 WBC/HPF with a low percentage of neutrophils. The likelihood of infection is
remote, and further nonsurgical treatment should not include antibiotics. There is no indication
for surgery based upon the information presented.](https://image.slidesharecdn.com/aao2016recon-180708071603/85/Aao2016-recon-104-320.jpg)

![AAOS 2016 Adult Reconstructive Surgery of the Hip and Knee
107
Figure 128 is the radiograph of a 78-year-old nursing home resident who has hypertension
and peripheral vascular disease. He has developed acute severe hip pain 20 years after
undergoing a cementless total hip arthroplasty (THA) and subsequent revision for instability.
He was previously ambulatory with a walker and now can no longer ambulate. His erythrocyte
sedimentation rate is 8 mm/h (reference range [rr], 0-20 mm/h) and C-reactive protein level is
0.6 mg/L (rr, 0.08-3.1 mg/L).
Question 128 of 200
When preparing for surgery, which protocol is most appropriate?
1- Intravenous (IV) prophylaxis with a cephalosporin for 24 hours
2- IV prophylaxis with a cephalosporin for 72 hours
3- IV prophylaxis with a cephalosporin and clindamycin
4- IV prophylaxis with a cephalosporin and gentamicin
PREFERRED RESPONSE: 1- Intravenous (IV) prophylaxis with a cephalosporin for 24
hours
Question 129 of 200
The patient is treated with proximal femoral replacement and acetabular reconstruction
that includes superior augmentation and a dual-mobility revision component (Figure 129).
During surgery, a large pseudotumor that has eroded the entire abductor mechanism and
extended over the anterior acetabulum and pelvis is found. Intrasurgical blood loss is 800 cc.
Low-molecular-weight heparin is used for postsurgical deep venous thrombosis (DVT)
prophylaxis. Eight units of packed red blood cells (PRBCs) are transfused over 5 days
following surgery. Twelve days after surgery, bloody drainage is expressed from the mid
portion of the wound, and the thigh is swollen. The man is afebrile; the wound is otherwise
clean without surrounding erythema. Treatment at this point should consist of
1- irrigation and debridement with liner and head exchange.
2- negative-pressure wound therapy (wound vac).
3- antibiotic therapy with vancomycin.
4- vastus lateralis muscle transposition.
PREFERRED RESPONSE: 1- irrigation and debridement with liner and head exchange.](https://image.slidesharecdn.com/aao2016recon-180708071603/85/Aao2016-recon-108-320.jpg)






![AAOS 2016 Adult Reconstructive Surgery of the Hip and Knee
119
Figure 145a Figure 145b Figure 146
CLINICAL SITUATION FOR QUESTIONS 145 THROUGH 147
Figures 145a and 145b are the radiographs of a 56-year-old man who has had persistent
pain in his right groin since undergoing primary total hip surgery 11 months ago. His
erythrocyte sedimentation rate (ESR) is 38 mm/h (reference range [rr], 0-20 mm/h) and C-
reactive protein (CRP) level is 28 mg/L (rr, 0.08-3.1 mg/L). A hip aspiration performed while
the patient was taking antibiotics demonstrated 3200 white blood cells/µL with no growth.
Treatment should consist of
Question 145 of 200
Treatment should consist of
1- repeat hip aspiration while the patient is not taking antibiotics.
2- iliopsoas injection under fluoroscopy.
3- acetabular revision.
4- irrigation and debridement with a polyethylene liner exchange.
PREFERRED RESPONSE: 1- repeat hip aspiration while the patient is not taking
antibiotics.](https://image.slidesharecdn.com/aao2016recon-180708071603/85/Aao2016-recon-120-320.jpg)











![AAOS 2016 Adult Reconstructive Surgery of the Hip and Knee
141
Figure 174a Figure 174b
Question 174 of 200
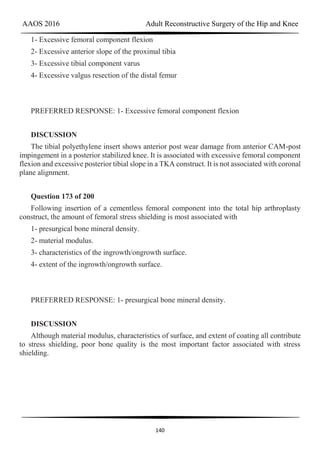
Figures 174a and 174b are the radiograph and clinical photograph of a 64-year-old obese
woman (body mass index [BMI] of 48) who has controlled diabetes and hypertension. She has
failed nonsurgical treatment and a weight loss program. She is considering total knee
arthroplasty (TKA). What is the most significant postsurgical risk for this patient?
1- Dissatisfaction after TKA
2- Periprosthetic infection and wound complications
3- Implant loosening
4- Thromboembolic disease
PREFERRED RESPONSE: 2- Periprosthetic infection and wound complications
DISCUSSION
The literature has demonstrated increased risk for complications among obese patients
undergoing TKA (10%-30%). An evaluation of TKA among obese patients revealed 3- to 9-
fold higher incidence of wound complications and deep-seated infection. Belmont and
associates demonstrated that patients with a BMI higher than 40 are at higher risk for overall
complications than patients with a BMI lower than 25, with a particularly high risk for
developing local wound complications and infection. An increased risk for thromboembolic
complications was not shown among obese patients undergoing TKA. Patient-reported
outcome scores among obese patients undergoing TKA are equivalent to those of nonobese](https://image.slidesharecdn.com/aao2016recon-180708071603/85/Aao2016-recon-142-320.jpg)













![AAOS 2016 Adult Reconstructive Surgery of the Hip and Knee
160
PREFERRED RESPONSE: 1- Pseudotumor from a local reaction to metal debris from the
bearing surface
DISCUSSION
This patient likely has a soft-tissue reaction (pseudotumor) related to metal-on-metal
articulation. Although the components are well positioned, patient gender and small head size
are both known risk factors for failure of hip resurfacing arthroplasties. Metal ion levels are
elevated but are not always markedly increased in the setting of a problematic metal-on-metal
articulation. The patient should have a metal artifact reduction sequence MR imaging study to
confirm the presence of a pseudotumor. Chronic infection is very unlikely in the setting of
normal ESR and CRP findings. Impingement and lumbar disk disease would not explain the
swelling around the hip.
45
Figure 199
Question 199 of 200
Figure 199 is the clinical photograph of a 68-year-old man with a history of atrial
fibrillation who was treated with warfarin. Nine days after undergoing elective total hip
arthroplasty, he has a swollen left thigh. His wound remains dry and he is afebrile. His
erythrocyte sedimentation rate (ESR) is 25 mm/h (reference range [rr], 0-20 mm/h) and C-
reactive protein (CRP) level is 6.1 mg/L (rr, 0.08-3.1 mg/L). Aspiration reveals 3246 white](https://image.slidesharecdn.com/aao2016recon-180708071603/85/Aao2016-recon-161-320.jpg)